Ijcep0048253.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
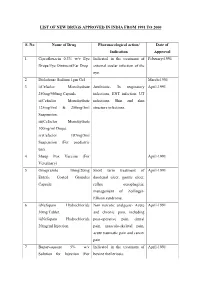
List of New Drugs Approved in India from 1991 to 2000
LIST OF NEW DRUGS APPROVED IN INDIA FROM 1991 TO 2000 S. No Name of Drug Pharmacological action/ Date of Indication Approval 1 Ciprofloxacin 0.3% w/v Eye Indicated in the treatment of February-1991 Drops/Eye Ointment/Ear Drop external ocular infection of the eye. 2 Diclofenac Sodium 1gm Gel March-1991 3 i)Cefaclor Monohydrate Antibiotic- In respiratory April-1991 250mg/500mg Capsule. infections, ENT infection, UT ii)Cefaclor Monohydrate infections, Skin and skin 125mg/5ml & 250mg/5ml structure infections. Suspension. iii)Cefaclor Monohydrate 100mg/ml Drops. iv)Cefaclor 187mg/5ml Suspension (For paediatric use). 4 Sheep Pox Vaccine (For April-1991 Veterinary) 5 Omeprazole 10mg/20mg Short term treatment of April-1991 Enteric Coated Granules duodenal ulcer, gastric ulcer, Capsule reflux oesophagitis, management of Zollinger- Ellison syndrome. 6 i)Nefopam Hydrochloride Non narcotic analgesic- Acute April-1991 30mg Tablet. and chronic pain, including ii)Nefopam Hydrochloride post-operative pain, dental 20mg/ml Injection. pain, musculo-skeletal pain, acute traumatic pain and cancer pain. 7 Buparvaquone 5% w/v Indicated in the treatment of April-1991 Solution for Injection (For bovine theileriosis. Veterinary) 8 i)Kitotifen Fumerate 1mg Anti asthmatic drug- Indicated May-1991 Tablet in prophylactic treatment of ii)Kitotifen Fumerate Syrup bronchial asthma, symptomatic iii)Ketotifen Fumerate Nasal improvement of allergic Drops conditions including rhinitis and conjunctivitis. 9 i)Pefloxacin Mesylate Antibacterial- In the treatment May-1991 Dihydrate 400mg Film Coated of severe infection in adults Tablet caused by sensitive ii)Pefloxacin Mesylate microorganism (gram -ve Dihydrate 400mg/5ml Injection pathogens and staphylococci). iii)Pefloxacin Mesylate Dihydrate 400mg I.V Bottles of 100ml/200ml 10 Ofloxacin 100mg/50ml & Indicated in RTI, UTI, May-1991 200mg/100ml vial Infusion gynaecological infection, skin/soft lesion infection. -

Proton Pump Inhibitors (PPI) Preferred Step Therapy Program Annual Review Date: 01/18/2021
Policy: Proton Pump Inhibitors (PPI) Preferred Step Therapy Program Annual Review Date: 01/18/2021 Impacted Last Revised Date: Drugs: • Aciphex, Aciphex Sprinkle • Dexilant 06/17/2021 • Esomeprazole DR, esomeprazole strontium DR • Nexium • Omeprazole/sodium bicarbonate • Prevacid, Prevacid 24HR, Prevacid SoluTab • Prilosec • Protonix • Rabeprazole DR OVERVIEW Proton pump inhibitors (PPIs) [i.e., esomeprazole, dexlansoprazole, lansoprazole, omeprazole, pantoprazole, and rabeprazole] are commonly used antisecretory agents that are highly effective at suppressing gastric acid and subsequently treating associated conditions, including gastroesophageal reflux disease (GERD). Omeprazole is available generically and over-the-counter (OTC). Omeprazole OTC is prescription strength (20 mg). Lansoprazole is also available generically and OTC. Lansoprazole OTC is available as 15 mg capsules. Zegerid capsules are available generically and OTC; the OTC product contains omeprazole 20 mg and sodium bicarbonate 1100 mg. Nexium® 24HR (esomeprazole magnesium 22.3 mg delayed-release capsules) is available OTC and is equivalent to 20 mg of esomeprazole base. The OTC products are indicated for the short-term (14 days) treatment of heartburn. Patients should not take the OTC products for more than 14 days or more often than every 4 months unless under the supervision of a physician. Although the PPIs vary in their specific Food and Drug Administration (FDA)-approved indications, all of the PPIs have demonstrated the ability to control GERD symptoms and to heal esophagitis when used at prescription doses. Most comparative studies between PPIs to date have demonstrated comparable efficacies for acid-related diseases, including duodenal and gastric ulcerations, GERD, Zollinger-Ellison syndrome, and H. pylori eradication therapies. Though the available clinical data are not entirely complete for the comparison of these agents, many clinical trials have shown the PPIs to be similar in safety and efficacy. -

