An Anesthesiologist's Perspective on the History of Basic Airway
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Importance of Validation Risk Prediction Tools
Art: toc Input-citi 22:40 12/2/7 12؍balt6/z7i-anesth/z7i-anesth/z7i00812/contents panickes S ON THE COVER: David Mackey, M.D., has organized a fascinating series of commentaries by national leaders In this issue of ANESTHESIOLOGY, two original research articles and three editorial views examine in the construction and use of clinical data registries by regulatory agencies and physician the use of data in clinical decision making. practices, the first two of which appear in this month’s issue: ● Kheterpal et al.: Impact of a Novel Multiparameter Decision Support System on Intraoperative ● Mackey: Can We Finally Conquer the Problem of Medical Quality? The Systems-based Processes of Care and Postoperative Outcomes, p. 272 Opportunities of Data Registries and Medical Teamwork, p. 225 ● Liu et al.: Defining the Intrinsic Cardiac Risks of Operations to Improve Preoperative Cardiac ● Jain et al.: A Public-Private Strategy to Advance the Use of Clinical Registries, p. 227 Risk Assessments, p. 283 Downloaded from http://pubs.asahq.org/anesthesiology/article-pdf/128/2/A1/364553/20180200_0-00001.pdf by guest on 01 October 2021 ● Sessler: Decision Support Alerts: Importance of Validation, p. 241 ● Glance et al.: Risk Prediction Tools: The Need for Greater Transparency, p. 244 ● Javitt: Regulatory Landscape for Clinical Decision Support Technology, p. 247 ᭛ THIS MONTH IN ANESTHESIOLOGY 9A ᭛◆ THISEDITORIAL MONTH VIEWS IN ANESTHESIOLOGY 1A . Can We Finally Conquer the Problem of Medical Quality? The Systems-based ◼ SCIENCE, MEDICINE, AND THE ANESTHESIOLOGIST 15A Opportunities of Data Registries and Medical Teamwork 225 David C. Mackey ◼ INFOGRAPHICS IN ANESTHESIOLOGY 19A . A Public-Private Strategy to Advance the Use of Clinical Registries 227 Sachin H. -
RN to EMT-Basic Transition Course
State of Wisconsin Registered Nurse to EMT-Basic Transition Course November 2010 Wisconsin EMS Section State of Wisconsin RN to EMT-Basic Transition Course TABLE OF CONTENTS Introduction .....................................................................................................iv List of Appendices...........................................................................................vi Module 1 – Preparatory 1-1 Introduction to Emergency Care .................................................. 1-1 1-2 Well-Being of the EMT Basic ....................................................... 1-6 1-3 Medical/Legal and Ethical Issues............................................... 1-12 1-5 Lifting and Moving Patients........................................................ 1-16 1-6 Evaluation .................................................................................. 1-25 Module 2 - Patient Assessment 2-1 Scene Size-up ............................................................................. 2-1 2-2 Initial Assessment........................................................................ 2-6 2-3 Baseline Vital Signs, SAMPLE History and the Use of Pulse Oximetry .......................................................................... 2-11 2-4 Focused History and Physical Exam: Trauma ........................... 2-16 2-5 Focused History and Physical Exam: Medical ........................... 2-22 2-6 Detailed Physical Exam ............................................................. 2-27 2-7 On-Going Assessment.............................................................. -
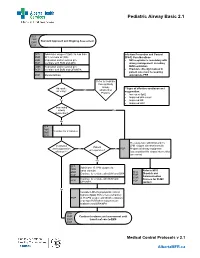
Pediatric Airway Basic 2.1
Pediatric Airway Basic 2.1 SFA FMR Standard Approach and Ongoing Assessment EMR PCP SFA Administer oxygen if SpO2 Is less than Infection Prevention and Control FMR 94% on room air (RA) (IP&C) Considerations EMR Reposition and/or suction prn • N95 respirator is mandatory with PCP Ventilate with BVM and OPA airway management, including EMR Reposition and/or suction prn BVM ventilation PCP Ventilate with BVM and OPA/NPA • Providers directly involved in patient care must be wearing PCP Monitor EtCO2 appropriate PPE Refer to Pediatric Foreign Body Airway Adequate **Signs of effective ventilation and No Obstruction air entry? oxygenation: Protocol • Increased Sp02 • Improved skin colour Yes • Improved HR • Improved LOC Impending airway Yes obstruction? No SFA FMR Ventilate for 2 minutes EMR PCP Pre-oxygenate with NRB and 15 Ventilation LPM oxygen via nasal cannula Patient and oxygenation No No PCP Prepare all airway equipment unresponsive? effective?** Assess patient for airway intervention (see notes) Yes SFA Administer 15 LPM oxygen via FMR nasal cannula Refer to MFR EMR SFA Continue to ventilate with BVM and OPA Dispatch and PCP FMR Communication EMR Continue to ventilate with BVM and Process for OLMC PCP PCP OPA/NPA contact Yes Consider LMA if symptomatic critical hypoxia (SpO2 85% or less) refractory PCP to 15 LPM oxygen with BVM ventilation (2-person BVM when resources are available) and OPA/NPA SFA FMR Continue treatment and assessment until EMR transfer of care to EMS PCP Medical Control Protocols v 2.1 AlbertaMFR.ca Pediatric Airway Basic 2.1 Definition Basic airway management is known to improve patient survival rates in the prehospital field. -

