“All Things Are Poison,” So What Should We Test For? Evaluation of Poisoning and Drug Overdose
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pharmacology/Therapeutics Ii Block 1 Handouts – 2015-16
PHARMACOLOGY/THERAPEUTICS II BLOCK 1 HANDOUTS – 2015‐16 55. H2 Blockers, PPls – Moorman 56. Palliation of Contipation & Nausea/Vomiting – Kristopaitis 57. On‐Line Only – Principles of Clinical Toxicology – Kennedy 58. Anti‐Parasitic Agents – Johnson Histamine Antagonists and PPIs January 6, 2016 Debra Hoppensteadt Moorman, Ph.D. Histamine Antagonists and PPIs Debra Hoppensteadt Moorman, Ph.D. Office # 64625 Email: [email protected] KEY CONCEPTS AND LEARNING OBJECTIVES . 1 To understand the clinical uses of H2 receptor antagonists. 2 To describe the drug interactions associated with the use of H2 receptor antagonists. 3 To understand the mechanism of action of PPIs 4 To describe the adverse effects and drugs interactions with PPIs 5 To understand when the histamine antagonists and the PPIs are to be used for treatment 6 To describe the drugs used to treat H. pylori infection Drug List: See Summary Table. Histamine Antagonists and PPIs January 6, 2016 Debra Hoppensteadt Moorman, Ph.D. Histamine Antagonists and PPIs I. H2 Receptor Antagonists These drugs reduce gastric acid secretion, and are used to treat peptic ulcer disease and gastric acid hypersecretion. These are remarkably safe drugs, and are now available over the counter. The H2 antagonists are available OTC: 1. Cimetidine (Tagamet®) 2. Famotidine (Pepcid®) 3. Nizatidine (Axid®) 4. Ranitidine (Zantac®) All of these have different structures and, therefore, different side-effects. The H2 antagonists are rapidly and well absorbed after oral administration (bioavailability 50-90%). Peak plasma concentrations are reached in 1-3 hours, and the drugs have a t1/2 of 1-3 hours. H2 antagonists also inhibit stimulated (due to feeding, gastrin, hypoglycemia, vagal) acid secretion and are useful in controlling nocturnal acidity – useful when added to proton pump therapy to control “nocturnal acid breakthrough”. -

Tall Man Lettering List REPORT DECEMBER 2013 1
Tall Man Lettering List REPORT DECEMBER 2013 1 TALL MAN LETTERING LIST REPORT WWW.HQSC.GOVT.NZ Published in December 2013 by the Health Quality & Safety Commission. This document is available on the Health Quality & Safety Commission website, www.hqsc.govt.nz ISBN: 978-0-478-38555-7 (online) Citation: Health Quality & Safety Commission. 2013. Tall Man Lettering List Report. Wellington: Health Quality & Safety Commission. Crown copyright ©. This copyright work is licensed under the Creative Commons Attribution-No Derivative Works 3.0 New Zealand licence. In essence, you are free to copy and distribute the work (including other media and formats), as long as you attribute the work to the Health Quality & Safety Commission. The work must not be adapted and other licence terms must be abided. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nd/3.0/nz/ Copyright enquiries If you are in doubt as to whether a proposed use is covered by this licence, please contact: National Medication Safety Programme Team Health Quality & Safety Commission PO Box 25496 Wellington 6146 ACKNOWLEDGEMENTS The Health Quality & Safety Commission acknowledges the following for their assistance in producing the New Zealand Tall Man lettering list: • The Australian Commission on Safety and Quality in Health Care for advice and support in allowing its original work to be either reproduced in whole or altered in part for New Zealand as per its copyright1 • The Medication Safety and Quality Program of Clinical Excellence Commission, New South -

