Maternal Mortality in Orissa: an Epidemiological Study My
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
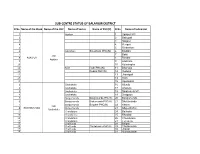
Sub-Centre Status of Balangir District
SUB-CENTRE STATUS OF BALANGIR DISTRICT Sl No. Name of the Block Name of the CHC Name of Sector Name of PHC(N) Sl No. Name of Subcenter 1 Agalpur 1 Agalpur MC 2 2 Babupali 3 3 Nagaon 4 4 Rengali 5 5 Rinbachan 6 Salebhata Salebhata PHC(N) 6 Badtika 7 7 Bakti CHC 8 AGALPUR 8 Bendra Agalpur 9 9 Salebhata 10 10 Kutasingha 11 Roth Roth PHC(N) 11 Bharsuja 12 Dudka PHC(N) 12 Duduka 13 13 Jharnipali 14 14 Roth 15 15 Uparbahal 1 Sindhekela 16 Alanda 2 Sindhekela 17 Arsatula 3 Sindhekela 18 Sindhekela MC 4 Sindhekela 19 Dedgaon 5 Bangomunda Bangomunda PHC(N) 20 Bangomunda 6 Bangomunda Bhalumunda PHC(N) 21 Bhalumunda 7 Bangomunda Belpara PHC(N) 22 Khaira CHC 8 BANGOMUNDA Bangomunda 23 Khujenbahal Sindhekela 9 Chandotora 24 Batharla 10 Chandotora 25 Bhuslad 11 Chandotora 26 Chandutara 12 Chandotora 27 Tureikela 13 Chulifunka 28 Biripali 14 Chulifunka Chuliphunka PHC(N) 29 Chuliphunka 15 Chulifunka 30 Jharial 16 Chulifunka 31 Munda padar 1 Gambhari 32 Bagdor 2 Gambhari 33 Ghagurli 3 Gambhari Gambhari OH 34 Ghambhari 4 Gambhari 35 Kandhenjhula 5 Belpada 36 Belpara MC 6 Belpada 37 Dunguripali 7 Belpada 38 Kapani 8 Belpada 39 Nunhad 9 Mandal 40 Khairmal CHC 10 BELPARA Mandal Khalipathar PHC(N) 41 Khalipatar Belpara 11 Mandal 42 Madhyapur 12 Mandal Mandal PHC(N) 43 Mandal 13 Mandal 44 Dhumabhata 14 Mandal Sulekela PHC(N) 45 Sulekela 15 Salandi 46 Bahabal 16 Salandi 47 Banmal 17 Salandi 48 Salandi 18 Salandi 49 Sarmuhan 19 Salandi 50 Kanut 1 Chudapali 51 Barapudugia 2 Chudapali Bhundimuhan PHC(N) 52 Bhundimuhan 3 Chudapali 53 Chudapali MC 4 Chudapali 54 -

Y Report (Dsr) of Balangir District, Odisha
Page | 1 DISTRICT SURVEY REPORT (DSR) OF BALANGIR DISTRICT, ODISHA. FOR ROAD METAL/BUILDING STONE/BLACK STONE (FOR PLANNING & EXPLOITATION OF MINOR MINERAL RESOURCES) ODISHA BALANGIR As per Notification No. S.O. 3611(E) New Delhi dated 25th July 2018 of Ministry of Environment, Forest & Climate Change (MoEF & CC) COLLECTORATE BALANGIR Page | 2 CONTENT CH. DESCRIPTION PAGE NO. NO. Preamble 4-5 1 Introduction 1.1 Location and Geographical Area 6-9 1.2 Administrative Units 9-10 1.3 Connectivity 10-13 2 Overview of Mining Activity in the District 13 3 General Profile of the District 3.1 Demography 14 4 Geology of the District 4.1 Physiography & Geomorphology 15-22 4.2 Soil 22-23 4.3 Mineral Resources. 23-24 5 Drainage of Irrigation Pattern 5.1 River System 25 6 Land Utilization Pattern in the District 6.1 Forest and non forest land. 26-27 6.2 Agricultural land. 27 6.3 Horticultural land. 27 7 Surface Water and Ground Water Scenario of the District 7.1 Hydrogeology. 28 7.2 Depth to water level. 28-30 7.3 Ground Water Quality. 30 7.4 Ground Water Development. 31 7.5 Ground water related issues & problems. 31 7.6 Mass Awareness Campaign on Water Management 31 Training Programme by CGWB 7.7 Area Notified By CGWB/SGWA 31 7.8 Recommendations 32 8 Rainfall of the District and Climate Condition 8.1 Month Wise rainfall. 32-33 8.2 Climate. 33-34 9 Details of Mining Lease in the District 9.1 List of Mines in operation in the District 34 Page | 4 PREAMBLE Balangir is a city and municipality, the headquarters of Balangir district in the state of Odisha, India. -

Officename a G S.O Bhubaneswar Secretariate S.O Kharavela Nagar S.O Orissa Assembly S.O Bhubaneswar G.P.O. Old Town S.O (Khorda
