Proton Pump Inhibitors (Ppis) for Four Weeks
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

List of New Drugs Approved in India from 1991 to 2000
LIST OF NEW DRUGS APPROVED IN INDIA FROM 1991 TO 2000 S. No Name of Drug Pharmacological action/ Date of Indication Approval 1 Ciprofloxacin 0.3% w/v Eye Indicated in the treatment of February-1991 Drops/Eye Ointment/Ear Drop external ocular infection of the eye. 2 Diclofenac Sodium 1gm Gel March-1991 3 i)Cefaclor Monohydrate Antibiotic- In respiratory April-1991 250mg/500mg Capsule. infections, ENT infection, UT ii)Cefaclor Monohydrate infections, Skin and skin 125mg/5ml & 250mg/5ml structure infections. Suspension. iii)Cefaclor Monohydrate 100mg/ml Drops. iv)Cefaclor 187mg/5ml Suspension (For paediatric use). 4 Sheep Pox Vaccine (For April-1991 Veterinary) 5 Omeprazole 10mg/20mg Short term treatment of April-1991 Enteric Coated Granules duodenal ulcer, gastric ulcer, Capsule reflux oesophagitis, management of Zollinger- Ellison syndrome. 6 i)Nefopam Hydrochloride Non narcotic analgesic- Acute April-1991 30mg Tablet. and chronic pain, including ii)Nefopam Hydrochloride post-operative pain, dental 20mg/ml Injection. pain, musculo-skeletal pain, acute traumatic pain and cancer pain. 7 Buparvaquone 5% w/v Indicated in the treatment of April-1991 Solution for Injection (For bovine theileriosis. Veterinary) 8 i)Kitotifen Fumerate 1mg Anti asthmatic drug- Indicated May-1991 Tablet in prophylactic treatment of ii)Kitotifen Fumerate Syrup bronchial asthma, symptomatic iii)Ketotifen Fumerate Nasal improvement of allergic Drops conditions including rhinitis and conjunctivitis. 9 i)Pefloxacin Mesylate Antibacterial- In the treatment May-1991 Dihydrate 400mg Film Coated of severe infection in adults Tablet caused by sensitive ii)Pefloxacin Mesylate microorganism (gram -ve Dihydrate 400mg/5ml Injection pathogens and staphylococci). iii)Pefloxacin Mesylate Dihydrate 400mg I.V Bottles of 100ml/200ml 10 Ofloxacin 100mg/50ml & Indicated in RTI, UTI, May-1991 200mg/100ml vial Infusion gynaecological infection, skin/soft lesion infection. -

Heartburn/Indigestion Heartburn Or Acid Indigestion During Pregnancy Is a Common Problem, Especially As the Baby Grows and Puts Pressure on the Stomach
Pregnant Moms COMMON PROBLEMS Nausea Nausea that occurs during pregnancy, better known as “morning sickness,” can be a problem any time, day or night. The good news is that it usually only lasts a couple of months. If you experience nausea, there are food choices that you can make that might help. Try dry, starchy foods like crackers and dry toast. Eat slowly. Sit or lie still while eating. Spicy, high-fat foods like sausage, other fatty meats, fried foods, and rich pastries are not well tolerated. Drink liquids separate from your meals, and take small sips. Citrus juices can make nausea worse. Once the nausea has passed, there are a few ways to help prevent it from coming back. Below are some tips to help prevent nausea. Eat small frequent meals instead of two or three large meals. Drink liquids between meals, not with your meal. Drink only about ½ cup at a time. Avoid high-fat drinks. 1 Pregnant Moms Avoid strong-smelling foods with offensive odors. Take prenatal vitamins and iron supplements on a full stomach. Heartburn/Indigestion Heartburn or acid indigestion during pregnancy is a common problem, especially as the baby grows and puts pressure on the stomach. Here are some foods you should avoid to help prevent indigestion. • Fatty meats Examples: sausage, bacon, hot dogs • Food from cabbage family Examples: cucumber, greens, broccoli, onions, and cabbage • Fried foods Examples: french fries, fried chicken • Rich pastries Examples: doughnuts, fried pies, cream pies 2 Pregnant Moms Here are more tips on how to avoid heartburn and indigestion during pregnancy. -

