An Anesthesiologist's Perspective on the History of Basic Airway Management
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Annual Report 09
Department of Surgery 2008-2009 ANNUAL REPORT Mercer University School of Medicine The Medical Center of Central Georgia July 2009 Department of Surgery The general surgery residency had its start under its founding Program Director, Milford B. Hatcher, M.D., in 1958. Will C. Sealy, M.D., succeeded him in 1984. Internationally famous for his work in arrhythmia surgery, Dr. Sealy provided structure and rigor to the Department’s educational programs. In 1991, Martin Dalton, M.D., followed Dr. Sealy as Professor and Chair. Dr. Dalton, another nationally prominent cardiotho- racic surgeon, had participated in the first human lung transplant during his training at the University of Mississippi with James Hardy, M.D. Dr. Dalton continued the academic growth of the Department, adding important clinical programs in trauma and critical care under Dennis Ashley, M.D., and surgical research Milford B. Hatcher, M.D. under Walter Newman, Ph.D., and Zhongbiao Wang, M.D. The residency grew to four from two chief resident positions, and regularly won approval from the Residency Review Committee for Surgery. With the selection of Dr. Dalton as the Dean of the School of Medicine at Mercer, Don Nakayama, M.D., a pediatric surgeon, was named the Milford B. Hatcher Professor and Chair of the Department of Surgery in 2007. The Residency in Surgery currently has four categorical residents each year. It has been fully accredited by the Residency Review Committee for Surgery of the Accreditation Council for Graduate Medical Education. Its last approval was in 2006 for four years, Will C. Sealy, M.D. with no citations. -

{Download PDF} Genius on the Edge: the Bizarre Double Life of Dr. William Stewart Halsted
GENIUS ON THE EDGE: THE BIZARRE DOUBLE LIFE OF DR. WILLIAM STEWART HALSTED PDF, EPUB, EBOOK Gerald Imber | 400 pages | 01 Feb 2011 | Kaplan Aec Education | 9781607148586 | English | Chicago, United States How Halsted Altered the Course of Surgery as We Know It - Association for Academic Surgery (AAS) Create a free personal account to download free article PDFs, sign up for alerts, and more. Purchase access Subscribe to the journal. Rent this article from DeepDyve. Sign in to download free article PDFs Sign in to access your subscriptions Sign in to your personal account. Get free access to newly published articles Create a personal account or sign in to: Register for email alerts with links to free full-text articles Access PDFs of free articles Manage your interests Save searches and receive search alerts. Get free access to newly published articles. Create a personal account to register for email alerts with links to free full-text articles. Sign in to save your search Sign in to your personal account. Create a free personal account to access your subscriptions, sign up for alerts, and more. Purchase access Subscribe now. Purchase access Subscribe to JN Learning for one year. Sign in to customize your interests Sign in to your personal account. Halsted is without doubt the father of modern surgery, and his eccentric behavior, unusual lifestyle, and counterintuitive productivity in the face of lifelong addiction make his story unusually compelling. The result is an illuminating biography of a complex and troubled man, whose genius we continue to benefit from today. Gerald Imber is a well known plastic surgeon and authority on cosmetic surgery, and directs a private clinic in Manhattan. -

Importance of Validation Risk Prediction Tools
Art: toc Input-citi 22:40 12/2/7 12؍balt6/z7i-anesth/z7i-anesth/z7i00812/contents panickes S ON THE COVER: David Mackey, M.D., has organized a fascinating series of commentaries by national leaders In this issue of ANESTHESIOLOGY, two original research articles and three editorial views examine in the construction and use of clinical data registries by regulatory agencies and physician the use of data in clinical decision making. practices, the first two of which appear in this month’s issue: ● Kheterpal et al.: Impact of a Novel Multiparameter Decision Support System on Intraoperative ● Mackey: Can We Finally Conquer the Problem of Medical Quality? The Systems-based Processes of Care and Postoperative Outcomes, p. 272 Opportunities of Data Registries and Medical Teamwork, p. 225 ● Liu et al.: Defining the Intrinsic Cardiac Risks of Operations to Improve Preoperative Cardiac ● Jain et al.: A Public-Private Strategy to Advance the Use of Clinical Registries, p. 227 Risk Assessments, p. 283 Downloaded from http://pubs.asahq.org/anesthesiology/article-pdf/128/2/A1/364553/20180200_0-00001.pdf by guest on 01 October 2021 ● Sessler: Decision Support Alerts: Importance of Validation, p. 241 ● Glance et al.: Risk Prediction Tools: The Need for Greater Transparency, p. 244 ● Javitt: Regulatory Landscape for Clinical Decision Support Technology, p. 247 ᭛ THIS MONTH IN ANESTHESIOLOGY 9A ᭛◆ THISEDITORIAL MONTH VIEWS IN ANESTHESIOLOGY 1A . Can We Finally Conquer the Problem of Medical Quality? The Systems-based ◼ SCIENCE, MEDICINE, AND THE ANESTHESIOLOGIST 15A Opportunities of Data Registries and Medical Teamwork 225 David C. Mackey ◼ INFOGRAPHICS IN ANESTHESIOLOGY 19A . A Public-Private Strategy to Advance the Use of Clinical Registries 227 Sachin H. -

Original Article
Archive of SID ORIGINAL ARTICLE A Short Review on the History of Anesthesia in Ancient Civilizations 147 Abstract Javad Abdoli1* Anesthesia is one of the main issues in surgery and has progressed a Seyed Ali Motamedi2, 3* 4 lot since two centuries ago. The formal history of surgery indicates that Arman Zargaran beginning of anesthesia backs to the 18th century, but reviewing the 1- BS Student at Department of Anes- thesiology, Alborz University of Medical history of medicine shows that pain management and anesthesia has a Science, Alborz, Iran long history in ancient times. The word “anesthesia”, comes from Greek 2- BS Student at Scientific Research Center, Tehran University of Medical language: an-(means: “without”) and aisthēsis (means: “sensation”), the Science, Tehran, Iran combination of which means the inhibition of sensation. The oldest re- 3- BS Student at Department of Anes- thesiology, Tehran University of Medical ports show that the Sumerians maybe were the first people that they cul- Science, Tehran, Iran tivated and harvested narcotic sedative like the opium Poppy as early as 4- PharmD, PhD, Assistant Professor, Department of History of Medicine, 3400 BC and used them as pain killers. There are some texts which show School of Traditional Medicine, Tehran us that Greek and Mesopotamia’s doctors prescribed alcoholic bever- University of Medical Science, Tehran, ages before their surgeries. In the Byzantine time, physicians used an Iran elixir known as “laudanum” that was a good sedative prior the patient’s *Javad Abdoli and Seyed Ali Mota- medi has an equal role as first author operation. Ancient Persia and China were as the biggest civilizations, of in this paper. -
RN to EMT-Basic Transition Course
State of Wisconsin Registered Nurse to EMT-Basic Transition Course November 2010 Wisconsin EMS Section State of Wisconsin RN to EMT-Basic Transition Course TABLE OF CONTENTS Introduction .....................................................................................................iv List of Appendices...........................................................................................vi Module 1 – Preparatory 1-1 Introduction to Emergency Care .................................................. 1-1 1-2 Well-Being of the EMT Basic ....................................................... 1-6 1-3 Medical/Legal and Ethical Issues............................................... 1-12 1-5 Lifting and Moving Patients........................................................ 1-16 1-6 Evaluation .................................................................................. 1-25 Module 2 - Patient Assessment 2-1 Scene Size-up ............................................................................. 2-1 2-2 Initial Assessment........................................................................ 2-6 2-3 Baseline Vital Signs, SAMPLE History and the Use of Pulse Oximetry .......................................................................... 2-11 2-4 Focused History and Physical Exam: Trauma ........................... 2-16 2-5 Focused History and Physical Exam: Medical ........................... 2-22 2-6 Detailed Physical Exam ............................................................. 2-27 2-7 On-Going Assessment.............................................................. -