Airway Management and Ventilation: 1 W4444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444
Airway: 2 Airway Management and Ventilation: 1 W4444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444 UNIT TERMINAL OBJECTIVE 2-1 At the completion of this unit, the EMT-Intermediate student will be able to establish and/ or maintain a patent airway, oxygenate, and ventilate a patient. COGNITIVE OBJECTIVES At the completion of this unit, the EMT-Intermediate student will be able to: 2-1.1 Explain the primary objective of airway maintenance. (C-1) 2-1.2 Identify commonly neglected prehospital skills related to airway. (C-1) 2-1.3 Identify the anatomy and functions of the upper airway. (C-1) 2-1.4 Describe the anatomy and functions of the lower airway. (C-1) 2-1.5 Explain the differences between adult and pediatric airway anatomy. (C-1) 2-1.6 Define normal tidal volumes for the adult, child, and infant. (C-1) 2-1.7 Define atelectasis. (C-1) 2-1.8 Define FiO2. (C-1) 2-1.9 Explain the relationship between pulmonary circulation and respiration. (C-3) 2-1.10 List factors which cause decreased oxygen concentrations in the blood. (C-1) 2-1.11 List the factors which increase and decrease carbon dioxide production in the body. (C 2-1.12 Describe the measurement of oxygen in the blood. (C-1) 2-1.13 Describe the measurement of carbon dioxide in the blood. (C-1) 2-1.14 List the concentration of gases which comprise atmospheric air. (C-1) 2-1.15 List the factors which affect respiratory rate and depth. (C-1) 2-1.16 Describe the voluntary and involuntary regulation of respiration. -