Acid Reflux and Oesophagitis Gastro-Oesophageal Reflux Disease (GORD)
Acid reflux and oesophagitis Gastro-oesophageal reflux disease (GORD) Acid reflux is when acid from the stomach leaks up into the gullet (oesophagus). This may cause heartburn and other symptoms. A medicine which prevents your stomach from making acid is a common treatment and usually works well. Some people take short courses of treatment when symptoms flare up. Some people need long term daily treatment to keep symptoms away. Understanding the oesophagus and stomach When we eat, food passes down the oesophagus (gullet) into the stomach. Cells in the lining of the stomach make acid and other chemicals that help to digest food. Stomach cells also make mucus that protects them from damage from the acid. The cells lining the oesophagus are different and have little protection from acid. There is a circular bank of muscle (a ‘sphincter’) at the junction between the oesophagus and stomach. This relaxes to allow food down but then normally tightens up and stops food and acid leaking back up (refluxing) into the oesophagus. In effect the sphincter acts like a valve. What are reflux and oesophagitis? Acid reflux is when some acid leaks up (refluxes) into the oesophagus. Oesophagitis means inflammation of the lining of the oesophagus. Most cases of oesophagatis are due to reflux of stomach acid which irritates the inside lining of the oesophagus. The lining of the oesophagus can cope with a certain amount of acid. However, it is more sensitive to acid in some people. Therefore, some people develop symptoms Source: Endoscopy Reference No: 6556-1 Issue date: 11/9/19 Review date: 11/9/22 Page 1 of 6 with only a small amount of reflux. -

Peptic Ulcer Disease
Peptic Ulcer Disease orking with you as a partner in health care, your gastroenterologist Wat GI Associates will determine the best diagnostic and treatment measures for your unique needs. Albert F. Chiemprabha, M.D. Pierce D. Dotherow, M.D. Reed B. Hogan, M.D. James H. Johnston, III, M.D. Ronald P. Kotfila, M.D. Billy W. Long, M.D. Paul B. Milner, M.D. Michelle A. Petro, M.D. Vonda Reeves-Darby, M.D. Matt Runnels, M.D. James Q. Sones, II, M.D. April Ulmer, M.D., Pediatric GI James A. Underwood, Jr., M.D. Chad Wigington, D.O. Mark E. Wilson, M.D. Cindy Haden Wright, M.D. Keith Brown, M.D., Pathologist Samuel Hensley, M.D., Pathologist Jackson Madison Vicksburg 1421 N. State Street, Ste 203 104 Highland Way 1815 Mission 66 Jackson, MS 39202 Madison, MS 39110 Vicksburg, MS 39180 Telephone 601/355-1234 • Fax 601/352-4882 • 800/880-1231 www.msgastrodocs.com ©2010 GI Associates & Endoscopy Center. All rights reserved. A discovery that Table of contents brought relief to millions of ulcer What Is Peptic Ulcer Disease............... 2 patients...... Three Major Types Of Peptic Ulcer Disease .. 6 The bacterium now implicated as a cause of some ulcers How Are Ulcers Treated................... 9 was not noticed in the stomach until 1981. Before that, it was thought that bacteria couldn’t survive in the stomach because Questions & Answers About Peptic Ulcers .. 11 of the presence of acid. Australian pathologists, Drs. Warren and Marshall found differently when they noticed bacteria Ulcers Can Be Stubborn................... 13 while microscopically inspecting biopsies from stomach tissue. -

Medicine Hx- Gastrointestinal System History of “Heartburn”
Medicine Hx- Gastrointestinal System History of “Heartburn” A. Overview: GORD is common, and is said to exist when reflux of stomach contents (acid ± bile) causes troublesome symptoms (≥2 heartburn episodes/wk) and/or complications. If reflux is prolonged, it may cause oesophagitis, benign oesophageal stricture or Barrett’s oesophagus. Causes: lower oesophageal sphincter hypotension, hiatus hernia, loss of oesophageal peristaltic function, abdominal obesity, gastric acid hypersecretion, slow gastric emptying, overeating, smoking, alcohol, pregnancy, surgery in achalasia, drugs (tricyclics, anticholinergics, nitrates), systemic sclerosis. Symptoms: 1. Heartburn (burning, retrosternal discomfort after meals, lying, stooping or straining, relieved by antacids) 2. Belching; acid brash (acid or bile regurgitation) 3. Waterbrash (Increased salivation: “My mouth fills with saliva”) 4. Odynophagia (painful swallowing, eg from oesophagitis or ulceration). 5. Extra-oesophageal: Nocturnal asthma, chronic cough, laryngitis (hoarseness, throat clearing), sinusitis. (From Oxford Handbook Of Clinical Medicine p244) Don’t confuse between acid regurgitation and waterbrash: -Acid regurgitation: the patient experiences a sour or bitter tasting fluid coming up into the mouth. This symptom strongly suggests that the reflux is occurring. -Waterbrash: excessive secretion of saliva into the mouth may occur, uncommonly, in patients with peptic ulcer disease or oesophagitis. The patient experience tasteless or salty fluid his mouth. B. Differential diagnosis: -

