COTH E-News Summer 2019
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fixmil M COMMERCIAL
8 WEVV 1UJUK HEltALD, TUESDAY, 5jjfirrJSMBEK 16, 1879..TRIP]uE SHEET. were aud to new fouri, 108'4' for and 108»i for now Area lonoo 81 LASF 2d,cl B 58 200 do. b60 8'< """ » irregular.generally higher at the opeulr.g, but Kant Imlia, in bond, 80c. a Rjc. per gallon, arrive, limm SlL J6 IM.ArU br ml 1 H"0 do«? IS £ JSa-lteiilHI |S I closing easier. Tho sales. including 4.V».<JOt> bushels for 75c. u HOc. securities at 27for Erie com t% future wore American railway Sirm l.ouAXolt lKt.bc lot 2O0 do o deliverv. 725.<MMJ busbwls. at If I l."»a$A l« for . 8J5 No. for preferred. 7«¥ tor the new seconiI Bllt pit* American Ex.. 47K jr. K * Dop Moliien.bc 14 S& 2rud.$l 15a$l 10 for do. do. ror September, $1 IV4 m men, 50lj Atlmij* ' do 10 a #1 IB for do. do. tor a for do. do. DOMESTIC MARKETS. COMMERCIAL Km do III) fIXMIL i'» KipNM.be 102.S 14\ * HS>, lU>Chw*OJdpr....«. £; October. #1 15;\ $1 IB>4 for consols, 74U for funded lives. 114V, for confcolidateiI luut'mitoii. 42 Km <o do KM 10O MhiiUhUdu. -M'k November. SI IB a *1 17 for No. 1 white. $1 1"»?£ a Oalvkston. Kept 13, 1X79. do be 42 Km } *!' Uo * 10 X Y Klevatad la.> $1 UV\ tor do. do. tor for J IB lutr 10\c.; firsts, 44 for 1'oimaylvalue,1 54 for New Jersey Cen im) do 14' ' H8J, October, $1 14 No. -
Hoping for a Return on Investment in the Cowlitz Pete Caster / [email protected] Judy C
Celebrating the Swedes Large Crowds Flock to Rochester to Let Their Inner Viking Out / Main 3 Hiker Found Dead / Main 5 $1 Early-Week Edition Tuesday, June 24, 2014 Reaching 110,000 Readers in Print and Online — www.chronline.com Hoping for a Return on Investment in the Cowlitz Pete Caster / [email protected] Judy C. Chain sits with her attorney, Sam Experimental Run of Salmon, Net Pens to Yield Better Harvest Groberg, during the irst day of her trial in Lewis County Superior Court on Monday. Trial for ‘Rising Son’ Head Starts ACCUSED: Judy Chafin Faces 30 Felony Charges for Allegedly Collecting $90,000 From Labor and Industries While Running the Controversial Group of Halfway Houses By Stephanie Schendel [email protected] At the peak of the House of the Rising Son organization, Judy Cha- fin ran numerous halfway houses for recently released convicts throughout Pete Caster / [email protected] Lewis County. Mossyrock Fish Hatchery Supervisor Tim Summers feeds fall chinook on Monday morning at the Mayield Net Pen Project at Silver Creek. The Washington De- She collected rent, went grocery partment of Fish and Wildlife is raising nearly 2 million fall chinook in these pins. The ish will eventually be released in the lower Cowlitz River near the salmon shopping for the tenants, enforced hatchery. house rules and dealt with all finan- cial transactions of the business. All FISH STORY: Money Secured in Part by Sen. John the while, she was allegedly collect- Braun Put to Use on Mayfield Lake ing disability checks from the De- partment of Labor and Industries, By Dameon Pesanti claiming she was unable to work. -

Godsmack | Primary Wave Music
GODSMACK facebook.com/Godsmack instagram.com/godsmack twitter.com/godsmack Imageyoutube.com/channel/UCe9rl8k6yymUeVzzXfFGWwA not found or type unknown godsmack.com en.wikipedia.org/wiki/Godsmack open.spotify.com/artist/6gZq1Q6bdOxsUPUG1TaFbF According to Greek mythology, the phoenix absorbs new life through rising from the ashes of its predecessor. By the same token, we tear down the relics of the past in order to make way for the innovations of the future. As every rebirth requires reinvention, GODSMACK— Sully Erna [vocals, guitar], Tony Rombola [guitar], Robbie Merrill [bass], and Shannon Larkin [drums]–continue a similar cycle on their seventh full-length and debut for BMG, When Legends Rise. The multiplatinum four-time GRAMMY® Award-nominated Boston bastion of hard rock raises its