A Brief History of Local Anesthesia REVIEW ARTICLE
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Annual Report 09
Department of Surgery 2008-2009 ANNUAL REPORT Mercer University School of Medicine The Medical Center of Central Georgia July 2009 Department of Surgery The general surgery residency had its start under its founding Program Director, Milford B. Hatcher, M.D., in 1958. Will C. Sealy, M.D., succeeded him in 1984. Internationally famous for his work in arrhythmia surgery, Dr. Sealy provided structure and rigor to the Department’s educational programs. In 1991, Martin Dalton, M.D., followed Dr. Sealy as Professor and Chair. Dr. Dalton, another nationally prominent cardiotho- racic surgeon, had participated in the first human lung transplant during his training at the University of Mississippi with James Hardy, M.D. Dr. Dalton continued the academic growth of the Department, adding important clinical programs in trauma and critical care under Dennis Ashley, M.D., and surgical research Milford B. Hatcher, M.D. under Walter Newman, Ph.D., and Zhongbiao Wang, M.D. The residency grew to four from two chief resident positions, and regularly won approval from the Residency Review Committee for Surgery. With the selection of Dr. Dalton as the Dean of the School of Medicine at Mercer, Don Nakayama, M.D., a pediatric surgeon, was named the Milford B. Hatcher Professor and Chair of the Department of Surgery in 2007. The Residency in Surgery currently has four categorical residents each year. It has been fully accredited by the Residency Review Committee for Surgery of the Accreditation Council for Graduate Medical Education. Its last approval was in 2006 for four years, Will C. Sealy, M.D. with no citations. -

{Download PDF} Genius on the Edge: the Bizarre Double Life of Dr. William Stewart Halsted
GENIUS ON THE EDGE: THE BIZARRE DOUBLE LIFE OF DR. WILLIAM STEWART HALSTED PDF, EPUB, EBOOK Gerald Imber | 400 pages | 01 Feb 2011 | Kaplan Aec Education | 9781607148586 | English | Chicago, United States How Halsted Altered the Course of Surgery as We Know It - Association for Academic Surgery (AAS) Create a free personal account to download free article PDFs, sign up for alerts, and more. Purchase access Subscribe to the journal. Rent this article from DeepDyve. Sign in to download free article PDFs Sign in to access your subscriptions Sign in to your personal account. Get free access to newly published articles Create a personal account or sign in to: Register for email alerts with links to free full-text articles Access PDFs of free articles Manage your interests Save searches and receive search alerts. Get free access to newly published articles. Create a personal account to register for email alerts with links to free full-text articles. Sign in to save your search Sign in to your personal account. Create a free personal account to access your subscriptions, sign up for alerts, and more. Purchase access Subscribe now. Purchase access Subscribe to JN Learning for one year. Sign in to customize your interests Sign in to your personal account. Halsted is without doubt the father of modern surgery, and his eccentric behavior, unusual lifestyle, and counterintuitive productivity in the face of lifelong addiction make his story unusually compelling. The result is an illuminating biography of a complex and troubled man, whose genius we continue to benefit from today. Gerald Imber is a well known plastic surgeon and authority on cosmetic surgery, and directs a private clinic in Manhattan. -

Femoral Nerve Block Versus Spinal Anesthesia for Lower Limb
Alexandria Journal of Anaesthesia and Intensive Care 44 Femoral Nerve Block versus Spinal Anesthesia for Lower Limb Peripheral Vascular Surgery By Ahmed Mansour, MD Assistant Professor of Anesthesia, Faculty of Medicine, Alexandria University. Abstract Perioperative cardiac complications occur in 4% to 6% of patients undergoing infrainguinal revascularization under general, spinal, or epidural anesthesia. The risk may be even greater in patients whose cardiac disease cannot be fully evaluated or treated before urgent limb salvage operations. Prompted by these considerations, we investigated the feasibility and results of using femoral nerve block with infiltration of the genito4femoral nerve branches in these high-risk patients. Methods: Forty peripheral vascular reconstruction of lower limbs were performed under either spinal anesthesia (20 patients) or femoral nerve block with infiltration of genito-femoral nerve branches supplemented with local infiltration at the site of dissection as needed (20 patients). All patients had arterial lines. Arterial blood pressure and electrocardiographic monitoring was continued during surgery, in PACU and in the intensive care units. Results: Operations included femoral-femoral, femoral-popliteal bypass grafting and thrombectomy. The intra-operative events showed that the mean time needed to perform the block and dose of analgesics and sedatives needed during surgery was greater in group I (FNB,) compared to group II [P=0.01*, P0.029* , P0.039*], however, the time needed to start surgery was shorter in group I than in group II [P=0. 039]. There were no block failures in either group, but local infiltration in the area of the dissection with 2 ml (range 1-5 ml) of 1% lidocaine was required in 4 (20%) patients in FNB group vs none in the spinal group. -

Lidocaine Infusion for Analgesia MOA Pharmacology 1
Lidocaine Infusion for Analgesia MOA Pharmacology 1. Attenuation of proinflammatory effects: Ø Hepatic metabolism with high extraction ratio; Ø Blocks polymorphonuclear granulocyte priming, plasma clearance is 10 ml/kg/min13 reducing release of cytokines & reactive oxygen species1 Ø Adjust dose based on hepatic function and 2. Diminish nociceptive signaling to central nervous system: blood flow Ø Inhibition of G-protein-mediated effects2 Ø Renal clearance of metabolites Ø Reduces sensitivity & activity of spinal cord neurons Ø Context-sensitive half-time after a 3-day infusion is (glycine and NMDA receptor mediated)3,4 ∼20–40 min Ø Clinical effect of lidocaine tends to exceed the 5 3. Reduces ectopic activity of injured afferent nerves duration of the infusion by 5.5 times the half-life, supporting the putative preventive analgesia effect14 Perioperative Use Dosing Ø IV local anesthetic infusions have been used safely for pain control in the perioperative setting since the early 1950’s6,7 Infusion: 2mg/kg/hr (range 1.5-3 mg/kg/hr) Ø Reduce pain, nausea, ileus duration, opioid requirement, Loading dose: 1.5mg/kg (range 1-2 mg/kg) and length of hospital stay Ø Strongly consider bolus to rapidly achieve therapeutic concentration, otherwise steady state 9-12 Evidence for Specific Surgeries: reached in 4-8 hr Ø Strong: Open & laparoscopic abdominal; Reduces Max dose: 4.5 mg/kg postoperative pain, speeds return of bowel function, Ø Consider total dose from other local anesthetics reduces PONV, reduces length of hospital stay (e.g. regional anesthesia, periarticular injections, & Ø Moderate: Open prostatectomy, thoracic procedures, local infiltration) ambulatory surgery, and major spine; Reduces Continuous infusions up to 3 mg/kg/hr have been postoperative pain and opioid consumption shown to be safe Ø Moderate: Breast; Prevention of chronic postsurgical pain Ø Reduce infusion rate in patients with impaired Ø No benefit: Total abdominal hysterectomy, total hip drug metabolism & clearance (i.e. -

Local Anesthetic Toxicity: Prevention and Treatment
Local Anesthetic Toxicity: Prevention and Treatment John W. Wolfe, M.D. Staff Anesthesiologist Indiana University School of Medicine Indianapolis, Indiana John F. Butterworth, M.D. Chairman, Department of Anesthesia Indiana University School of Medicine Indianapolis, Indiana LESSON OBJECTIVES dine, and the site of injection on peak Upon completion of this lesson, the reader local anesthetic concentrations in blood. should be able to: 6. Describe the mechanism of local anes- 1. List the signs and symptoms of local thetic central nervous system toxicity. anesthetic toxicity. 7. Identify the risk factors for local anes- 2. Discuss the concept of "maximum safe thetic toxicity. doses of a local anesthetic." 8. Plan the treatment of local anesthetic- 3. Describe methods for reducing the risk of induced cardiac arrhythmias and cardiac local anesthetic toxicity. arrest. 4. Explain the treatment of local anes- 9. Describe the mechanism of local anes- thetic-related neurologic symptoms and thetic cardiovascular toxicity. toxic side effects. 10. Explain the dosage and proposed mech- 5. Discuss the effects of epinephrine, cloni- anism of lipid emulsion therapy. Current Reviews for Nurse Anesthetists designates this lesson for 1 CE contact hour in Clinical pharmacology/therapeutics. Introduction Mechanism of Cardiac and central nervous system (CNS) toxic Local Anesthetic Toxicity side effects of local anesthetics are relatively rare but potentially catastrophic complications of local and Local anesthetics normally produce their desired regional anesthesia. Fortunately, the likelihood of a effects on peripheral nerves by binding and inhibit- local anesthetic toxic event can be reduced by ad- ing voltage-gated sodium channels in neural cell herence to good technique. -
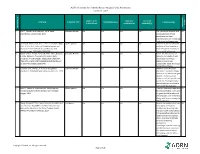
AORN Guideline for Patients Receiving Local-Only Anesthesia Evidence Table
AORN Guideline for Patients Receiving Local-Only Anesthesia Evidence Table SAMPLE SIZE/ CONTROL/ OUTCOME CITATION EVIDENCE TYPE INTERVENTION(S) CONCLUSION(S) POPULATION COMPARISON MEASURE(S) SCORE CONSENSUS REFERENCE # REFERENCE 1 Lirk P., Picardi S. and Hollmann, M. W. Local Literature Review n/a n/a n/a n/a The mechanism of action and VA anaesthetics: 10 essentials. 2014 access pathways of local anesthetics and their pharmokinetics are increasingly understood and appreciated. 2 Calatayud, Jesús, M.D.,D.D.S., Ph.D., González, Õngel, Expert Opinion n/a n/a n/a n/a A review of the discovery and VA M.D., D.D.S., Ph.D. History of the development and evolution of local anesthesia evolution of local anesthesia since the coca leaf. from the Spanish discovery of Anesthesiology. 2003;98(6):1503-1508. the coca leaf in America. 3 Gordh T, M.D., Gordh, Torsten E.,M.D., Ph.D., Lindqvist Literature Review n/a n/a n/a n/a Before the introduction of VA K, M.Sc. Lidocaine: The origin of a modern local lidocaine, the choice of local anesthetic. Anesthesiology. 2010;113(6):1433-1437. anesthetics was limited. https://doi.org/10.1097/ALN.0b013e3181fcef48. doi: Lidocaine's onset was 10.1097/ALN.0b013e3181fcef48. substantially faster and longer lasting than procaine. 4 Volcheck G.W., Mertes, P. M. Local and general Literature Review n/a n/a n/a n/a Whether to test the local VA anesthetics immediate hypersensitivity reactions. 2014 anesthetic causing the allergic reaction or an alternative agent depends on the expected future need of the specific local anesthetic. -

The Use of Buffering Solutions in the Pediatrics Local Anesthesia to Reduce the Pain of Minor Procedures
Volume 2- Issue 1 : 2018 DOI: 10.26717/BJSTR.2018.02.000695 Eduardo de Oliveira Duque-Estrada. Biomed J Sci & Tech Res ISSN: 2574-1241 Mini Review Open Access The Use of Buffering Solutions in the Pediatrics Local Anesthesia to Reduce the Pain of Minor Procedures Eduardo de Oliveira Duque-Estrada MD* Received: January 17, 2018; Published: January 25, 2018 *Corresponding author: Eduardo de Oliveira Duque-Estrada, Ex-Professor of Pediatrics and Pediatric Surgery, Teresópolis Schoolof Medicine, Rio de Janeiro, Rua Jose da Silva Ribeiro 119 apt 11 São Paulo, SP Brazil CEP: 05726-130, Email: Abstract The local anesthetics are widely u sed in minor pediatric surgical procedures. The major problem with their use is the resulted pain experienced by the patients at the time of injection. To discuss those situations in the light of the medical literature we present this mini-review. Key words: Local Injection; Pain; Buffer; pH; Lidocaine; Pediatric Surgery Procedure Introduction Table 1: Techniques for injection pain control*. a eutectic mixture of lidocaine and prilocaine (EMLA) cream [17] S.No Techniques for injection pain control before infiltration, and local external cooling (cryoanalgesia) have 1. Warming the anesthetic solution [18,19] (Table 1). also been used to reduce the pain of infiltration of local anesthetic 2. Buffering the anesthetic Buffering the Anesthetic 3. Injection technique 4. Distraction Local anesthesia is extremely useful either as the sole method the best results on the minor surgery in general [3,6]. Blocking 5. Combination anesthetic technique the pain pathway with local anesthetic solution will also reduce 6. Cooling of skin the family stress response to the surgical procedure. -

Veterinary Anesthetic and Analgesic Formulary 3Rd Edition, Version G
Veterinary Anesthetic and Analgesic Formulary 3rd Edition, Version G I. Introduction and Use of the UC‐Denver Veterinary Formulary II. Anesthetic and Analgesic Considerations III. Species Specific Veterinary Formulary 1. Mouse 2. Rat 3. Neonatal Rodent 4. Guinea Pig 5. Chinchilla 6. Gerbil 7. Rabbit 8. Dog 9. Pig 10. Sheep 11. Non‐Pharmaceutical Grade Anesthetics IV. References I. Introduction and Use of the UC‐Denver Formulary Basic Definitions: Anesthesia: central nervous system depression that provides amnesia, unconsciousness and immobility in response to a painful stimulation. Drugs that produce anesthesia may or may not provide analgesia (1, 2). Analgesia: The absence of pain in response to stimulation that would normally be painful. An analgesic drug can provide analgesia by acting at the level of the central nervous system or at the site of inflammation to diminish or block pain signals (1, 2). Sedation: A state of mental calmness, decreased response to environmental stimuli, and muscle relaxation. This state is characterized by suppression of spontaneous movement with maintenance of spinal reflexes (1). Animal anesthesia and analgesia are crucial components of an animal use protocol. This document is provided to aid in the design of an anesthetic and analgesic plan to prevent animal pain whenever possible. However, this document should not be perceived to replace consultation with the university’s veterinary staff. As required by law, the veterinary staff should be consulted to assist in the planning of procedures where anesthetics and analgesics will be used to avoid or minimize discomfort, distress and pain in animals (3, 4). Prior to administration, all use of anesthetics and analgesic are to be approved by the Institutional Animal Care and Use Committee (IACUC). -

Original Article
Archive of SID ORIGINAL ARTICLE A Short Review on the History of Anesthesia in Ancient Civilizations 147 Abstract Javad Abdoli1* Anesthesia is one of the main issues in surgery and has progressed a Seyed Ali Motamedi2, 3* 4 lot since two centuries ago. The formal history of surgery indicates that Arman Zargaran beginning of anesthesia backs to the 18th century, but reviewing the 1- BS Student at Department of Anes- thesiology, Alborz University of Medical history of medicine shows that pain management and anesthesia has a Science, Alborz, Iran long history in ancient times. The word “anesthesia”, comes from Greek 2- BS Student at Scientific Research Center, Tehran University of Medical language: an-(means: “without”) and aisthēsis (means: “sensation”), the Science, Tehran, Iran combination of which means the inhibition of sensation. The oldest re- 3- BS Student at Department of Anes- thesiology, Tehran University of Medical ports show that the Sumerians maybe were the first people that they cul- Science, Tehran, Iran tivated and harvested narcotic sedative like the opium Poppy as early as 4- PharmD, PhD, Assistant Professor, Department of History of Medicine, 3400 BC and used them as pain killers. There are some texts which show School of Traditional Medicine, Tehran us that Greek and Mesopotamia’s doctors prescribed alcoholic bever- University of Medical Science, Tehran, ages before their surgeries. In the Byzantine time, physicians used an Iran elixir known as “laudanum” that was a good sedative prior the patient’s *Javad Abdoli and Seyed Ali Mota- medi has an equal role as first author operation. Ancient Persia and China were as the biggest civilizations, of in this paper. -
Local Anesthesia for Carpal Tunnel Surgery
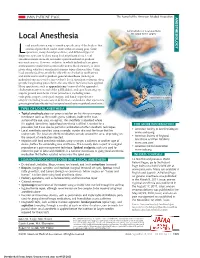
JAMA PATIENT PAGE The Journal of the American Medical Association ANESTHESIOLOGY Administration of local anesthetic Local Anesthesia for carpal tunnel surgery ocal anesthesia is a way to numb a specific area of the body so that a medical procedure can be done without causing pain. Some Loperations, many dental procedures, and different types of diagnostic tests can be done using local anesthesia alone. Local anesthesia medications do not make a person sedated or produce unconsciousness. However, sedation, in which individuals are given medications to make them comfortable and to block memory, is often given along with local anesthesia for many types of procedures. Using local anesthesia alone avoids the side effects of sedation medications and medications used to produce general anesthesia (making an individual unconscious for a procedure). Local anesthetic solutions often provide long-lasting pain relief to the area where they have been applied. Many operations, such as appendectomy (removal of the appendix), cholecystectomy (removal of the gallbladder), and open heart surgery, require general anesthesia. Other procedures, including some orthopedic surgery, urological surgery, and female reproductive Carpal tunnel surgery surgery (including most cesarean deliveries), can be done after a person is given regional anesthesia (such as spinal anesthesia or epidural anesthesia). TYPES OF LOCAL ANESTHESIA • Topical anesthesia places or sprays a solution on the skin or a mucous membrane (such as the mouth, gums, eardrum, inside of the nose, surface of the eye, anus, or vagina). The anesthetic is absorbed where it is applied. Sometimes topical local anesthesia is all that is needed for a FOR MORE INFORMATION procedure, but it can also be part of a combination of other anesthetic techniques. -