Crohn's Disease and Diet
Crohn’s Disease and Diet What is Crohn’s Disease? Crohn’s disease is a condition that causes inflammation in the intestine. The symptoms of Crohn’s disease depend on the severity of the disease and what part of the intestine is affected. The most common symptoms are abdominal pain/cramping, diarrhea and fever. Can Diet Help? The following diet recommendations can help you to: Manage symptoms of Crohn’s disease Maintain normal bowel function Keep well nourished Diet Recommendations for Crohn’s Disease People living with Crohn’s disease often have periods of remission (mild or no symptoms) in addition to periods of flare-up (moderate or severe symptoms). The diet recommendations for Crohn’s disease depend on whether you are in a remission period or a flare- up period. Follow the diet recommendations that are appropriate for the period that you are in (see Flare-up Period or Remission Period below) . Flare-up Period When the small intestine is inflamed during a flare-up, the inside of the small bowel can become narrow. This can make it more difficult for high residue foods (i.e. bulky food or food with coarse Flare-up Period (continued) 1 particles) to pass through. High residue foods can therefore cause cramping or abdominal pain during a flare-up. It may help to follow a low-residue diet during this time. See Appendix 1 - Low Residue Diet for foods that are recommended. When your symptoms improve (i.e. you enter the remission period), you can start to add high residue foods back into your diet as tolerated. -

Dyspepsia (Indigestion)
Indigestion (dydpepsia). Indigestion information - Patient | Patient Page 1 of 5 View this article online at https://patient.info/health/dyspepsia-indigestion Dyspepsia (Indigestion) Dyspepsia (indigestion) is a term which describes pain and sometimes other symptoms which come from your upper gut (the stomach, oesophagus or duodenum). There are various causes (described below). Treatment depends on the likely cause. Understanding digestion Food passes down the gullet (oesophagus) into the stomach. The stomach makes acid which is not essential but helps to digest food. Food then passes gradually into the first part of the small intestine (the duodenum). In the duodenum and the rest of the small intestine, food mixes with chemicals called enzymes. The enzymes come from the pancreas and from cells lining the intestine. The enzymes break down (digest) the food. Digested food is then absorbed into the body from the small intestine. What is dyspepsia? Dyspepsia is a term which includes a group of symptoms that come from a problem in your upper gut. The gut (gastrointestinal tract) is the tube that starts at the mouth and ends at the anus. The upper gut includes the oesophagus, stomach and duodenum. Various conditions cause dyspepsia. The main symptom is usually pain or discomfort in the upper tummy (abdomen). In addition, other symptoms that may develop include: • Bloating. • Belching. • Quickly feeling full after eating. • Feeling sick (nausea). • Being sick (vomiting). Symptoms are often related to eating. Doctors used to include heartburn (a burning sensation felt in the lower chest area) and bitter-tasting liquid coming up into the back of the throat (sometimes called 'waterbrash') as symptoms of dyspepsia. -

Medicines That Affect Fluid Balance in the Body
the bulk of stools by getting them to retain liquid, which encourages the Medicines that affect fluid bowels to push them out. balance in the body Osmotic laxatives e.g. Lactulose, Macrogol - these soften stools by increasing the amount of water released into the bowels, making them easier to pass. Older people are at higher risk of dehydration due to body changes in the ageing process. The risk of dehydration can be increased further when Stimulant laxatives e.g. Senna, Bisacodyl - these stimulate the bowels elderly patients are prescribed medicines for chronic conditions due to old speeding up bowel movements and so less water is absorbed from the age. stool as it passes through the bowels. Some medicines can affect fluid balance in the body and this may result in more water being lost through the kidneys as urine. Stool softener laxatives e.g. Docusate - These can cause more water to The medicines that can increase risk of dehydration are be reabsorbed from the bowel, making the stools softer. listed below. ANTACIDS Antacids are also known to cause dehydration because of the moisture DIURETICS they require when being absorbed by your body. Drinking plenty of water Diuretics are sometimes called 'water tablets' because they can cause you can reduce the dry mouth, stomach cramps and dry skin that is sometimes to pass more urine than usual. They work on the kidneys by increasing the associated with antacids. amount of salt and water that comes out through the urine. Diuretics are often prescribed for heart failure patients and sometimes for patients with The major side effect of antacids containing magnesium is diarrhoea and high blood pressure. -