pincode officename districtname statename 751001 A G S.O Khorda ODISHA 751001 Bhubaneswar Secretariate S.O Khorda ODISHA 751001 Kharavela Nagar S.O Khorda ODISHA 751001 Orissa Assembly S.O Khorda ODISHA 751001 Bhubaneswar G.P.O. Khorda ODISHA 751002 Old Town S.O (Khorda) Khorda ODISHA 751002 Harachandi Sahi S.O Khorda ODISHA 751002 Kedargouri S.O Khorda ODISHA 751002 Santarapur S.O Khorda ODISHA 751002 Bhimatangi ND S.O Khorda ODISHA 751002 Gopinathpur B.O Khorda ODISHA 751002 Itipur B.O Khorda ODISHA 751002 Kalyanpur Sasan B.O Khorda ODISHA 751002 Kausalyaganga B.O Khorda ODISHA 751002 Kuha B.O Khorda ODISHA 751002 Sisupalgarh B.O Khorda ODISHA 751002 Sundarpada B.O Khorda ODISHA 751002 Bankual B.O Khorda ODISHA 751003 Baramunda Colony S.O Khorda ODISHA 751003 Suryanagar S.O (Khorda) Khorda ODISHA 751004 Utkal University S.O Khorda ODISHA 751005 Sainik School S.O (Khorda) Khorda ODISHA 751006 Budheswari Colony S.O Khorda ODISHA 751006 Kalpana Square S.O Khorda ODISHA 751006 Laxmisagar S.O (Khorda) Khorda ODISHA 751006 Jharapada B.O Khorda ODISHA 751006 Station Bazar B.O Khorda ODISHA 751007 Saheed Nagar S.O Khorda ODISHA 751007 Satyanagar S.O (Khorda) Khorda ODISHA 751007 V S S Nagar S.O Khorda ODISHA 751008 Rajbhawan S.O (Khorda) Khorda ODISHA 751009 Bapujee Nagar S.O Khorda ODISHA 751009 Bhubaneswar R S S.O Khorda ODISHA 751009 Ashok Nagar S.O (Khorda) Khorda ODISHA 751009 Udyan Marg S.O Khorda ODISHA 751010 Rasulgarh S.O Khorda ODISHA 751011 C R P Lines S.O Khorda ODISHA 751012 Nayapalli S.O Khorda ODISHA 751013 Regional Research Laboratory -

Centre to SC
www Vol - 17 www Issue-301 www Bhubaneswar www 15 June, 2021 www Tuesday ww Orissa Today email:[email protected], www Rs.2.00 People’s Voice [email protected] www Pages -8 RNI NO - ODIENG/2005/16409 For e paper : www.orissatodaynews. in [email protected] PM greets people Bengal post-poll violence of Odisha on MHA notification not related Raja Parba Rape survivors seek To CAA: Centre to SC SC intervention New Delhi, Jun 14 (UNI) sisted that an FIR was New Delhi, Jun 14 (UNI) ation to the foreigners and tors of Morbi, Rajkot, Two rape survivors includ- filed. The 17-year-old The Centre has informed applies only to a foreigner Patan and Vadodara in ing a minor girl and a 60- girl's plea contended that the Supreme Court that the who has entered the coun- Gujarat, Jalore, Udaipur, year-old woman have ap- she was gang-raped on New Delhi, Jun 14 (UNI) May 28 order of the Min- try legally as the Central Pali, Barmer, and Sirohi proached the Supreme May 9 by the supporters Prime Minister Narendra istry of Home Affairs Government used its au- in Rajasthan, Durg, and Court seeking a Special of Trinamool Congress Modi on Monday greeted (MHA) which empowered thority under Section 16 of Balodabazar in Investigation Team (SIT) and sought an SIT probe the people of Odisha on certain districts to grant the Citizenship Act and Chhattisgarh, Faridabad probe into the gang-rape into the incident and also the occasion of Raja citizenship to non-Muslim delegated its powers to in Haryana and incidents and violence sought a transfer of case Parba. -

Town and Village Directory, Bolangir, Part-A, Series-16, Orissa