Proton Pump Inhibitors
MEDICATION POLICY: Proton Pump Inhibitors Generic Name: Proton Pump Inhibitors Preferred: Esomeprazole (generic), Lansoprazole (generic), Omeprazole (generic), Therapeutic Class or Brand Name: Proton Pantoprazole (generic), and Rabeprazole Pump Inhibitors (generic) Applicable Drugs (if Therapeutic Class): Non-preferred: Aciphex® (rabeprazole), Esomeprazole (generic), Lansoprazole Dexilant® (dexlansoprazole), Nexium® (generic), Omeprazole (generic), Pantoprazole (esomeprazole), Not Medically Necessary: (generic), and Rabeprazole (generic). Omeprazole/Sodium Bicarbonate (generic), Aciphex® (rabeprazole), Dexilant® Zegerid® (omeprazole/sodium bicarbonate). (dexlansoprazole), Nexium® (esomeprazole), Prevacid® (lansoprazole), Prilosec® Date of Origin: 2/1/2013 (omeprazole), and Protonix® (pantoprazole). Date Last Reviewed / Revised: 12/23/2020 Omeprazole/Sodium Bicarbonate (generic), Zegerid® (omeprazole/sodium bicarbonate). Policy also applies to any other Proton Pump Inhibitors not listed. GPI Code: 4927002000, 4927002510, 4927004000, 4927006000, 4927007010, 4927007610, 4999600260 PRIOR AUTHORIZATION CRITERIA (May be considered medically necessary when criteria I and II are met) I. Documented diagnosis of one of the following A through G: A. Gastroesophageal reflux disease (GERD). B. Erosive esophagitis. C. Gastric ulcers. D. Risk reduction of NSAID-associated gastric ulcer. E. Duodenal ulcers. F. Eradication of H. pylori. G. Hypersecretory conditions II. Non-preferred PPIs require documented trials and failures of all generic PPIs. EXCLUSION -

Dr. Reddy's – Recall of Ranitidine
Dr. Reddy’s – Recall of ranitidine • On October 23, 2019, Dr. Reddy’s announced the voluntary, consumer-level recall of prescription ranitidine due to potential contamination with N-nitrosodimethylamine (NDMA). • Dr. Reddy’s initially announced retail level recalls for prescription and OTC ranitidine in early October; however, the recall of prescription ranitidine products has been escalated to the consumer level. The recall of OTC ranitidine remains at the retail level. Prescription Ranitidine Capsules Recalled by Dr. Reddy’s Product Description NDC# Ranitidine 150 mg capsules, 60 count bottle 55111-129-60 Ranitidine 150 mg capsules, 500 count bottle 55111-129-05 Ranitidine 300 mg capsules, 30 count bottle 55111-130-30 Ranitidine 300 mg capsules, 100 count bottle 55111-130-01 • Refer to the Dr. Reddy’s announcement for a complete list of the OTC recalled ranitidine products. • Other manufacturers, including Apotex, Perrigo and Sanofi have recently announced retail level recalls of their OTC ranitidine products. • In September, Sandoz issued a consumer level recall of prescription ranitidine products. • These recalls follow a recent FDA statement about NDMA impurities detected in ranitidine medicines. • NDMA is classified as a probable human carcinogen based on results from laboratory tests. NDMA is a known environmental contaminant and found in water and foods, including meats, dairy products, and vegetables. • Ranitidine is an OTC and prescription drug. Ranitidine is an H2 (histamine-2) blocker, which decreases the amount of acid created by the stomach. OTC ranitidine is approved to prevent and relieve heartburn associated with acid ingestion and sour stomach. • Prescription ranitidine is approved for multiple indications, including treatment and prevention of ulcers of the stomach and intestines and treatment of gastroesophageal reflux disease. -