Ideal Conditions for Urine Sample Handling, and Potential in Vitro Artifacts Associated with Urine Storage
Urinalysis Made Easy: The Complete Urinalysis with Images from a Fully Automated Analyzer A. Rick Alleman, DVM, PhD, DABVP, DACVP Lighthouse Veterinary Consultants, LLC Gainesville, FL Ideal conditions for urine sample handling, and potential in vitro artifacts associated with urine storage 1) Potential artifacts associated with refrigeration: a) In vitro crystal formation (especially, calcium oxalate dihydrate) that increases with the duration of storage i) When clinically significant crystalluria is suspected, it is best to confirm the finding with a freshly collected urine sample that has not been refrigerated and which is analyzed within 60 minutes of collection b) A cold urine sample may inhibit enzymatic reactions in the dipstick (e.g. glucose), leading to falsely decreased results. c) The specific gravity of cold urine may be falsely increased, because cold urine is denser than room temperature urine. 2) Potential artifacts associated with prolonged storage at room temperature, and their effects: a) Bacterial overgrowth can cause: i) Increased urine turbidity ii) Altered pH (1) Increased pH, if urease-producing bacteria are present (2) Decreased pH, if bacteria use glucose to form acidic metabolites iii) Decreased concentration of chemicals that may be metabolized by bacteria (e.g. glucose, ketones) iv) Increased number of bacteria in urine sediment v) Altered urine culture results b) Increased urine pH, which may occur due to loss of carbon dioxide or bacterial overgrowth, can cause: i) False positive dipstick protein reaction ii) Degeneration of cells and casts iii) Alter the type and amount of crystals present 3) Other potential artifacts: a) Evaporative loss of volatile substances (e.g. -

Poisoning in Children
ARTICLE IN PRESS Current Paediatrics (2005) 15, 563–568 www.elsevier.com/locate/cupe Poisoning in children Fiona JepsenÃ, Mary Ryan Emergency Medicine, Royal Liverpool Children’s NHS Trust, Alder Hey, Liverpool L12 2AP, UK KEYWORDS Summary Poisoning accounts for about 7% of all accidents in children under 5 Poisoning; years and is implicated in about 2% of all childhood deaths in the developed world, Child; and over 5% in the developing world (National Poisons Information Service). In Accidents; considering this topic, however, it is important to differentiate accidental overdose Home (common in the younger age groups) and deliberate overdose (more common in young adults). Although initial assessment and treatment of these groups may not differ significantly, the social issues and ongoing follow-up of these children will be totally different and the treating physician must remain aware of this difference. The initial identification and treatment of these children remains the mainstay of management, and many ingested substances do not have a specific antidote. Supportive treatment must be planned and the potential for delayed or long-term effects noted. The specific presentation and treatment of some of the commonly ingested substances will be addressed in this article, and guidance given on when to contact expert help. & 2005 Elsevier Ltd. All rights reserved. Introduction such as bleaches, detergents and turpentine sub- stitutes. More than 100 000 individuals are admitted to Toxic compounds may be ingested or inhaled hospital in England and Wales annually due to either accidentally or deliberately. Accidental poisoning, accounting for 10% of all acute admis- poisoning can occur at any age, but is much more 1 sions.1 However, the true incidence of acute common in children. -

Guideline on Antidote Availability for Emergency Departments January 2017
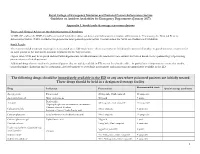
Royal College of Emergency Medicine and National Poisons Information Service Guideline on Antidote Availability for Emergency Departments January 2017 TOXBASE and/or the BNF should be consulted for further advice on doses and indications for antidote administration and, if necessary, the National Poisons Information Service (NPIS) should be telephoned for more patient-specific advice. Contact details for NPIS are available on TOXBASE. Additional drugs that are used in the poisoned patient that are widely available in ED are not listed in the table – in particular it is important to ensure that insulin, benzodiazepines (diazepam and/or lorazepam), glyceryl trinitrate or isosorbide dinitrate and magnesium are immediately available in the ED. The following drugs should be immediately available in the ED or any area where poisoned patients are initially treated. These drugs should be held in a designated storage facility* The stock held should be sufficient to initiate treatment (stocking guidance is in Appendix 1). Drug Indication Acetylcysteine Paracetamol Activated charcoal Many oral poisons Atropine Organophosphorus or carbamate insecticides Bradycardia Calcium chloride Calcium channel blockers Systemic effects of hydrofluoric acid Calcium gluconate Local infiltration for hydrofluoric acid Calcium gluconate gel Hydrofluoric acid Cyanide antidotes Cyanide Dicobalt edetate The choice of antidote depends on the severity of poisoning, certainty of diagnosis and cause Hydroxocobalamin (Cyanokit®) of poisoning/source of cyanide. Sodium nitrite - Dicobalt edetate is the antidote of choice in severe cases when there is a high clinical Sodium thiosulphate suspicion of cyanide poisoning e.g. after cyanide salt exposure. - Hydroxocobalamin (Cyanokit®) should be considered in smoke inhalation victims who have a severe lactic acidosis, are comatose, in cardiac arrest or have significant cardiovascular compromise - Sodium nitrite may be used if dicobalt edetate is not available. -

Interpretation of Canine and Feline Urinalysis
$50. 00 Interpretation of Canine and Feline Urinalysis Dennis J. Chew, DVM Stephen P. DiBartola, DVM Clinical Handbook Series Interpretation of Canine and Feline Urinalysis Dennis J. Chew, DVM Stephen P. DiBartola, DVM Clinical Handbook Series Preface Urine is that golden body fluid that has the potential to reveal the answers to many of the body’s mysteries. As Thomas McCrae (1870-1935) said, “More is missed by not looking than not knowing.” And so, the authors would like to dedicate this handbook to three pioneers of veterinary nephrology and urology who emphasized the importance of “looking,” that is, the importance of conducting routine urinalysis in the diagnosis and treatment of diseases of dogs and cats. To Dr. Carl A. Osborne , for his tireless campaign to convince veterinarians of the importance of routine urinalysis; to Dr. Richard C. Scott , for his emphasis on evaluation of fresh urine sediments; and to Dr. Gerald V. Ling for his advancement of the technique of cystocentesis. Published by The Gloyd Group, Inc. Wilmington, Delaware © 2004 by Nestlé Purina PetCare Company. All rights reserved. Printed in the United States of America. Nestlé Purina PetCare Company: Checkerboard Square, Saint Louis, Missouri, 63188 First printing, 1998. Laboratory slides reproduced by permission of Dennis J. Chew, DVM and Stephen P. DiBartola, DVM. This book is protected by copyright. ISBN 0-9678005-2-8 Table of Contents Introduction ............................................1 Part I Chapter 1 Sample Collection ...............................................5 -
RCEM NPIS Antidote Guideline Appx 1
Royal College of Emergency Medicine and National Poisons Information Service Guideline on Antidote Availability for Emergency Departments (January 2017) Appendix 1. Stock levels & storage recommendations Doses and Clinical Advice on the Administration of Antidotes TOXBASE and/or the BNF should be consulted for further advice on doses and indications for antidote administration. If necessary, the National Poisons Information Service (NPIS) should be telephoned for more patient-specific advice. Contact details for NPIS are available on TOXBASE. Stock Levels The recommended minimum stocking levels (rounded up to full “pack-sizes” where necessary) are based on the amount of antidote required to initiate treatment for an adult patient in the ED and to continue treatment for the first 24 hours. Higher stock levels may be required and individual departments should determine the amount of each antidote they stock based on the epidemiology of poisoning presentations to their department. Additional drugs that are used in the poisoned patient that are widely available in ED are not listed in the table – in particular it is important to ensure that insulin, benzodiazepines (diazepam and/or lorazepam), glyceryl trinitrate or isosorbide mononitrate and magnesium are immediately available in the ED. The following drugs should be immediately available in the ED or any area where poisoned patients are initially treated These drugs should be held in a designated storage facility Recommended stock Drug Indication Presentation Special storage conditions -

Depletion of Trace Elements and Acute Ocular Toxicity Induced by Desferrioxamine in Patients with Thalassaemia
Arch Dis Child: first published as 10.1136/adc.63.3.250 on 1 March 1988. Downloaded from Archives of Disease in Childhood, 1988, 63, 250-255 Depletion of trace elements and acute ocular toxicity induced by desferrioxamine in patients with thalassaemia S DE VIRGILIIS, M CONGIA, M P TURCO, F FRAU, C DESSI, F ARGIOLU, R SORCINELLI,* A SITZIA,* AND A CAO Istituto di Clinica e Biologia dell Eta' Evolutiva, Universita' Studi Cagliari, and *Istituto di Clinica Oculistica, Universita' Studi Cagliari, Cagliari, Sardinia, Italy SUMMARY High doses of intravenous desferrioxamine infused over a short period of time induce a large faecal and urinary iron excretion but also produce retinal abnormalities that are characterised by decreased amplitude on electroretinography and defective dark adaptation. This regimen also results in high faecal iron, zinc, and copper excretion, and reduced granulocyte zinc concentrations and alkaline phosphatase activity. The retinal abnormalities may be related to the zinc and copper deficiency and/or iron depletion 'per se' which interferes negatively with critical iron dependent enzymes. Subcutaneous infusion of desferrioxamine is the comply with the regimen of subcutaneous adminis- most efficient method for reducing the iron burden tration. in patients with thalassaemia major who are trans- fusion dependent.1 The daily infusion of 40- Patients and methods 60 mg/kg over 12 hours for six days a week is usually sufficient to obtain iron balance.'v Because some Fifteen children, aged from 9 to 16 years, with http://adc.bmj.com/ -

Critical Care Nursing of Infants and Children Martha A
University of Pennsylvania ScholarlyCommons Miscellaneous Papers Miscellaneous Papers 1-1-2001 Critical Care Nursing of Infants and Children Martha A. Q. Curley University of Pennsylvania, [email protected] Patricia A. Moloney-Harmon The Children's Hospital at Sinai Copyright by the author. Reprinted from Critical Care Nursing of Infants and Children, Martha A.Q. Curley and Patricia A. Moloney-Harmon (Editors), (Philadelphia: W.B. Saunders Co., 2001), 1,128 pages. NOTE: At the time of publication, the author, Martha Curley was affiliated with the Children's Hospital of Boston. Currently, she is a faculty member in the School of Nursing at the University of Pennsylvania. This paper is posted at ScholarlyCommons. http://repository.upenn.edu/miscellaneous_papers/4 For more information, please contact [email protected]. Please Note: The full version of this book and all of its chapters (below) can be found on ScholarlyCommons (from the University of Pennsylvania) at http://repository.upenn.edu/miscellaneous_papers/4/ Information page in ScholarlyCommons Full book front.pdf - Front Matter, Contributors, Forward, Preface, Acknowledgements, and Contents Chapter 1.pdf - The Essence of Pediatric Critical Care Nursing Chapter 2.pdf - Caring Practices: Providing Developmentally Supportive Care Chapter_3.pdf - Caring Practices: The Impact of the Critical Care Experience on the Family Chapter_4.pdf - Leadership in Pediatric Critical Care Chapter 5.pdf - Facilitation of Learning Chapter_6.pdf - Advocacy and Moral Agency: A Road Map for -

Chelation Therapy
Corporate Medical Policy Chelation Therapy File Name: chelation_therapy Origination: 12/1995 Last CAP Review: 2/2021 Next CAP Review: 2/2022 Last Review: 2/2021 Description of Procedure or Service Chelation therapy is an established treatment for the removal of metal toxins by converting them to a chemically inert form that can be excreted in the urine. Chelation therapy comprises intravenous or oral administration of chelating agents that remove metal ions such as lead, aluminum, mercury, arsenic, zinc, iron, copper, and calcium from the body. Specific chelating agents are used for particular heavy metal toxicities. For example, desferroxamine (not Food and Drug Administration [FDA] approved) is used for patients with iron toxicity, and calcium-ethylenediaminetetraacetic acid (EDTA) is used for patients with lead poisoning. Note that disodium-EDTA is not recommended for acute lead poisoning due to the increased risk of death from hypocalcemia. Another class of chelating agents, called metal protein attenuating compounds (MPACs), is under investigation for the treatment of Alzheimer’s disease, which is associated with the disequilibrium of cerebral metals. Unlike traditional systemic chelators that bind and remove metals from tissues systemically, MPACs have subtle effects on metal homeostasis and abnormal metal interactions. In animal models of Alzheimer’s disease, they promote the solubilization and clearance of β-amyloid protein by binding to its metal-ion complex and also inhibit redox reactions that generate neurotoxic free radicals. MPACs therefore interrupt two putative pathogenic processes of Alzheimer’s disease. However, no MPACs have received FDA approval for treating Alzheimer’s disease. Chelation therapy has also been investigated as a treatment for other indications including atherosclerosis and autism spectrum disorder. -