CENSUS OF INDIA, 1971 SERIES 16 ORISSA PART X DISTRICT CENSUS HANDBOO~ PART A-TOWN AND VILLAGE DIRECTORY BOLANGIR B. TRIPATHI of- the Indian Administrative Service Director Df Census Operations, Orissa CENSUS OF INDIA, 1971 DISTRICT CENSUS HA-NDBOOK PART A-TOWN AND VILLAGE DIRECTORY BOLA_NGIR PREFACE The District Census Handbook first introduced.as an ancillary to 1951 Census appeared as a State. Government publication in a more elaborate and ambitious form in 1961 Census. It was divided into 3 parts: Part] gave a narrative account of each District; Part 1I contained various Census Tables and a ~eries of Primary Census data relating to each village and town ; and Part III presented certain administrative statistics obtained from Government Departments. These parts further enriched by inclusion of maps of the district and of police stations within the district were together -brought out in ODe volume. The Handbook, for each one of the 13 Districts of the State was acknowledged to be highly useful. 2. But the purpose and utility of this valuable compilation somewhat suffered on account of the time lag that intervened between the conclusion of Census and the publication of the Handbook. The delay was unavoidable in the sense that the Handbook-complete with all the constituent parts brought together in one volume had necessarily<to wait till after completion of the processing and tabulation of Gensus data and collection and compilation of a large array of administrative and other statistics. 3. With the object of cutting out the delay, and also_ to making each volume handy and not-too-bulky it has been decided to bring out the 1971 District Census Handbook in three parts separately with the data becoming available from stage to stage as briefly indicated below : Part A-This part will incorporate the Town Directory and the Village Directory for each district. -

List of PHC {N) SI. No District C.H.C Si. No .P.H.C {NJ Angul BANAMIRA > Angul 2 PURUNAGARH :.- Angul Banta La PURUNA !(OTE
- List of PHC {N) - 0 SI. No District C.H.C s- I. No .P.H.C {NJ Angul 1 BANAMIRA > -- Angul 2 PURUNAGARH :.-_ -- Angul Banta la 3 PURUNA_!(OTE Angul 4 - JAGANNATHPUR ,- Angul 5 TAINSI MHU -- Angul 6- PAIKSAHI / Madhapu Angul 7 {THAKURGARH le r Angul 8 PATAKA. C Angul I® - - 9 BADAKE RAJANGA A»g , Angul 10 . BALARAMPRASAD Banarpal_ Angul 11 MARATIRAHAT / - Angul 12 , TALAMUL - - Angul 13 BAGEDIA Angul 14 Kosala JARAPADA Angul 15 BALIPATA 1 ·- Angul 16 Patrapada - Angul 17 BAJRAKOTE. Angul 18 BIROO -· Kaniha a Angul .. 19 PABITRANAGAR Angul 20 Kuluma (Angul 21 CHASA GURUJANGA Angul 22 JAMARDIHI 7 Angul Khamar 23 JHARBEDA / Angul 24 RAJADANGA Angul 25 SAHAR GURUJUNGA ,,,,--_ Angul 26 Raj ANGAPADA Angul 27 HANDAPA K.Nagar Angul 28 BOINDA. - Angul 29 Godiban KALLAM CHHULN · » Angul 30 GOPAL PRASAD - dha Angul 31 KANKILL - Balasore 32 Ghantua Balasore 33 LANGALES WAR Balasore Baliapal 34 SRIRAMPUR -- Balasore 35 JAMAKUNDA A Balasore 36 Bolanga g Balasore 37 AMARDA ROAD Balasore 38 IRDA.· so , Balasore Basta 39 PAUNSAKALI Balasore 40 SANTOSH UR Balasore 41 SINGLA Balasore 42 BHOGORAI Balasore 43 CHANDANESWAR Balasore 44 DAHAMUNDA · Joo Balasore g Iola¢urn 45 DEULA 0 JQI>VVa Balasore 46 Pur JALASUHARIA , Balasore 47 KAKHADA Balasore 48 NIMATPUR Balasore 49 Jayarampur Balasore .. so 1SRADHAP UR , Balasore 51 GARASANGA - Balasore 52 ANTARA· - J Balasore 53 / Khaira DUNGURA Balasore / I 54 GANDIBED Balasore 55 K UPARI - Balasore 56 TUDIGADIA Balasore 57 KESHARIPUR Balasore 58 BAGUDI - a, - Bala sore Soro 59 DANDAPALASA - Balasore , 60 MANIPUR ,, - Balasore 61 - PAKHAR - Balasore All 62 BAHANAGA· a Balasore Gopal 63 BISHNUPUR Jo Balasore Pur 64 KHARASAHAPUR ®e Balasore 65 SAUD Balasore 66 BASANTI SINDHIA 2 Balasore 67 PALASAPUR . -

Information( 13 Tahasil & 80 R.I. Offices)