General Surgery and Semiology
„Nicolae Testemiţanu” State University of Medicine and Pharmacy Department of General Surgery and Semiology E.Guţu, D.Casian, V.Iacub, V.Culiuc GENERAL SURGERY AND SEMIOLOGY LECTURE SUPPORT for the 3rd-year students, faculty of Medicine nr.2 2nd edition Chişinău, 2017 2 CONTENTS I. Short history of surgery 5 II. Antisepsis 6 Mechanical antisepsis 6 Physical antisepsis 6 Chemical antisepsis 6 Biological antisepsis 7 III. Aseptic technique in surgery 9 Prevention of airborne infection 9 Prevention of contact infection 9 Prevention of contamination by implantation 10 Endogenous infection 10 Antibacterial prophylaxis 10 IV. Hemorrhage 11 Classifications of bleeding 11 Reactions of human organism to blood loss 11 Clinical manifestations and diagnosis 12 V. Blood coagulation and hemostasis 14 Blood coagulation 14 Syndrome of disseminated intravascular coagulation 14 Medicamentous and surgical hemostasis 15 VI. Blood transfusion 17 History of blood transfusion 17 Blood groups 17 Blood transfusion 18 Procedure of blood transfusion 19 Posttransfusion reactions and complications 20 VII. Local anesthesia 22 Local anesthetics 22 Types of local anesthesia 23 Topical anesthesia 23 Tumescent anesthesia 23 Regional anesthesia 24 Blockades with local anesthetics 25 VIII. Surgical intervention. Pre- and postoperative period 26 Preoperative period 26 Surgical procedure 27 Postoperative period 28 IX. Surgical instruments. Sutures and knots 29 Surgical instruments 29 Suture material 30 Knots and sutures 31 X. Dressings and bandages 32 3 Triangular bandages 32 Cravat bandages 32 Roller bandages 33 Elastic net retention bandages 35 XI. Minor surgical procedures and manipulations 36 Injections 36 Vascular access 36 Thoracic procedures 36 Abdominal procedures 37 Gastrointestinal procedures 37 Urological procedures 38 XII. -

History of Surgery in Turkey Dr
History of Surgery in Turkey Dr. Neset Koksal UEMS Surgery Section Meeting, 5-6 April, Istanbul Hittites, Phrygians, Lydians, Ions, Urartu (B.C. 2000 - B.C. 600) Persians (B.C. 543-333) Empire of Alexander the Great Roman Empire Byzantines (395-1071) Turks (1071-to present) • Central Asian Turkic States • Great Seljuk State Period • Ottoman Empire Period • Republic Period Prof. Dr. İbrahim Ceylan, Türklerde Cerrahinin Gelişimi. TCD, 2012 • Medical history goes back to the eighth century, the time of the Uyghurs and Orhon Turks. During this period surgeons from neighboring countries had an influence on Turkish medicine and some written data were established. • Physicians were educated in hospitals in a "master-apprentice" relation. Akinci S Dissection and autopsy in Ottoman Empire [in Turkish]. Istanbul Tip Falcultesi Mecmuasi. 1962;2597- 115 Central Asian Turkic States • The first Turkish medicine text belongs to the Uyghurs. • various eye diseases, headache, ear, nose and oral diseases, respiratory and heart diseases, diseases related to children and childbirth, sexual organ diseases. • Uyghurs tried to treat some diseases by cauterisation which is a different application of acupuncture. The first Turkish medical text found in Turfan excavations. (History of the World and Turkish Medicine, picture 141, depicted by Ilter Uzel) İbni Sina (Avicenna) (980-1037) • Died at the age of 57; he left more than 150 works on physics, astronomy, medicine and philosophy. • He hypothesised the presence of creatures that are invisible to the eye causing transmission of some diseases hence sensed the presence of microbes without microscope. İbni Sina (Avicenna) (980-1037) • Surgical intervention was not preferred because of inadequate knowledge of anatomy, development of surgical instruments and fighting against pain and microbes. -