voice louder than ever on their first album in four years. “You’ve got to burn it down to build it up,” affirms Erna. “When Legends Rise is a metaphor. Life can get challenging at times. It can knock you onto the ground. However, if you reach inside of yourself, find that inner strength, and rise up again, you’ll flourish. Over the past few years, I went through a really tough time, but I learned this firsthand. Coming out on the other side, we’re going to do this bigger and better than we ever have. We’re ready to work.” Truth is, the members of GODSMACK have never been afraid to put in the work… Like the city they call home, these musicians speak louder, fight harder, and grow stronger each day. Through an uncompromising attitude and uncanny knack for a hummable hook, they quietly became one of modern rock’s most reliable and resonant institutions. -
AUDIO + VIDEO 4/13/10 Audio & Video Releases *Click on the Artist Names to Be Taken Directly to the Sell Sheet
NEW RELEASES WEA.COM ISSUE 07 APRIL 13 + APRIL 20, 2010 LABELS / PARTNERS Atlantic Records Asylum Bad Boy Records Bigger Picture Curb Records Elektra Fueled By Ramen Nonesuch Rhino Records Roadrunner Records Time Life Top Sail Warner Bros. Records Warner Music Latina Word AUDIO + VIDEO 4/13/10 Audio & Video Releases *Click on the Artist Names to be taken directly to the Sell Sheet. Click on the Artist Name in the Order Due Date Sell Sheet to be taken back to the Recap Page Street Date CD- NON 521074 ALLEN, TONY Secret Agent $18.98 4/13/10 3/24/10 CD- RAA 523695 BECK, JEFF Emotion & Commotion $18.98 4/13/10 3/24/10 CD- ATL 521144 CASTRO, JASON Jason Castro $9.94 4/13/10 3/24/10 DV- WRN 523924 CUMMINS, DAN Crazy With A Capital F (DVD) $16.95 4/13/10 3/17/10 CD- ASW 523890 GUCCI MANE Burrrprint (2) HD $13.99 4/13/10 3/24/10 CD- LAT 524047 MAGO DE OZ Gaia III - Atlantia $20.98 4/13/10 3/24/10 CD- MERCHANT, NON 522304 NATALIE Leave Your Sleep (2CD) $24.98 4/13/10 3/24/10 CD- MERCHANT, Selections From The Album NON 522301 NATALIE Leave Your Sleep $18.98 4/13/10 3/24/10 CD- LAT 524161 MIJARES Vivir Asi - Vol. II $16.98 4/13/10 3/24/10 CD- STRAIGHT NO ATL 523536 CHASER With A Twist $18.98 4/13/10 3/24/10 4/13/10 Late Additions Street Date Order Due Date CD- ERP 524163 GLORIANA Gloriana $13.99 4/13/10 3/24/10 CD- MFL 524110 GREAVER, PAUL Guitar Lullabies $11.98 4/13/10 3/24/10 Last Update: 03/03/10 ARTIST: Tony Allen TITLE: Secret Agent Label: NON/Nonesuch Config & Selection #: CD 521074 Street Date: 04/13/10 Order Due Date: 03/24/10 Compact Disc UPC: 075597981001 Box Count: 30 Unit Per Set: 1 SRP: $18.98 Alphabetize Under: T File Under: World For the latest up to date info on this release visit WEA.com. -

Songs by Artist
73K October 2013 Songs by Artist 73K October 2013 Title Title Title +44 2 Chainz & Chris Brown 3 Doors Down When Your Heart Stops Countdown Let Me Go Beating 2 Evisa Live For Today 10 Years Oh La La La Loser Beautiful 2 Live Crew Road I'm On, The Through The Iris Do Wah Diddy Diddy When I'm Gone Wasteland Me So Horny When You're Young 10,000 Maniacs We Want Some P---Y! 3 Doors Down & Bob Seger Because The Night 2 Pac Landing In London Candy Everybody Wants California Love 3 Of A Kind Like The Weather Changes Baby Cakes More Than This Dear Mama 3 Of Hearts These Are The Days How Do You Want It Arizona Rain Trouble Me Thugz Mansion Love Is Enough 100 Proof Aged In Soul Until The End Of Time 30 Seconds To Mars Somebody's Been Sleeping 2 Pac & Eminem Closer To The Edge 10cc One Day At A Time Kill, The Donna 2 Pac & Eric Williams Kings And Queens Dreadlock Holiday Do For Love 311 I'm Mandy 2 Pac & Notorious Big All Mixed Up I'm Not In Love Runnin' Amber Rubber Bullets 2 Pistols & Ray J Beyond The Gray Sky Things We Do For Love, The You Know Me Creatures (For A While) Wall Street Shuffle 2 Pistols & T Pain & Tay Dizm Don't Tread On Me We Do For Love She Got It Down 112 2 Unlimited