Information( 13 Tahasil & 80 R.I. Offices) CHAMPUA TAHASIL Champua Tahasil started functioning w.e.f. 01.04.1963. The total area of this Tahasil is Ac. 84,754.274. (342.98 SQ. KMS.) This Tahasil is coming under the jurisdiction of Champua Sub- Division and the area of this Tahasil is co-terminus with the area of Champua Block and Champua NAc consisting six R.I. circles namely Champua, Jyotipur, Chimila, Remuuli, Karanjia and Bhanda. This Tahasil is constituted with 151 revenue villages under 23 G.Ps. and newly created Champua NAC which coveres three police stations namely Champua, Joda (part) and Baria(part) . The total population of the Tahasil is 1, 15,103 as per 2011 census. Communication facilities are available from Tahasil head quarter to District head quarter. The principal income source of the people is cultivation and business. Champua Tahasil is situated 50 Kms away from District Headquarters. This Tahasil is surrounded by Maurbhanj District in east, Barbil Tahsil in west, Singhbhum District of Jharkhand State in north and Jhumpura Tahasil in south. Brief notes on R.I. Circles Under Champua Tahasil Champua : This R.I. circle is consisting of 17 revenue villages covering Rajia G.P. and newly declared Champua NAC having area of Ac.11,967.650. All the 17 villages are coming under jurisdiction of Champua P.S. and co-terminus with the area of Rajia G.P. and Champua NAC. Chimila : This R.I. circle is consisting of 27 villages covering Kodagadia, Jamudalak, Sunaposi and Kutariposi G.Ps. having area of Ac.14,484.513. -

40423-053: Due Diligence of Ongoing Projects in Assam, Chhattisgarh
Due Diligence Report on Social Safeguards April 2015 IND: Rural Connectivity Investment Program – Project 3 Due Diligence of Ongoing Projects in Assam, Chhattisgarh, Madhya Pradesh, Odisha, and West Bengal under Project 1 and Project 2 (Loan 2881-IND) and (Ln 3065-IND) Prepared by Ministry of Rural Development, Government of India for the Asian Development Bank. CURRENCY EQUIVALENTS (as of 31 March 2015) Currency unit – Indian rupees (INR/Rs) Rs1.00 = $ 0.016 $1.00 = Rs 62.5096 ACRONYMS AND ABBREVIATIONS ADB : Asian Development Bank APs : Affected Persons BPL : Below Poverty Line CD : Cross Drainage DM : District Magistrate EA : Executing Agency EAF : Environment Assessment Framework ECOP : Environmental Codes of Practice FFA : Framework Financing Agreement GOI : Government of India GRC : Grievances Redressal Committee IA : Implementing Agency IEE : Initial Environmental Examination MFF : Multi-Project Financing Facility MORD : Ministry of Rural Development MOU : Memorandum of Understanding NC : Not Connected NGO : Non-Government Organization NRRDA : National Rural Road Development Agency NREGP : National Rural Employment Guarantee Program PIU : Project Implementation Unit PIC : Project Implementation Consultants PFR : Periodic Finance Request PMGSY : Pradhan Mantri Gram Sadak Yojana RCIP : Rural Connectivity Investment Programme ROW : Right-of-Way RRP : Report and Recommendation of the President RRSIP II : Rural Roads Sector II Investment Program SRRDA : State Rural Road Development Agency ST : Scheduled Tribes TA : Technical Assistance TOR : Terms of Reference TSC : Technical Support Consultants UG : Upgradation WHH : Women Headed Households GLOSSARY Affected Persons (APs): Affected persons are people (households) who stand to lose, as a consequence of a project, all or part of their physical and non-physical assets, irrespective of legal or ownership titles. -

Village and Town Directory, Kendujhar, Part-A, Series-19, Orissa