The Effects of the General Anaesthetic Propofol on Drosophila Larvae Drew Min Su Cylinder Bachelor of Science
The effects of the general anaesthetic propofol on Drosophila larvae Drew Min Su Cylinder Bachelor of Science A thesis submitted for the degree of Master of Philosophy at The University of Queensland in 2019 Queensland Brain Institute Abstract Although general anaesthetics have been in use since the mid-19th century, the mechanism by which these drugs induce reversible loss of consciousness is still poorly understood. Previous research has indicated that general anaesthetics activate endogenous sleep pathways by potentiating GABAA receptors in wake-promoting neurons. However, more recent studies have demonstrated that general anaesthetics also inhibit synaptic release through interactions with the SNARE complex, an integral part of presynaptic neurotransmitter release machinery in all neurons. The presynaptic and postsynaptic mechanisms may thus be linked in a two-step process: at low doses, general anaesthetics activate sleep-promoting circuits, thereby producing unconsciousness, while at the higher doses necessary for surgery, general anaesthetics inhibit presynaptic release machinery brain-wide, thereby causing a total loss of behavioural responsiveness. While this hypothesis remains speculative, it is testable in animal models. This study develops larval Drosophila melanogaster as an animal model to test this hypothesis in the context of a common intravenous GABA-acting general anaesthetic, propofol. Although presynaptic effects of general anaesthetics have been studied in larval neuromuscular junction preparations, there is not much data for how these drugs affect larval behaviour or brain activity. General anaesthesia is easily addressed in animal models because it can be described as a state of decreased responsiveness which can be assessed using diverse behavioural endpoints. In this study, a series of behavioural assays were designed and tested to assess the effect of GABA-acting general anaesthetics and sedative drugs on Drosophila larvae. -
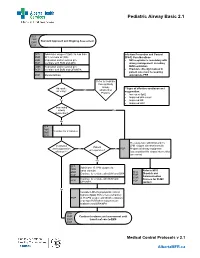
Pediatric Airway Basic 2.1
Pediatric Airway Basic 2.1 SFA FMR Standard Approach and Ongoing Assessment EMR PCP SFA Administer oxygen if SpO2 Is less than Infection Prevention and Control FMR 94% on room air (RA) (IP&C) Considerations EMR Reposition and/or suction prn • N95 respirator is mandatory with PCP Ventilate with BVM and OPA airway management, including EMR Reposition and/or suction prn BVM ventilation PCP Ventilate with BVM and OPA/NPA • Providers directly involved in patient care must be wearing PCP Monitor EtCO2 appropriate PPE Refer to Pediatric Foreign Body Airway Adequate **Signs of effective ventilation and No Obstruction air entry? oxygenation: Protocol • Increased Sp02 • Improved skin colour Yes • Improved HR • Improved LOC Impending airway Yes obstruction? No SFA FMR Ventilate for 2 minutes EMR PCP Pre-oxygenate with NRB and 15 Ventilation LPM oxygen via nasal cannula Patient and oxygenation No No PCP Prepare all airway equipment unresponsive? effective?** Assess patient for airway intervention (see notes) Yes SFA Administer 15 LPM oxygen via FMR nasal cannula Refer to MFR EMR SFA Continue to ventilate with BVM and OPA Dispatch and PCP FMR Communication EMR Continue to ventilate with BVM and Process for OLMC PCP PCP OPA/NPA contact Yes Consider LMA if symptomatic critical hypoxia (SpO2 85% or less) refractory PCP to 15 LPM oxygen with BVM ventilation (2-person BVM when resources are available) and OPA/NPA SFA FMR Continue treatment and assessment until EMR transfer of care to EMS PCP Medical Control Protocols v 2.1 AlbertaMFR.ca Pediatric Airway Basic 2.1 Definition Basic airway management is known to improve patient survival rates in the prehospital field. -

Airway Management and Ventilation: 1 W4444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444
Airway: 2 Airway Management and Ventilation: 1 W4444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444 UNIT TERMINAL OBJECTIVE 2-1 At the completion of this unit, the EMT-Intermediate student will be able to establish and/ or maintain a patent airway, oxygenate, and ventilate a patient. COGNITIVE OBJECTIVES At the completion of this unit, the EMT-Intermediate student will be able to: 2-1.1 Explain the primary objective of airway maintenance. (C-1) 2-1.2 Identify commonly neglected prehospital skills related to airway. (C-1) 2-1.3 Identify the anatomy and functions of the upper airway. (C-1) 2-1.4 Describe the anatomy and functions of the lower airway. (C-1) 2-1.5 Explain the differences between adult and pediatric airway anatomy. (C-1) 2-1.6 Define normal tidal volumes for the adult, child, and infant. (C-1) 2-1.7 Define atelectasis. (C-1) 2-1.8 Define FiO2. (C-1) 2-1.9 Explain the relationship between pulmonary circulation and respiration. (C-3) 2-1.10 List factors which cause decreased oxygen concentrations in the blood. (C-1) 2-1.11 List the factors which increase and decrease carbon dioxide production in the body. (C 2-1.12 Describe the measurement of oxygen in the blood. (C-1) 2-1.13 Describe the measurement of carbon dioxide in the blood. (C-1) 2-1.14 List the concentration of gases which comprise atmospheric air. (C-1) 2-1.15 List the factors which affect respiratory rate and depth. (C-1) 2-1.16 Describe the voluntary and involuntary regulation of respiration. -