Veterinary Anesthesia and Pain Management Secrets / Edited by Stephen A
Publisher: HANLEY & BELFUS, INC. Medical Publishers 210 South 13th Street Philadelphia, PA 19107 (215) 546-7293; 800-962-1892 FAX (215) 790-9330 Web site: http://www.hanleyandbelfus.com Note to the reader Although the information in this book has been carefully reviewed for cor rectness of dosage and indications, neither the authors nor the editor nor the publisher can accept any legal responsibility for any errors or omissions that may be made. Neither the publisher nor the editor makes any warranty, expressed or implied, with respect to the material contained herein. Before prescribing any drug. the reader must review the manu facturer's correct product information (package inserts) for accepted indications, absolute dosage recommendations. and other information pertinent to the safe and effective use of the product described. This is especially important when drugs are given in combination or as an adjunct to other forms of therapy Library of Congress Cataloging-in-Publication Data Veterinary anesthesia and pain management secrets / edited by Stephen A. Greene. p. em. - (The Secrets Series®) Includes bibliographical references (p.). ISBN 1-56053-442-7 (alk paper) I. Veterinary anesthesia-Examinations, questions. etc. 2. Pain in animals Treatment-Examinations, questions, etc. I. Greene, Stephen A., 1956-11. Series. SF914.V48 2002 636 089' 796'076--dc2 I 2001039966 VETERINARY ANESTHESIA AND PAIN MANAGEMENT SECRETS ISBN 1-56053-442-7 © 2002 by Hanley & Belfus, Inc. All rights reserved. No part of this book may be repro duced, reused, republished. or transmitted in any form, or stored in a database or retrieval system, without written permission of the publisher Last digit is the print number: 9 8 7 6 5 4 3 2 CONTRIBUTORS G. -

Local Anesthetic Agents Infiltration: Role of the Nurse
Doug Ducey Joey Ridenour Governor Executive Director Arizona State Board of Nursing 1740 W Adams Street, Suite 2000 Phoenix. AZ 85007 Phone (602) 771-7800 Home Page: http://www.azbn.gov OPINION: INFILTRATION OF LOCAL An advisory opinion adopted by AZBN is an interpretation of what the law requires. While an ANESTHETIC AGENTS: THE ROLE OF THE advisory opinion is not law, it is more than a recommendation. In other words, an advisory opinion NURSE is an official opinion of AZBN regarding the practice of nursing as it relates to the functions of APPROVED DATE: 3/2015 nursing. Facility policies may restrict practice further in their setting and/or require additional REVISED DATE: 7/2018 expectations related to competency, validation, training, and supervision to assure the safety of their patient population and or decrease risk. ORIGINATING COMMITTEE: SCOPE OF PRACTICE COMMITTEE Within the Scope of Practice of X RN x LPN ADVISORY OPINION LOCAL ANESTHETIC AGENTS INFILTRATION: ROLE OF THE NURSE It is within the scope of practice of a registered nurse (RN) and a licensed practical nurse (LPN) to administer certain local anesthetic agents intradermal, subcutaneous, and submucosal for the purposes of analgesia and/or anesthesia prior to potentially painful procedures. Tumescent lidocaine infiltration for ambulatory procedures, such as but not limited to, the treatment of hyperhidrosis, ambulatory phlebectomy and laser facial resurfacings would be within the RN scope under the direction of an licensed independent practitioner (LIP) and when certain criteria is met within this advisory opinion. The licensed nurse must meet the general requirements and course of instruction listed in parts I and II.