CENSUS OF INDIA, 1991 SERIES -19 ORISSA PART - XII DISTRICT CENSUS HANDBOOK PART A -VILLAGE.. AND TOWN DIRECTORY KENDUJHAR R.N. SENAPATI OFTHE INDIAN ADMINISTRATIVE SERVICE Director of Census Operations, Orissa CENSUS OF INDIA, 1991 DISTRICT CENSUS HANDBOOK PART A - VILLAGE AND TOWN DIRECTORY KENDUJHAR FOREWORD Publication of the District Census Handbocks (DCHs )was initiated after the 1951 Census and is continuing since then with some innovations/modifications after each decennial Census. This is the most valuable district level publication brought out by the Census Organisation on behalf of each State Govt./Union Territory administration. It inter-alia provides data/information on some of the basic demographic and socia-economic characteristics and on the availability of certain important civic amenities/facilities in each village and town of the respective districts. This publication has thus proved to be of immense utility to the planners, administrators, academicians and researchers. The scope of the DCH was initially confined to certain important census tables on population, economic and socia-cultural aspects as also the Primary Census Abstract (PCA) of each village and town (ward-wise) of the district. The DCHs published after the 1961 Census contained a descriptive account of the district administrative statistics, census tables and Village and Town Directories including PCA. After the1971 Census,two parts of the District Census Handbooks (Part-A comprising Village and Town Directories and Part -B comprising Village and Town PCA) were released in all the States and Union Territories. The third Part (Part-C) of the District Census Handbooks comprising administrative statistics and district census tables, which was also to be brought out, could not be published in many States/UTs due to considerable delay in compilation of relevant material. -
Environmental Monitoring Report
Environmental Monitoring Report Semiannual Monitoring Report April – September 2017 July 2018 IND: Railway Sector Investment Program Prepared by Ministry of Railways for the Government of India and the Asian Development Bank. This environmental monitoring report is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or staff, and may be preliminary in nature. In preparing any country program or strategy, financing any project, or by making any designation of or reference to a particular territory or geographic area in this document, the Asian Development Bank does not intend to make any judgments as to the legal or other status of any territory or area. Indian Government Ministry of Railways Asian Development Bank Multitranche Financing Facility No. 0060-IND Loan No. 2793-IND, 3108-IND Railway Sector Investment Program Track Doubling and Electrification on Critical Routes Environmental Monitoring Report Semi Annual Report: April 2017 – September 2017 Egis Rail – Egis India Environmental Safeguards Monitoring Report No. 9 September 2017 Contents Executive Summary ................................................................................................................................. 2 1. Background ..................................................................................................................................... 3 1.1 Railway Sector Investment Programme and Multi Tranche Financing Facility ...................... 3 1.2 Active contracts -

KEONJHARGARH BLOCK. the Name of the Block Is Keonjhargarh Block