Abdominal Pain - Gastroesophageal Reflux Disease
ACS/ASE Medical Student Core Curriculum Abdominal Pain - Gastroesophageal Reflux Disease ABDOMINAL PAIN - GASTROESOPHAGEAL REFLUX DISEASE Epidemiology and Pathophysiology Gastroesophageal reflux disease (GERD) is one of the most commonly encountered benign foregut disorders. Approximately 20-40% of adults in the United States experience chronic GERD symptoms, and these rates are rising rapidly. GERD is the most common gastrointestinal-related disorder that is managed in outpatient primary care clinics. GERD is defined as a condition which develops when stomach contents reflux into the esophagus causing bothersome symptoms and/or complications. Mechanical failure of the antireflux mechanism is considered the cause of GERD. Mechanical failure can be secondary to functional defects of the lower esophageal sphincter or anatomic defects that result from a hiatal or paraesophageal hernia. These defects can include widening of the diaphragmatic hiatus, disturbance of the angle of His, loss of the gastroesophageal flap valve, displacement of lower esophageal sphincter into the chest, and/or failure of the phrenoesophageal membrane. Symptoms, however, can be accentuated by a variety of factors including dietary habits, eating behaviors, obesity, pregnancy, medications, delayed gastric emptying, altered esophageal mucosal resistance, and/or impaired esophageal clearance. Signs and Symptoms Typical GERD symptoms include heartburn, regurgitation, dysphagia, excessive eructation, and epigastric pain. Patients can also present with extra-esophageal symptoms including cough, hoarse voice, sore throat, and/or globus. GERD can present with a wide spectrum of disease severity ranging from mild, intermittent symptoms to severe, daily symptoms with associated esophageal and/or airway damage. For example, severe GERD can contribute to shortness of breath, worsening asthma, and/or recurrent aspiration pneumonia. -