First Straw Come See Me No Limits Hey You Cupid 20 Fingers I'll Be Here Awhile Dance With Me Short Dick Man Love Song It's Over Now 21 Demands You Wouldn't Believe Only You Give Me A Minute 38 Special Peaches & Cream 21st Century Girls Back Where You Belong Right Here For You 21St Century Girls Caught Up In You U Already Know 3 Colours Red Hold On Loosely 112 & Ludacris Beautiful Day If I'd Been The One Hot & Wet 3 Days Grace Rockin' Into The Night 12 Gauge Home Second Chance Dunkie Butt Just Like You Teacher, Teacher 12 Stones 3 Doors Down Wild Eyed Southern Boys Crash Away From The Sun 3LW Far Away Be Like That I Do (Wanna Get Close To We Are One Behind Those Eyes You) 1910 Fruitgum Co. -

Karaoke Song Book Karaoke Nights Frankfurt’S #1 Karaoke
KARAOKE SONG BOOK KARAOKE NIGHTS FRANKFURT’S #1 KARAOKE SONGS BY TITLE THERE’S NO PARTY LIKE AN WAXY’S PARTY! Want to sing? Simply find a song and give it to our DJ or host! If the song isn’t in the book, just ask we may have it! We do get busy, so we may only be able to take 1 song! Sing, dance and be merry, but please take care of your belongings! Are you celebrating something? Let us know! Enjoying the party? Fancy trying out hosting or KJ (karaoke jockey)? Then speak to a member of our karaoke team. Most importantly grab a drink, be yourself and have fun! Contact [email protected] for any other information... YYOUOU AARERE THETHE GINGIN TOTO MY MY TONICTONIC A I L C S E P - S F - I S S H B I & R C - H S I P D S A - L B IRISH PUB A U - S R G E R S o'reilly's Englische Titel / English Songs 10CC 30H!3 & Ke$ha A Perfect Circle Donna Blah Blah Blah A Stranger Dreadlock Holiday My First Kiss Pet I'm Mandy 311 The Noose I'm Not In Love Beyond The Gray Sky A Tribe Called Quest Rubber Bullets 3Oh!3 & Katy Perry Can I Kick It Things We Do For Love Starstrukk A1 Wall Street Shuffle 3OH!3 & Ke$ha Caught In Middle 1910 Fruitgum Factory My First Kiss Caught In The Middle Simon Says 3T Everytime 1975 Anything Like A Rose Girls 4 Non Blondes Make It Good Robbers What's Up No More Sex.... -

Karaoke with a Message – September 29, 2018 a Project of Angel Nevarez & Valerie Tevere at Interference Archive (314 7Th St
Another Protest Song: karaoke with a message – September 29, 2018 a project of Angel Nevarez & Valerie Tevere at Interference Archive (314 7th St. Brooklyn, NY 11215) karaoke provided by All American Karaoke, songbook edited by Angel Nevarez & Valerie Tevere ( ) 18840 (Ghost) Riders In The Sky Johnny Cash 10274 (I Am Not A) Robot Marina & Diamonds 00005 (I Can't Get No) Satisfaction Rolling Stones 17636 (I Hate) Everything About You Three Days Grace 15910 (I Want To) Thank You Freddie Jackson 05545 (I'm Not Your) Steppin' Stone Monkees 06305 (It's) A Beautiful Mornin' Rascals 19116 (Just Like) Starting Over John Lennon 15128 (Keep Feeling) Fascination Human League 04132 (Reach Up For The) Sunrise Duran Duran 05241 (Sittin' On) The Dock Of The Bay Otis Redding 17305 (Taking My) Life Away Default 15437 (Who Says) You Can't Have It All Alan Jackson # 07630 18 'til I Die Bryan Adams 20759 1994 Jason Aldean 03370 1999 Prince 07147 2 Legit 2 Quit MC Hammer 18961 21 Guns Green Day 004-m 21st Century Digital Boy Bad Religion 08057 21 Questions 50 Cent & Nate Dogg 00714 24 Hours At A Time Marshall Tucker Band 01379 25 Or 6 To 4 Chicago 14375 3 Strange Days School Of Fish 08711 4 Minutes Madonna 08867 4 Minutes Madonna & Justin Timberlake 09981 4 Minutes Avant 18883 5 Miles To Empty Brownstone 13317 500 Miles Peter Paul & Mary 00082 59th Street Bridge Song Simon & Garfunkel 00384 9 To 5 Dolly Parton 08937 99 Luftballons Nena 03637 99 Problems Jay-Z 03855 99 Red Balloons Nena 22405 1-800-273-8255 Logic/Alessia Cara/Khalid A 614 A Beautiful Life Ace -

Rock Rally by Luke Klink Endust and Released Their Self-Titled Metal
Northwoods Escape 2013 - 13 Summer really rocks at Northwoods Rock Rally By Luke Klink endust and released their self-titled metal. Then, all of a sudden, we If you wanna rock this summer, debut album on April 15, 1997. were playing alternative metal. We there is no better place than the Since formation, Sevendust has re- are some kind of heavy and some Northwoods Rock Rally in Rusk leased eight studio albums, earned kind of rock and some kind of met- County. The out additional charting success and gold al.” Rock Rally runs Thursday through sales certiications. The bands gold Trapt is an American rock band Saturday, Aug. 15-17, south of Glen albums are Sevendust, released in that formed in Los Gatos, Calif., in Flora on County B. 1997, Home, released in 1999, and August 1997. The group consists The top-billed Animosity, re- of lead singer Chris Taylor Brown, bands include Sev- leased in 2001. lead guitarist Travis Miguel, drum- endust, Trapt, 3 Pill Sevendust Their top- mer Dylan Thomas Howard and Morning and Royal Trapt charting tracks bass guitarist Peter Charell. Bliss. They will be are “Enemy” (10), The band can be described as joined by at least 10 3 Pill Morning “Ugly,” (12), modern, aggressive hard rock. The more hard rocking “Driven” (10), band expanded its sound to include acts. Party or stay Royal Bliss “Angel’s Son” synthesizers and samples. home, organizers More than 10 bands (11), “Praise” Two of the band’s six studio al- say. (15) and “Denial” bums have peaked higher than 20 on The annual hard- (14). -

February 4Th-February 7Th Weekly Newsletter
Trevor’s Weekly News Letter Rodgers, Trevor – Author/Editor February 4th- February 7th Tuesday, February 4th Instructor one- students are continuing their studies in classroom one today the leader is gong over the Introduction, Learning Formally and InFormally instructing curiosity and adapting learning skills. This class will be here all week and since it is a Tuesday we have the regular weekly Board oF Directors meeting usually taking place in classroom Four. NIPSTA Fire Academy- students are in the hangar the class oF 2001 they are practicing training with the Ventilation using their tools to carve out and play open the pieces oF wood on top oF the prop. As a reminder For those unaware 2020 is a leap year so there will be an extra day this month, February 29th instead oF stopping on the 28th whether that’s a good thing I guess we’ll find out could be a sign for a longer winter than usual or an early spring. The groundhog didn’t see it’s shadow on Sunday which signiFies an early spring, however the Furry creature has only been correct with it’s predictions about 40 percent of the time so take it with a grain of salt we can only hope. Wednesday, February 5th Aerovisa- students are in classroom Four with the instructor going over Is The Weather Good Enough to Fly the drones? Talking about an in depth discussion measuring the weather patterns in the clouds to determine if it saFe to Fly them in the air. Only class going on this aFternoon I believe the others took place in the morning or beFore I arrived. -
Augsome Karaoke Song List Page 1
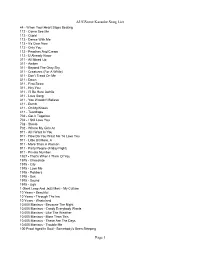
AUGSome Karaoke Song List 44 - When Your Heart Stops Beating 112 - Come See Me 112 - Cupid 112 - Dance With Me 112 - It's Over Now 112 - Only You 112 - Peaches And Cream 112 - U Already Know 311 - All Mixed Up 311 - Amber 311 - Beyond The Gray Sky 311 - Creatures (For A While) 311 - Don't Tread On Me 311 - Down 311 - First Straw 311 - Hey You 311 - I'll Be Here Awhile 311 - Love Song 311 - You Wouldn't Believe 411 - Dumb 411 - On My Knees 411 - Teardrops 702 - Get It Together 702 - I Still Love You 702 - Steelo 702 - Where My Girls At 911 - All I Want Is You 911 - How Do You Want Me To Love You 911 - Little Bit More, A 911 - More Than A Woman 911 - Party People (Friday Night) 911 - Private Number 1927 - That's When I Think Of You 1975 - Chocolate 1975 - City 1975 - Love Me 1975 - Robbers 1975 - Sex 1975 - Sound 1975 - Ugh 1 Giant Leap And Jazz Maxi - My Culture 10 Years - Beautiful 10 Years - Through The Iris 10 Years - Wasteland 10,000 Maniacs - Because The Night 10,000 Maniacs - Candy Everybody Wants 10,000 Maniacs - Like The Weather 10,000 Maniacs - More Than This 10,000 Maniacs - These Are The Days 10,000 Maniacs - Trouble Me 100 Proof Aged In Soul - Somebody's Been Sleeping Page 1 AUGSome Karaoke Song List 101 Dalmations - Cruella de Vil 10Cc - Donna 10Cc - Dreadlock Holiday 10Cc - I'm Mandy 10Cc - I'm Not In Love 10Cc - Rubber Bullets 10Cc - Things We Do For Love, The 10Cc - Wall Street Shuffle 112 And Ludacris - Hot And Wet 12 Gauge - Dunkie Butt 12 Stones - Crash 12 Stones - We Are One 1910 Fruitgum Co. -

Chanticleer | Vol 55, Issue 22
Jacksonville State University JSU Digital Commons Chanticleer Historical Newspapers 2007-03-08 Chanticleer | Vol 55, Issue 22 Jacksonville State University Follow this and additional works at: https://digitalcommons.jsu.edu/lib_ac_chanty Recommended Citation Jacksonville State University, "Chanticleer | Vol 55, Issue 22" (2007). Chanticleer. 1471. https://digitalcommons.jsu.edu/lib_ac_chanty/1471 This Book is brought to you for free and open access by the Historical Newspapers at JSU Digital Commons. It has been accepted for inclusion in Chanticleer by an authorized administrator of JSU Digital Commons. For more information, please contact [email protected]. myspace.com. I a place for friends This could get you into so much trouble. -Seestory, page 3. arch 8,2007 Jacksonvllle State University Volume 55, Issue 22 I-. f Student Access System. the local paper link to the "local news." 1'The "library" tab introduces nine box- MyJSU also acts as a pin reliever. Parents no long<: es at the helm of the MyJSU user. From have to use swear words over tlie phone to find a student'& 6in the rafters of the Jacksonville State Universiv cntcring the ccltalog, checklng out books financiat aid information Provided under the "registrai- Hall of Fame hang prominent jerseys that have solidified or simply scrolling through the data- tion" link in,the "hom'e" tab, students are able to find. thi campus as a hghly prestigious academic institution. bases, the nine "library" tabs represent out which financial aid letters have been submitted and :, N es such as Dr. Theron Montgomery and events such h Houston Cole Library in a nutshell. -

Pacad286-All Access#7
Sevendus t’s Clint Lowery: ATLAnTA -bASeD AGGro -roCKerS SeVenDuST hAVe JuST reLeASeD An lounge. he’s based out of north Carolina where he has a studio. unplugged album. but don’t get the idea they’ve mellowed out. he’s my idol.” These Yamahas “we put on what has to be the heaviest acoustic show ever,” Yet Clint’s first instrument was drums — because, he explains, claims Clint Lowery, who shares guitar duties in Sevendust with he wanted to play with his dad. but the younger Lowery eventually are just incredible John Connolly. “The comment we get from a lot of fans is, ‘That’s switched over to guitar, studying with north Carolina instructor the most aggressive acoustic concert I’ve ever seen!’ we’re not robbie Greene and eventually fulfilling his wish of playing with his John Denver-ing it up there — we’re strumming real hard.” father. “we’d play old songs like ‘A whiter Shade of Pale’ and otis guitars. The second According to Lowery, Sevendust fans weren’t the only people redding stuff,” recalls Clint. “It was great to learn the chord pro - who needed convincing that the acoustic album was a good idea. gressions for all those old songs.” I picked them up, “our label wasn’t all that interested at first. we were cautious too Clint eventually made his way to Atlanta, where the members because we didn’t want it to seem like we were trying to market of Sevendust starting jamming in 1995. but the band was not ourselves as some sort of more commercial acoustic band.