Cardiotoxicity of Doxorubicin Is Mediated Through Mitochondrial Iron Accumulation
Cardiotoxicity of doxorubicin is mediated through mitochondrial iron accumulation Yoshihiko Ichikawa, … , Tejaswitha Jairaj Naik, Hossein Ardehali J Clin Invest. 2014;124(2):617-630. https://doi.org/10.1172/JCI72931. Research Article Cardiology Doxorubicin is an effective anticancer drug with known cardiotoxic side effects. It has been hypothesized that doxorubicin- dependent cardiotoxicity occurs through ROS production and possibly cellular iron accumulation. Here, we found that cardiotoxicity develops through the preferential accumulation of iron inside the mitochondria following doxorubicin treatment. In isolated cardiomyocytes, doxorubicin became concentrated in the mitochondria and increased both mitochondrial iron and cellular ROS levels. Overexpression of ABCB8, a mitochondrial protein that facilitates iron export, in vitro and in the hearts of transgenic mice decreased mitochondrial iron and cellular ROS and protected against doxorubicin-induced cardiomyopathy. Dexrazoxane, a drug that attenuates doxorubicin-induced cardiotoxicity, decreased mitochondrial iron levels and reversed doxorubicin-induced cardiac damage. Finally, hearts from patients with doxorubicin-induced cardiomyopathy had markedly higher mitochondrial iron levels than hearts from patients with other types of cardiomyopathies or normal cardiac function. These results suggest that the cardiotoxic effects of doxorubicin develop from mitochondrial iron accumulation and that reducing mitochondrial iron levels protects against doxorubicin- induced cardiomyopathy. Find the latest version: https://jci.me/72931/pdf Research article Cardiotoxicity of doxorubicin is mediated through mitochondrial iron accumulation Yoshihiko Ichikawa,1 Mohsen Ghanefar,1 Marina Bayeva,1 Rongxue Wu,1 Arineh Khechaduri,1 Sathyamangla V. Naga Prasad,2 R. Kannan Mutharasan,1 Tejaswitha Jairaj Naik,1 and Hossein Ardehali1 1Feinberg Cardiovascular Institute, Northwestern University School of Medicine, Chicago, Illinois, USA. -

Fomepizole for Acetaminophen Toxicity
Clinical Pharmacology & Toxicology Pearl of the Week Fomepizole for Acetaminophen Toxicity Mechanisms There are two ways that fomepizole works to help prevent hepatotoxicity in APAP overdose. The primary mechanism involves inhibition of CYP450 2E1. o When a toxic amount of APAP is ingested, the pathways that convert it into nontoxic metabolites become overwhelmed. o Thus, more APAP gets converted into NAPQI. o Fomepizole inhibits the 2E1 pathway, thus preventing conversion of APAP into NAPQI. The second mechanism of action is the JNK (“junk”) enzyme. o NAPQI-induced mitochondrial dysfunction leads to formation of reactive oxidant species. This oxidant stress leads to activation of c-jun N-terminal kinase, or JNK, enzyme. o This enzyme translocates to the mitochondria, amplifying oxidant stress, and ultimately resulting in the cessation of ATP production. o Additionally, the JNK enzyme can lead to the rupture of the outer mitochondrial membrane, causing release of intermembrane proteins, which can potentially lead to DNA fragmentation o Interestingly, it is thought that both metabolic acidosis, as well as elevated lactate levels, may be the result of alterations in mitochondrial respiratory function o Fomepizole works by preventing the APAP-induced activation of this enzyme. Role in Acetaminophen poisoning management In cases where fomepizole and NAC were administered together, evidence has shown that the combination has contributed to a decrease in both hepatotoxicity and mortality. Most of the evidence has come from case reports and animal models. Currently, fomepizole is recommended for massive APAP ingestions (as in, ingestions over 500- 600 mg/kg or in cases where 4-hour equivalent acetaminophen concentrations over 5000 umol/L).