An Anesthesiologist's Perspective on the History of Basic Airway Management
Anesthesiology ALN SPECIAL ARTICLE ANET anet ABSTRACT aln This fourth and last installment of my history of basic airway management dis- cusses the current (i.e., “modern”) era of anesthesia and resuscitation, from 1960 to the present. These years were notable for the implementation of inter- ALN An Anesthesiologist’s mittent positive pressure ventilation inside and outside the operating room. Basic airway management in cardiopulmonary resuscitation (i.e., expired air Perspective on the ventilation) was de-emphasized, as the “A-B-C” (airway-breathing-circula- ALN tion) protocol was replaced with the “C-A-B” (circulation-airway-breathing) History of Basic Airway intervention sequence. Basic airway management in the operating room 0003-3022 (i.e., face-mask ventilation) lost its predominant position to advanced airway Management management, as balanced anesthesia replaced inhalation anesthesia. The one-hand, generic face-mask ventilation technique was inherited from the 1528-1175 The “Modern” Era, 1960 to Present progressive era. In the new context of providing intermittent positive pres- sure ventilation, the generic technique generated an underpowered grip with Lippincott Williams & WilkinsHagerstown, MD Adrian A. Matioc, M.D. a less effective seal and an unspecified airway maneuver. The significant advancement that had been made in understanding the pathophysiology of ANESTHESIOLOGY 2019; 130:00–00 upper airway obstruction was thus poorly translated into practice. In contrast 10.1097/ALN.0000000000002646 to consistent progress in advanced airway management, progress in basic airway techniques and devices stagnated. “Anesthetists who have not tried this two-handed ANESTHESIOLOGY 2019; 130:00–00 hyperextension manipulation will be surprised to observe the combined effects of simultaneously Special Article pushing the vertex of the head backward and pulling The generic one-hand face-mask ventilation inher- upward on the symphysis of the mandible.” ited from the progressive era (i.e., the “E-C” technique) 2019 Editorial. -

Basic Airway Management & Decision Making
Roberts: Clinical Procedures in Emergency Medicine, 5th ed. CHAPTER 3 – Basic Airway Management and Decision-Making Robert F. Reardon, Phillip E. Mason, Joseph E. Clinton Over the last few decades, several important changes have occurred in emergency airway management. Bag-mask ventilation has been supplemented by intermediate, or backup, ventilation devices like the laryngeal mask airway (LMA), the Combitube, and the laryngeal tube. These have become important devices for the initial resuscitation of apneic patients and for rescue ventilation when intubation fails.[1] Noninvasive positive-pressure ventilation (NPPV) is now used in place of tracheal intubation in some critically ill patients. Despite these advances, basic techniques such as opening the airway, oxygenation, and bag-mask ventilation remain the cornerstones of good emergency airway management. [2] [3] Airway maintenance without endotracheal intubation is one of the most important emergency [4] airway management techniques to keep patients alive until a definitive airway can be established. This chapter describes basic airway skills including opening the airway, O2 therapy, NPPV, bag-mask ventilation, and intermediate ventilation devices. Because of the complexity of these skills and decisions, providers should develop a simple, organized approach to emergency airway management, being cognizant that when a specific intervention has failed, it is time to move rapidly to a different approach. Developing a simple preconceived algorithm that employs proven techniques and is applicable to a broad range of clinical scenarios will help providers manage difficult, anxiety-provoking emergency airways. THE CHALLENGE OF EMERGENCY AIRWAY MANAGEMENT Although other specialists are sometimes available, most emergency airways are managed by emergency clinicians.[5] Airway management in the emergency department (ED) is much different from airway management in the controlled setting of the operating room. -

Airway Management
AIRWAY MANAGEMENT Angkana Lurngnateetape, MD. Department of Anesthesiology Siriraj Hospital Perhaps the most important responsibility of the anesthesiologist is “management of the patient’s airway” Miller RD’s Anesthesia 2000 Barash PG, Cullen BF, Stoelting RK’s Clinical Anesthesia 2001 What should we know about “airway management”? ● Airway anatomy and function ● Evaluation of airway ● Clinical management of the airway - Maintenance and ventilation - Intubation and extubation - Difficult airway management Airway anatomy The term “airway” refers to the upper airway, consisting of ● Nasal and oral cavities ● Pharynx ● Larynx ● Trachea ● Principle bronchi Anatomy of upper airway Larynx in laryngoscopic view Nerves V1 V2 V3 IX Vagus nerve • Superior laryngeal n – External br (Motor) • cricothyroid m SL – Internal br (Sensory) • area above cord • Recurrent laryngeal n - Motor br • intrinsic m RL – Sensory br • area below cord Evaluation of the airway ● History ● Physical examination ● Special investigation Evaluation of the airway “History” ● Previous history of difficult airway ● Airway-related untoward events ● Airway-related symptoms/diseases Evaluation of the airway Physical examination ● Ease of open airway and maintenance ● Ease of tracheal intubation ● Teeth ● Neck movement ● Intubation hazards ● Signs of airway distress Evaluation of the airway Anatomic characteristics associated with difficult airway management ● Short muscular neck ● Receding mandible ● Protruding maxillary incisors ● Long high-arched palate ● Inability to visualize -