Cimetidine As a Last Resort
Primary Care Guidance for Reviewing Patients on All Oral Formulations of Ranitidine (In response to Supply Disruption Alert dated 15 October 2019) Patients on ALL oral formulations of RANITIDINE Yes Can ranitidine be stopped or stepped down Stop / Try antacids to an antacid/alginate? No Can treatment be changed to a PPI? No Yes Patients who clinically should remain on ranitidine but has Children (Under 18 years old) now been withdrawn: On dual treatment of ranitidine and PPI and unsuitable for step-down ‘Simple’ GORD or Severe reflux o Consider maximising dose of PPI and trial without absence of oesophagitis, GI ranitidine if required. complex medical ulcer, complex On ranitidine for pre-chemotherapy prevention history medical history o This will be reviewed in secondary care. requiring acid On ranitidine due to C.diff risk with PPI reduction o Current or recent episode of C Difficile, or previously Stop ranitidine if had C Difficile and currently on antibiotics and are at possible and high risk. See recommendations below. recommend Allergic or intolerant to PPI or PPI contraindicated (e.g. dietary measures due to interstitial nephritis, acute kidney injury, previous hyponatraemia with PPI etc). See recommendations or antacids below. Always Check Weight Recommendations: Suitable PPI alternatives: 1. At time of publication (January 2020) Ranitidine is no longer available for supply. Consider if an H2 antagonist is still required. 1st line - Omeprazole capsule or dispersible tablets. Direction: Disperse tablet (or half of) in 5-10ml of water. For 5mg dose half the tablet before dispersing 2. If an H2 antagonist is required for children (over 1 year), consider switching to cimetidine as a last resort. -

PHRP March 2015
March 2015; Vol. 25(2):e2521518 doi: http://dx.doi.org/10.17061/phrp2521518 www.phrp.com.au Research Manual versus automated coding of free-text self-reported medication data in the 45 and Up Study: a validation study Danijela Gnjidica,b,i, Sallie-Anne Pearsona,c, Sarah N Hilmerb,d, Jim Basilakise, Andrea L Schaffera, Fiona M Blythb,f,g and Emily Banksg,h, on behalf of the High Risk Prescribing Investigators a Faculty of Pharmacy, University of Sydney, NSW, Australia b Sydney Medical School, University of Sydney, NSW, Australia c Sydney School of Public Health, University of Sydney, NSW, Australia d Royal North Shore Hospital and Kolling Institute of Medical Research, Sydney, NSW, Australia e School of Computing, Engineering and Mathematics, University of Western Sydney, NSW, Australia f Centre for Education and Research on Ageing (CERA), Concord Hospital, Sydney, NSW, Australia g The Sax Institute, Sydney, NSW, Australia h National Centre for Epidemiology and Population Health, Australian National University, Canberra, ACT i Corresponding author: [email protected] Article history Abstract Publication date: March 2015 Background: Increasingly, automated methods are being used to code free- Citation: Gnjidic D, Pearson S, Hilmer S, text medication data, but evidence on the validity of these methods is limited. Basilakis J, Schaffer AL, Blyth FM, Banks E. To examine the accuracy of automated coding of previously keyed Manual versus automated coding of free-text Aim: in free-text medication data compared with manual coding of original self-reported medication data in the 45 and Up Study: a validation study. Public Health handwritten free-text responses (the ‘gold standard’). -

New and Future Drug Development for Gastroesophageal Reflux Disease
J Neurogastroenterol Motil, Vol. 20 No. 1 January, 2014 pISSN: 2093-0879 eISSN: 2093-0887 http://dx.doi.org/10.5056/jnm.2014.20.1.6 JNM Journal of Neurogastroenterology and Motility Review New and Future Drug Development for Gastroesophageal Reflux Disease Carla Maradey-Romero and Ronnie Fass* The Esophageal and Swallowing Center, