Bakhle, Mick: Transcript of an Audio Interview (10-Aug-2016)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Universities (PDF 183.65
University of Leeds Classification of Books Universities No longer used : see Education 378 [A General] A-0.01 periodicals A-0.02 series A-0.03 collections of essays, Festschriften etc. A-0.04 bibliography A-0.07 Academic dress A-1 General [B University education] B-1 General B-2 Methods B-2.1 Selection B-2.2 Students; students' guides; student services B-2.3 Teaching methods; Curriculum B-2.5 Degrees & other awards B-3 Universities & the community B-3.1 University graduates [C University administration] C-1 General C-1.5 University libraries See also Bibliography H-2.4 C-2 Finance C-3 Staffing C-3.5 Association of University Teachers C-4 Planning (includes architectural aspects) [D-R History & studies of universities] D-0 General D-1 Regional Divided geographically to country level e.g. England D-1.1 Individual universities in E-R [E England] E-1 London E-2 Royal Veterinary College E-3 Birkbeck College E-4 University College London E-5 King's College E-6 School of Pharmacy E-6.3 Chelsea College E-7 Bedford College E-8 Westfield College E-9 Royal Holloway College E-10 Queen Mary College E-11 Wye College E-12 London School of Economics and Political Science E-13 Imperial College of Science, Technology & Medicine E-14 Queen Elizabeth College E-15 School of Oriental and African Studies E-16 City University E-17 Brunel University E-21 University of Surrey E-23 University of Kent at Canterbury E-25 University of Sussex E-27 University of Southampton E-29 University of Reading E-35 University of Exeter E-38 University of Bath E-41 University -
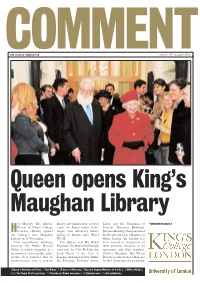
Commentthe College Newsletter Issue No 144 | December 2002
COMMENTTHE COLLEGE NEWSLETTER ISSUE NO 144 | DECEMBER 2002 DOMINIC TURNER Queen opens King’s Maughan Library er Majesty The Queen, library and information services Lucas and the Chairman of Continued on page 2 Patron of King’s College centre for King’s makes it the Council, Baroness Rawlings. HLondon, officially opened largest new university library Baroness Rawlings then presented the College’s new Maughan facility in Britain since World Sir Deryck and Lady Maughan, in Library on 14 November. War II. whose honour the Library has This magnificent building, The Queen and His Royal been named in recognition of formerly the Public Record Highness The Duke of Edinburgh their generous donation to its Office, is widely regarded as a were met by The Rt Hon the restoration, and their daughter, masterpiece of neo-gothic archi- Lord Mayor of the City of Chelsea Maughan. Mrs Vivien tecture. It is believed that its London, Alderman Gavyn Arthur, Robertson, Site Services Manager transformation into a modern the Principal, Professor Arthur for the Library, was also presented. 2 Queen’s Anniversary Prize | 3 Tom Ridge | 4 25 years of Nursing | 5 Russian Deputy Minister of Justice | 6 DNA at King’s | 8 & 9 The Royal Visit in pictures | 13 Flashback: Nobel Laureates | 15 Student news | 16 Art exhibitions News those at Shrivenham) and a which has so far been spectacu- Letter from the King’s wins turnover of £2 million. larly successful. War Studies is one of only Chairman of Council My fellow Council members Queen’s prize two such departments in the and senior officers await with country to be consistently The highlight of this term for me great interest new Government ing’s has been awarded a awarded the highest rating over was the opening of the Maughan plans for higher education which prestigious Queen’s Anni- the last three RAEs, and in 2001 Library by HM The Queen and are due to be unveiled in Jan- versary Prize for Higher and both the Departments of War HRH The Duke of Edinburgh. -

Title Pub Date Note Edrs Price Abstract
DOCUMENT RESUME ED 067 101 LI 003 839 TITLE Report of the Committee on Library Resources. INSTITUTION London Univ. (England). PUB DATE 71 NOTE 250p.;(0 References) AVAILABLE FROMPublications Dept. University of London, The Senate House, Malet Street, WCIE 7HU, London, England EDRS PRICE MF-$0.65 HC Not Available from EDRS. DESCRIPTORS Archives; *Financial Policy; Foreign Countries; Graduate Study; Librarians; *Library Collections; *Library Se:vices; *Medical Libraries; Personnel Policy; Resources; Undergraduate Study; *University Libraries IDENTIFIERS England; *Library Resources ABSTRACT The University of London appointed a committee with the charge to investigate the library provisions and conditions within the University in relation to the library resources of the London area in general; to explore the possibilities of increased co-ordination and co-operation between these libraries; and to make recommendations on all aspects of library policy. This report of the committee looks at and makes recommendations for the following: library resources of the University and of the London area in general; provision for undergraduate studies, advanced study and research; medical libraries; manuscripts and archives; central library services; staffing the Libraries Council; and, finance and accommodation. (Author/SJ) UNIVERSITY OF LONDON Report of the Committee on Library Resources U.S. DEPARTMENT OF HEALTH, "PERMISSION TO REPRODUCETHIS COPY RIGHTED MATERIAL BY MICROFICHEONLY EDUCATION & WELFARE HAS BEE'. SRADITED 8Y OFFICE OF EDUCATION THIS DOCUMENT HAS BEEN REPRO- -th_t114 MI.Ver 047 DUCED EXACTLY AS RECEIVED FROM THE PERSON OR ORGANIZATION ORIG. or Le 10 ERIC AND ORGANIZATIONS INATING IT. POINTS OF VIEW OR OPIN OPERATING UNDER AGREEMENTS WITH IONS STATED DO NOT NECESSARILY OF EDUCATION THE US OFFICE REPRESENT OFFICIAL OFFICE OF EDU- FURTHER REPRODUCTION OUTSIDE THE ERIC SYSTEMREQUIRES PER CATION POSITION OR POLICY. -

Women Physiologists
Women physiologists: Centenary celebrations and beyond physiologists: celebrations Centenary Women Hodgkin Huxley House 30 Farringdon Lane London EC1R 3AW T +44 (0)20 7269 5718 www.physoc.org • journals.physoc.org Women physiologists: Centenary celebrations and beyond Edited by Susan Wray and Tilli Tansey Forewords by Dame Julia Higgins DBE FRS FREng and Baroness Susan Greenfield CBE HonFRCP Published in 2015 by The Physiological Society At Hodgkin Huxley House, 30 Farringdon Lane, London EC1R 3AW Copyright © 2015 The Physiological Society Foreword copyright © 2015 by Dame Julia Higgins Foreword copyright © 2015 by Baroness Susan Greenfield All rights reserved ISBN 978-0-9933410-0-7 Contents Foreword 6 Centenary celebrations Women in physiology: Centenary celebrations and beyond 8 The landscape for women 25 years on 12 "To dine with ladies smelling of dog"? A brief history of women and The Physiological Society 16 Obituaries Alison Brading (1939-2011) 34 Gertrude Falk (1925-2008) 37 Marianne Fillenz (1924-2012) 39 Olga Hudlická (1926-2014) 42 Shelagh Morrissey (1916-1990) 46 Anne Warner (1940–2012) 48 Maureen Young (1915-2013) 51 Women physiologists Frances Mary Ashcroft 56 Heidi de Wet 58 Susan D Brain 60 Aisah A Aubdool 62 Andrea H. Brand 64 Irene Miguel-Aliaga 66 Barbara Casadei 68 Svetlana Reilly 70 Shamshad Cockcroft 72 Kathryn Garner 74 Dame Kay Davies 76 Lisa Heather 78 Annette Dolphin 80 Claudia Bauer 82 Kim Dora 84 Pooneh Bagher 86 Maria Fitzgerald 88 Stephanie Koch 90 Abigail L. Fowden 92 Amanda Sferruzzi-Perri 94 Christine Holt 96 Paloma T. Gonzalez-Bellido 98 Anne King 100 Ilona Obara 102 Bridget Lumb 104 Emma C Hart 106 Margaret (Mandy) R MacLean 108 Kirsty Mair 110 Eleanor A. -

Magdalene College Magazine 2019-20
magdalene college magdalene magdalene college magazine magazine No 63 No 64 2018–19 2019 –20 M A G D A L E N E C O L L E G E The Fellowship, October 2020 THE GOVERNING BODY 2020 MASTER: Sir Christopher Greenwood, GBE, CMG, QC, MA, LLB (1978: Fellow) 1987 PRESIDENT: M E J Hughes, MA, PhD, Pepys Librarian, Director of Studies and University Affiliated Lecturer in English 1981 M A Carpenter, ScD, Professor of Mineralogy and Mineral Physics 1984 J R Patterson, MA, PhD, Praelector, Director of Studies in Classics and USL in Ancient History 1989 T Spencer, MA, PhD, Director of Studies in Geography and Professor of Coastal Dynamics 1990 B J Burchell, MA and PhD (Warwick), Joint Director of Studies in Human, Social and Political Sciences and Professor in the Social Sciences 1990 S Martin, MA, PhD, Senior Tutor, Admissions Tutor (Undergraduates), Joint Director of Studies and University Affiliated Lecturer in Mathematics 1992 K Patel, MA, MSc and PhD (Essex), Director of Studies in Land Economy and UL in Property Finance 1993 T N Harper, MA, PhD, College Lecturer in History and Professor of Southeast Asian History (1990: Research Fellow) 1994 N G Jones, MA, LLM, PhD, Director of Studies in Law (Tripos) and Reader in English Legal History 1995 H Babinsky, MA and PhD (Cranfield), Tutorial Adviser (Undergraduates), Joint Director of Studies in Engineering and Professor of Aerodynamics 1996 P Dupree, MA, PhD, Tutor for Postgraduate Students, Joint Director of Studies in Natural Sciences and Professor of Biochemistry 1998 S K F Stoddart, MA, PhD, Director -

K/INV Invitations and Tickets K/INV1 Dinners
King's College London Archives K/INV Invitations and Tickets K/INV1 Dinners K/INV1/1 1948 May 4 Invitation from the Principal of King's College London and President of the Old Student's Association inviting Miss E. R. B. Rhodes to the Graduation Dinner held at the College on Tuesday 4 May 1948 K/INV1/2 1955 Jun 17 Blank invitation from the Principal of King's College London to the Fellows' Dinner, held in the College on Friday 17 June 1955 K/INV1/3 1956 Jun 15 Blank invitation from the Principal of King's College London to the Fellows' Dinner, held in the College on Friday 15 June 1956 K/INV1/4 1958 Blank invitation from the Principal of King's College London and the President of the King's College London Association, to one of the Graduation Dinners, held in the College on Monday 17 March and Tuesday 13 May 1958 K/INV1/5 1958 Jun 13 Blank invitation from the Principal and Dean of King's College London to the Fellows' Dinner, held in the College on Friday 13 June 1958 K/INV1/6 1959 Blank invitation from the Principal of King's College London and the President of the King's College London Association, to one of the Graduation Dinners, held in the College on Tuesday 17 March and Tuesday 12 May 1959 K/INV1/7 1959 Jun 12 Blank invitation from the Principal and Dean of King's College London to the Fellows' Dinner, held in the College on Friday 12 June 1959 K/INV1/8 1960 Blank invitation from the Principal of King's College London and the President of the King's College London Association, to one of the Graduation Dinners, held in the College on Tuesday 15 March and Tuesday 10 May 1960. -
Date Year Name Name Changes/Notes Date Sealed Ref
Date Year Name Name Changes/Notes Date Sealed Ref. 1231 University of Cambridge 1248 University of Oxford 1272 Saddlers Company 28-May 1284 Peterhouse, Cambridge 10-Mar 1326 Merchant Taylors Company 01-Mar 1327 Skinners Company 06-Mar 1327 Mayor and Commonalty and Citizens of the City of London 1327 Goldsmiths Company 06-Aug 1348 Dean and Canons of Windsor 1348 Gonville and Caius College, Cambridge 30-Jun 1379 New College, Oxford 1382 Winchester College 13-Jan 1393 Mercers Company 04-Dec 1416 Cutlers Company 16-Feb 1428 Grocers Company 22-Feb 1437 Brewers Company 23-Aug 1437 Vintners Company 26-Apr 1439 Cordwainers Company 1444 Leathersellers Company 1448 Queen's College of St Margaret and St Bernard, Cambridge Commonly known as 513 C993 08-May 1453 Armourers Company 17.06.1708 Company of C996 13-Oct 1457 Magdalen College, Oxford 08-Mar 1462 Tallow Chandlers Company 1462 Barbers Company 20-Mar 1463 Ironmongers Company 16-Feb 1471 Dyers Company 20-Jan 1473 Pewterers Company Commonly known as C495(2) 1474 Corporation of Blacksmith's of Dublin 16-Aug 1475 St. Catharine's College, Cambridge 07-Jul 1477 Carpenters Company 16-Feb 1484 The Wax Chandlers Company "Master, Wardens and C651 Commonalty of the Art or Mistery of Wax Chandlers" commonly known as "Worshipful Company of Wax Chandlers" 1496 Jesus College, Cambridge Date Year Name Name Changes/Notes Date Sealed Ref. 10-Mar 1501 Plaisterers Company 29-Apr 1501 Coopers Company 23-Feb 1504 Poulters Company 22-Jul 1509 Bakers Company 15-Jan 1512 Brasenose College, Oxford 1517 Corpus Christi -
Felix Issue 0307, 1972