Tutor Guide – Pre-Oxygenation and Basic Airway Management Thank
Tutor Guide – Pre-oxygenation and Basic Airway Management Thank you very much for helping with the airway mastery learning program. Attached is the pre-course material which trainees should read and complete before attending. It includes a checklist and you should use this when assessing them. It also includes a pass mark, which should be regarded as formative rather than summative. Ideally the programme should be delivered as described here, but we recognise that not every department will be able to achieve this. • Teaching can take up to 60 minutes depending on the trainee. • There should ideally only be up to two trainees per tutor at a time. • Ideally the trainee should also have had an opportunity to practice with the equipment on the manikin prior to the session. • It is very important to create a safe space and non-threatening environment for the learner. Stages of the process are: 1. Trainee reads pre-course material and watches video before attending. 2. Participant performs procedure on the manikin as a formative assessment. 3. Tutor gives specific feedback about performance. 4. Trainee repeats procedure until you are happy they do it properly (this may need more than one session). Skills to assess as part of formative assessment (use checklist): 1. Conditions for airway management – demonstrate an understanding of equipment, monitoring, personnel and supervision needed for safe practice. 2. Demonstrates knowledge of pre-oxygenation goals. 3. Perform airway opening manoeuvres (including use of adjuncts). 4. Effective bag-valve-mask -

Management of Airway Emergencies (1995)
Reprinted from the July 1995 issue of RESPIRATORY CARE [Respir Care 1995;40(7):749–760] AARC Clinical Practice Guideline Management of Airway Emergencies MAE 1.0 PROCEDURE: Recognition of signs of an impending or actual airway emergency. Initial treatment and continued management of airway emergencies to minimize the likelihood of adverse outcomes, in adults, children, and infants. MAE 2.0 DESCRIPTION/DEFINITION: Management of airway emergencies (MAE) for the purpose of this guideline encompasses all care necessary to deal with sudden and often life-threatening events affecting natural and artificial airways and involves the identification, assessment, and treatment of patients in danger of losing or not being able to maintain an adequate airway, including the newborn. This includes (1) identification of the causes of airway emergencies; (2) management of airway emergencies prior to tracheal intubation; (3) use of adjunctive equipment and special techniques for establishing, maintaining, and monitoring effective ventilation; (4) translaryngeal tracheal intubation, including nasal and oral tracheal intubation; (5) transtracheal catheter ventilation, (6) percutaneous dilational cricothyrotomy, and; (7) surgical cricothyrotomy. MAE 3.0 SETTING: The guideline appliesRETIRED to a variety of settings including but not limited to hospitals and pre- or interhospital transport. MAE 4.0 INDICATIONS: 4.1 Conditions requiring management of the airway, in general, are impending or actual (1) airway compromise, (2) respiratory failure, and (3) need -

European Training Requirements in Anaesthesiology.Pdf
European Training Requirement ETR in ANAESTHESIOLOGY FROM THE STANDING COMMITTEE ON EDUCATION AND PROFESSIONAL DEVELOPMENT (EPD) OF THE SECTION AND BOARD OF ANAESTHESIOLOGY 1 Table of Contents Part 1. General information about the ETR ............................................................................................. 5 ETR update preparation .................................................................................................................. 5 Timelines in current ETR update preparation ................................................................................. 5 Duration and type of training .......................................................................................................... 6 Generic competencies and roles ..................................................................................................... 6 Part 2. Domains and competencies in the ETR ....................................................................................... 9 Definition of domains ...................................................................................................................... 9 Learning objectives .......................................................................................................................... 9 New aspects in the ETR update 2018 ............................................................................................ 10 Domain 1.1: Perioperative medicine, patient assessment and risk reduction ................................. 11 a. Knowledge ................................................................................................................................ -

EMT-Special Skill Curriculum
EMT-Special Skill Curriculum Supraglottic Airway Required curricula for conducting a Supraglottic Airway Endorsement Course for EMTs Revised December 2011 DOH 530-138 January 2012 This page intentionally left blank Page 3 OBJECTIVES LEGEND C=Cognitive P=Psychomotor A=Application 1=Knowledge 2=Application 3=Problem Solving Level LESSON TERMINAL OBJECTIVE: At the end of this lesson, the EMS provider will be able to utilize the assessment findings to formulate a field impression and implement the management plan for the patient experiencing an airway or breathing emergency. COGNITIVE OBJECTIVES: At the completion of this lesson, the EMS provider will be able to: 1. Identify the anatomy of the upper and lower airway. (C-1) 2. Describe the functions of the upper and lower airway. (C-1) 3. Define gag reflex. (C-1) 4. Establish the relationship between pulmonary circulation and respiration. (C-3) 5. Define the partial pressures and list the concentration of gases, which comprise atmospheric air. (C-1) 6. Describe the measurement of oxygen in the blood. (C-1) 7. Describe the measurement of carbon dioxide in the blood. (C-1) 8. List factors, which cause decreased oxygen concentrations in the blood. (C-1) 9. Define atelectasis. (C-1) 10. Define: • Hypoxia. (C-1) • Hypoxemia. (C-1) 11. List the factors, which increase carbon dioxide production in the body. (C-1) 12. List the factors, which decrease carbon dioxide elimination in the body. (C-1) 13. Describe the voluntary regulation of respiration. (C-1) 14. Describe the involuntary regulation of respiration. (C-1) 15. Describe the modified forms of respiration. -

Carolinas Healthcare Union Department of Anesthesiology
CAROLINAS HEALTHCARE UNION DEPARTMENT OF ANESTHESIOLOGY I have reviewed the DOP/Roster provided to me by MSS and confirm as indicated below: My DOP is accurate and reflects privileges relevant to my current practice I have listed privileges that should be removed: Printed Name: Signature: Date: If your roster indicates that you hold any of the privileges listed below, you must provide the maintenance criteria as described, in order to maintain the privilege. Your maintenance criteria and attestation must be returned together. Not applicable – no maintenance criteria STOP: UNLESS YOU ARE REQUESTING NEW OR ADDITIONAL PRIVILEGES, YOU DO NOT NEED TO GO BEYOND THIS POINT. CAROLINAS HEATLHCARE SYSTEM UNION Provider Name: __________________________________ CAROLINAS MEDICAL CENTER-UNION DELINEATION OF PRIVILEGES DEPARTMENT OF ANESTHESIOLOGY The Criteria for meeting the minimal requirements necessary for obtaining privileges in a specific area are listed under the following sections: A. General Anesthesiology Privileges B. Subspecialties in Anesthesiology C. Privileges granted to Anesthesiologists and other physicians Clinical privileges in the Department of Anesthesiology are based upon education, clinical training, demonstrated skills, current competence and the ability to perform all procedures requested and to manage procedurally related complications. It is the mission of the Department of Anesthesiology at CAROLINAS MEDICAL CENTER-UNION to provide high quality specialized anesthesia care twenty-four (24) hours per day for all patients, regardless of ability to pay or insurance status. If granted membership and privileges, applicants must assume all the functions and responsibilities of appointment and privileges in the Department of Anesthesiology, including care of unassigned patients, care of staff cases, equal share of Medicare, Medicaid and indigent care, emergency service care, subspecialty call, and consultation.