KEONJHARGARH BLOCK. The name of the Block is Keonjhargarh Block. It started functioning in the year 1955. The geographical area of this Block is 297 Sqr. Miles. The population as per 2011 census of this Block is 162148 out of which Male Population is 81305, Female Population is 80843, ST Population is 81567SC Population is 16082 and Others are 64499 no. The literate population of this Block is 94723. Category wise the population percentage of this Block is as follows, Male:- 50.14, Female :- 49.86, ST :- 50.3, SC : 09.9, Oth :- 39.8 and literate population percentage is 58.4. The total Households of this Block is 35963 no. This Block consists of 24 no. of GPs in which there are 231 Revenue villages and 09 hamlets. The Block has 01 no. of CHC , 05 no. of New PHC, 02 no. of Govt. Homeopathy Dispensary, 30 no. of ANM centers, 190 Asha centers, 261 no. of AW centers, 198 no. of GKS for facilitation of better health care of the villagers. For education regards the Block has 141 no. of PS, 25 no. of PUPS, 11 no. of NUPS, 21 no. of UPS, 17 no. of UGMES, 38 no. of High Schools, 03 no. of Degree Colleges and 02 no. of Degree Engineering Colleges. The Block provides drinking water to the inhabitants through 1584 no. of Tube Wells, 47 Wells and 25 no. of Piped Water System. To irrigate its agricultural fields the Block has 03 MIPs. 36 no. of Financial Institutions and 02 no. of LAMPS are functioning in the Block and they are financing the villagers in respect of ISB, Agriculture, Pisciculture and all sort of segments including credit linkage to SHG groups. -

ODISHA:CUTTACK NOTIFICATION No
OFFICE OF THE BOARD OF SECONDARY EDUCATION :ODISHA:CUTTACK NOTIFICATION No:-458(syllabus)/ Date19.07.2017 In pursuance of the Notification No-19724/SME, Dated-28.09.2016 of the Govt. of Odisha, School & Mass Education Deptt. & Letter No-1038/Plg, Dated-19.06.2017 of the State Project Director, OMSM/RMSA, the Vocational Education Course under RMSA at Secondary School Level in Trades i.e. 1.IT & ITES, 2.Travel & Tourism & 3.Retail will continue as such in Class-IX for the Academic session-2017-18 and 4.BFS (In place of B.F.S.I) , 5.Beauty & Wellness and 6. Health Care will be introduced newly in Class-IX(Level- I ) for the Academic Session- 2017-18 as compulsory subject in the following 208(old) & 106(new) selected Schools (Subject mentioned against each).The above subjects shall be the alternative of the existing 3rd language subjects . The students may Opt. either one of the Third Languages or Vocational subject as per their choice. The period of distribution shall be as that of Third Language Subjects i.e. 04 period per week so as to complete 200 hours of course of Level-I . The course curriculum shall be at par with the curriculum offered by PSSCIVE, Bhopal . List of 314 schools (208 + 106) approved under Vocational Education (2017-18) under RMSA . 208 (Old Schools) Sl. Name of the Approval Name of Schools UDISE Code Trade 1 Trade 2 No. District Phase PANCHAGARH BIJAY K. HS, 1 ANGUL 21150303103 Phase II IT/ITeS Travel & Tourism BANARPAL 2 ANGUL CHHENDIPADA High School 21150405104 Phase II IT/ITeS Travel & Tourism 3 ANGUL KISHORENAGAR High School 21150606501 Phase II IT/ITeS Travel & Tourism MAHENDRA High School, 4 ANGUL 21151001201 Phase II IT/ITeS Travel & Tourism ATHAMALLIK 5 ANGUL MAHATAB High School 21150718201 Phase II IT/ITeS Travel & Tourism 6 ANGUL PABITRA MOHAN High School 21150516502 Phase II IT/ITeS Travel & Tourism 7 ANGUL JUBARAJ High School 21151101303 Phase II IT/ITeS Travel & Tourism 8 ANGUL Anugul High School 21150902201 Phase I IT/ITeS 9 BALANGIR GOVT.