Ijcep0048253.Pdf
Int J Clin Exp Pathol 2017;10(4):4089-4098 www.ijcep.com /ISSN:1936-2625/IJCEP0048253 Original Article Comparative effectiveness of different recommended doses of omeprazole and lansoprazole for gastroesophageal reflux disease: a meta-analysis of published data Feng Liu1, Jing Wang1, Hailong Wu1, Hui Wang2, Jianxiang Wang1, Rui Zhou1, Zhi Zhu3 Departments of 1Surgery, 2Gastroenterology, 3Epidemiology and Biostatistics, Puai Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China Received January 6, 2017; Accepted February 20, 2017; Epub April 1, 2017; Published April 15, 2017 Abstract: This meta-analysis aims to evaluate the effectiveness of different recommended doses of omeprazole and lansoprazole on gastroesophageal reflux diseases (GERD) in adults. The electronic databases of PubMed, EMBASE, Cochrane Library, and ClinicalTrials.gov were searched before September 13 2016. Fifteen eligible studies were identified involving 8752 patients in our meta-analysis. For the healing outcome of esophagitis, compared with 15 mg per day of lansoprazole, there were significant difference of both 30 mg per day of lansoprazole (RR=1.29, 95% CI [1.01, 1.66], I2=79.3%, P=0.028) and 60 mg per day of lansoprazole (RR=1.59, 95% CI [1.28, 1.99], I2=Not ap- plicable (NA), P=NA), and the other result were not significantly different between 60 mg per day and 30 mg per day. For relief of symptoms, our result indicated a significant difference between 20 mg per day and 10 mg per day of omeprazole (RR=1.21, 95% CI [1.06, 1.39], I2=53.9%, P=0.089); the overall result indicated a significant difference between lansoprazole and omeprazole (RR=0.93, 95% CI [0.86, 0.999], I2=60.7%, P=0.038). -
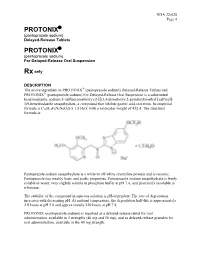
Protonix Protonix
NDA 22-020 Page 4 PROTONIX® (pantoprazole sodium) Delayed-Release Tablets PROTONIX® (pantoprazole sodium) For Delayed-Release Oral Suspension Rx only DESCRIPTION ® The active ingredient in PROTONIX (pantoprazole sodium) Delayed-Release Tablets and ® PROTONIX (pantoprazole sodium) For Delayed-Release Oral Suspension is a substituted benzimidazole, sodium 5-(difluoromethoxy)-2-[[(3,4-dimethoxy-2-pyridinyl)methyl] sulfinyl]- 1H-benzimidazole sesquihydrate, a compound that inhibits gastric acid secretion. Its empirical formula is C16H14F2N3NaO4S x 1.5 H2O, with a molecular weight of 432.4. The structural formula is: Pantoprazole sodium sesquihydrate is a white to off-white crystalline powder and is racemic. Pantoprazole has weakly basic and acidic properties. Pantoprazole sodium sesquihydrate is freely soluble in water, very slightly soluble in phosphate buffer at pH 7.4, and practically insoluble in n-hexane. The stability of the compound in aqueous solution is pH-dependent. The rate of degradation increases with decreasing pH. At ambient temperature, the degradation half-life is approximately 2.8 hours at pH 5.0 and approximately 220 hours at pH 7.8. PROTONIX (pantoprazole sodium) is supplied as a delayed-release tablet for oral administration, available in 2 strengths (40 mg and 20 mg); and as delayed-release granules for oral administration, available in the 40 mg strength. NDA 22-020 Page 5 Each PROTONIX (pantoprazole sodium) Delayed-Release tablet contains 45.1 mg or 22.6 mg of pantoprazole sodium sesquihydrate (equivalent to 40 mg or 20 mg pantoprazole, respectively) with the following inactive ingredients: calcium stearate, crospovidone, hypromellose, iron oxide, mannitol, methacrylic acid copolymer, polysorbate 80, povidone, propylene glycol, sodium carbonate, sodium lauryl sulfate, titanium dioxide, and triethyl citrate. -

Proton Pump Inhibitors (PPI) Preferred Step Therapy Program Annual Review Date: 01/18/2021
Policy: Proton Pump Inhibitors (PPI) Preferred Step Therapy Program Annual Review Date: 01/18/2021 Impacted Last Revised Date: Drugs: • Aciphex, Aciphex Sprinkle • Dexilant 06/17/2021 • Esomeprazole DR, esomeprazole strontium DR • Nexium • Omeprazole/sodium bicarbonate • Prevacid, Prevacid 24HR, Prevacid SoluTab • Prilosec • Protonix • Rabeprazole DR OVERVIEW Proton pump inhibitors (PPIs) [i.e., esomeprazole, dexlansoprazole, lansoprazole, omeprazole, pantoprazole, and rabeprazole] are commonly used antisecretory agents that are highly effective at suppressing gastric acid and subsequently treating associated conditions, including gastroesophageal reflux disease (GERD). Omeprazole is available generically and over-the-counter (OTC). Omeprazole OTC is prescription strength (20 mg). Lansoprazole is also available generically and OTC. Lansoprazole OTC is available as 15 mg capsules. Zegerid capsules are available generically and OTC; the OTC product contains omeprazole 20 mg and sodium bicarbonate 1100 mg. Nexium® 24HR (esomeprazole magnesium 22.3 mg delayed-release capsules) is available OTC and is equivalent to 20 mg of esomeprazole base. The OTC products are indicated for the short-term (14 days) treatment of heartburn. Patients should not take the OTC products for more than 14 days or more often than every 4 months unless under the supervision of a physician. Although the PPIs vary in their specific Food and Drug Administration (FDA)-approved indications, all of the PPIs have demonstrated the ability to control GERD symptoms and to heal esophagitis when used at prescription doses. Most comparative studies between PPIs to date have demonstrated comparable efficacies for acid-related diseases, including duodenal and gastric ulcerations, GERD, Zollinger-Ellison syndrome, and H. pylori eradication therapies. Though the available clinical data are not entirely complete for the comparison of these agents, many clinical trials have shown the PPIs to be similar in safety and efficacy.