Basic Airway Management & Decision Making
Roberts: Clinical Procedures in Emergency Medicine, 5th ed. CHAPTER 3 – Basic Airway Management and Decision-Making Robert F. Reardon, Phillip E. Mason, Joseph E. Clinton Over the last few decades, several important changes have occurred in emergency airway management. Bag-mask ventilation has been supplemented by intermediate, or backup, ventilation devices like the laryngeal mask airway (LMA), the Combitube, and the laryngeal tube. These have become important devices for the initial resuscitation of apneic patients and for rescue ventilation when intubation fails.[1] Noninvasive positive-pressure ventilation (NPPV) is now used in place of tracheal intubation in some critically ill patients. Despite these advances, basic techniques such as opening the airway, oxygenation, and bag-mask ventilation remain the cornerstones of good emergency airway management. [2] [3] Airway maintenance without endotracheal intubation is one of the most important emergency [4] airway management techniques to keep patients alive until a definitive airway can be established. This chapter describes basic airway skills including opening the airway, O2 therapy, NPPV, bag-mask ventilation, and intermediate ventilation devices. Because of the complexity of these skills and decisions, providers should develop a simple, organized approach to emergency airway management, being cognizant that when a specific intervention has failed, it is time to move rapidly to a different approach. Developing a simple preconceived algorithm that employs proven techniques and is applicable to a broad range of clinical scenarios will help providers manage difficult, anxiety-provoking emergency airways. THE CHALLENGE OF EMERGENCY AIRWAY MANAGEMENT Although other specialists are sometimes available, most emergency airways are managed by emergency clinicians.[5] Airway management in the emergency department (ED) is much different from airway management in the controlled setting of the operating room. -

Me Ancestors of Inhalational Anesthesia Me Soponic Sponges (Xitb-Xvlltls Centuries) a Universally Recommended Medical Technique Was Abruptly
265 Anesthesiology 2000; 93265-9 0 2000 American Society of Anesthesiologists, Inc. Iippincott Williams & Willcins, Inc. me Ancestors of Inhalational Anesthesia me Soponic Sponges (XItb-xvlltls Centuries) a Universally Recommended Medical Technique Was Abruptly How Downloaded from http://pubs.asahq.org/anesthesiology/article-pdf/93/1/265/330537/0000542-200007000-00037.pdf by guest on 30 September 2021 Discarded Philippe Juvin, M.D.,* Jean-Marie Desmonts, M.D. t THE history of anesthesia is intimately linked to the of a sponge soaked in juices of plants with hypnotic history of surgery. The textbooks of the Hippocratic properties under the nose of the patient. The current Collection,which are the oldest surviving books of West- article describes the changing composition of the sopo- ern medicine, describe a number of elaborate surgical rific sponges during the centuries and the conflicting techniques. These procedures must have necessitated opinions about their effectiveness. that the patient remained perfectly still, suggesting that restraints were probably used, and some degree of anal- gesia or partial alteration of consciousness. Methods The Abbeys (VIth-XIth Centuries) available at the time to obtain adequate operating con- At the councils held by the Roman Catholic Church in ditions included application of heat or cold, jugular vein the VIth century, the bishops of the Western world were compression,2and oral administration of alcoholic bev- urged to attend diligently to their duties of hospitality erages or potions prepared from plants with sedative and assistance. They were invited to set up hospitalia effects. Sedative substances inhaled at the time, but only near their residences, offering beds for the crippled and in nonmedical situations, such as that of the Delphic the needy.5 Little by little, hospitalia were created in priestess, who uttered her oracles while in a trance rural parishes, along roads (most notably those traveled induced as a result of the inhalation of hallucinogenic by pilgrims), near monasteries, or, sometimes, as in Saint vapors.