I.C. to lose UGC grants access Imperial College will lose its right to go direct to the University Grants Committee for its money if th» NEWSPAPER OF IMPERIAL COLLEGE UNION Murray Report on the Governance of the University of 14th November, 1972 FREE! ISSUE No. 318 London, published today, is implemented. At present, Imperial is treated differently to other colleges of the University, whose grants are determined by the Court of the University. Until now, we have gone direct to the UGC independently of other colleges. This was because the Government gave the college national responsibility for the development of scientific and technological teaching. The report says: Senate and the Court for "We understand that Planning and Develop- this treatment (direct ac- ment. cess to the UGC) has been At the time of going to extended by the Univer- press (Sunday 8 p.m.) the sity Grants Committee to Editor of Felix was the the end of the 1972-77 only person in the Col- quinquennium butt is then lege to have seen a copy to be reviewed in the light of the Report. It of our Report. Unless is not easy to judge what there are grounds of Gov- the reaction will be. In ernment or University early 1971, Judith Walk- Grants Committee policy, er, then President of such as were mentioned in I.C.U., sent the Murray Sir John Wolfenden's let- Committee a strongly ter in 1966, for continuing worded letter saying that this treatment, we can, for "Imperial College fought our part, see no special hard for this privilege and reason why Imperial Col- would not wish to sacri- lege, as a constituent fice this independent posi- School of the University, tion." should be treated differ- In the same letter Miss ently from the other Walker decried the "cum- Schools whose grants are bersome, over-bureaucra- determined by the Court tic machinery" of the of the University." University and said that The University of London is, to say the least, a complex institution. -

Record of Charters Granted
Date Year Name Name Changes/Notes Date Sealed 1231 University of Cambridge 1248 University of Oxford 1272 Saddlers Company 28-May 1284 Peterhouse, Cambridge 10-Mar 1326 Merchant Taylors Company 1-Mar 1327 Skinners Company 6-Mar 1327 Mayor and Commonalty and Citizens of the City of London 1327 Goldsmiths Company 6-Aug 1348 Dean and Canons of Windsor 1348 Gonville and Caius College, Cambridge 30-Jun 1379 New College, Oxford 1382 Winchester College 13-Jan 1393 Mercers Company 4-Dec 1416 Cutlers Company 16-Feb 1428 Grocers Company 22-Feb 1437 Brewers Company 23-Aug 1437 Vintners Company 26-Apr 1439 Cordwainers Company 1444 Leathersellers Company The Wardens and Society of the Mistery or Art of the Leathersellers of the City of London (Charter 1604) Date Year Name Name Changes/Notes Date Sealed 1448 Queen's College of St Margaret and St Bernard, Cambridge Commonly known as "Queens' College, Cambridge" 8-May 1453 Armourers Company 17.06.1708 Company of Armourers and Brasiers in the City of London 13-Oct 1457 Magdalen College, Oxford 8-Mar 1462 Tallow Chandlers Company 1462 Barbers Company 20-Mar 1463 Ironmongers Company 16-Feb 1471 Dyers Company 20-Jan 1473 Pewterers Company Commonly known as "Worshipful Company of Pewterers" 1474 Corporation of Blacksmith's of Dublin 16-Aug 1475 St. Catharine's College, Cambridge 7-Jul 1477 Carpenters Company 16-Feb 1484 The Wax Chandlers Company "Master, Wardens and Commonalty of the Art or Mistery of Wax Chandlers" commonly known as "Worshipful Company of Wax Chandlers" 1496 Jesus College, Cambridge 10-Mar -

An Introduction to the King's-Crick Partnership
Introduction to the King’s-Crick Partnership Professor Malcolm Irving and Dr Karen Liu King’s College London History of King’s • Founded 1829 • 4th oldest university in England • Founding member of University of London 1836 • 12 Nobel prize winners King's professors played a major part in nineteenth-century science and in extending higher education to women and working men through evening classes. The university has grown and developed through mergers with several institutions, each with their own distinguished histories. These include: United Medical and Dental Schools of Guy's and St Thomas' Hospitals Chelsea College Queen Elizabeth College Institute of Psychiatry King’s by Numbers 21st in QS world rankings 5 London campuses • Strand Campus • Waterloo Campus • Guy's Campus • Denmark Hill Campus • St. Thomas’ Campus 29,600 students from 150 countries 8,027 employees 11,750 postgraduate students 4 MRC centres • King’s has four Medical Research Council (MRC) centres • Member of King's Health Partners Academic Health Sciences Centre • 84 per cent of research is world-leading or internationally excellent (2014 Research Excellence Framework) Academic Faculties at King’s Faculties at King’s Affiliated with the Crick Dental Institute (DI) Faculty of Life Sciences and Medicine (FoLSM) Institute of Psychiatry, Psychology and Neuroscience (IoPPN) Faculty of Natural and Mathematical Science (NMS) Your PhD Team at King’s and the Crick • King’s-Crick • Associate Research Director Academic Lead with responsibility for Career (Malcolm Irving) Development and Training Crick (John Diffley) • King’s Crick PhD Programme Lead • Director of Studies and (Dr Karen Liu) Academic Programmes • KCL Administrative (Sally Leevers) Lead • Postgraduate Studies Manager (Jennifer Tomomitsu) (Caroline Ransom) • King’s Supervisors King’s Core Team King’s Student Faculties Professional Services Services Our Campuses Guy’s Campus London Bridge Strand Campus Waterloo Campus St. -

SCONUL Focus 32.Indd
SCONUL Focus Number 32 Summer/Autumn 2004 Contents ISSN 1745-5782 3 Coming into Focus 4 Innovative library induction – introducing the ‘Cephalonian Method’ Nigel Morgan, Linda Davies, 9 Access management: the new information skill? Sally Chambers 12 First steps: piloting WebCT at WIT Nora Hegarty 15 Launch of Cambridge graduate trainees’ website Louisa Evans 16 On becoming Fryed: a report from the Frye Leadership Institute Maggie Fieldhouse 18 INSPIRE – a progress report on the national access and referral scheme Yvonne Hamblin 21 INPSPIRE in the West Midlands – tarmac or tracks? Caroline Rock 24 From recommendations to practice – the next steps towards open access David C. Prosser 28 ResIN: Research Information at Newcastle University Library Moira Bent 31 RLG Cultural Materials Alliance – building a cultural resource together Ricky Erway 34 100 years of forestry information from Oxford Roger Mills 40 A new intellectual property information service for Wales: Swansea University Library joins the PATLIB network Julie Allan 42 Developing a marketing orientation at the British Library Jill Finney, Gary Warnaby 45 Peer evaluation: putting libraries back on the inspection map Steve Cropper 47 Just for txtin’?: a mobile phone use survey Jane Harrington, Carole Symes 49 Self-service in academic libraries: a survey of current practice Philippa Jones 51 Virtually there: virtual learning environments and libraries Reviewed by Elizabeth Charles 52 New professionals at the Gregynog Colloquium, Reviewed by Neil Smyth 53 News from SCONUL Toby Bainton 55 The Open Rose Group: opening up access for disabled users of academic libraries in Yorkshire. Christopher Beevers, Lois Burt, Paul Conway 57 ACOSC Digest of Scholarly Communication News Fredrick J. -

K/ART Artefacts Draft Catalogue
King's College London Archives K/ART - Artefacts This collection consists of various material objects and some printed matter relating to King’s College London and its history. The material is diverse and notably includes printing blocks, College regalia and prizes. K/ART1 [1900] 2 unlabelled metal and wood printing blocks (13.5cm x 20.5cm) signed 'Sedgwick' and bearing different photographic images of industrial machinery, possibly the interior of the King's College London Engineering Department. 2 items K/ART2 [1900] Unlabelled metal and wood printing block (9cm x 12cm) bearing a photographic image of a King's College London laboratory, possibly in the Biology Department K/ART3 [1900] Metal and wood printing block (9cm x 12cm) bearing a photographic image of a King's College London laboratory, possibly in the Chemistry Department. The reverse of the block shows a copy of the printed image and is labelled 'King's College' K/ART4 [1900] Unlabelled metal and wood printing block (21cm x 12.5cm) signed 'Sedgwick' and bearing a photographic image of students working with tools and equipment, possibly in the King's College London Engineering workshop K/ART5 [1900] Unlabelled metal and wood printing block (12cm x 10cm) bearing a photographic image of the interior of a King's College London class room or laboratory, with book shelves and portraits on the walls K/ART6 [1900] Metal and wood printing block (10.5cm x 8cm) labelled 'King's College Xmas Card on A/C of Mr Gregory [C] Macmillan and Co' and bearing a photographic image of the exterior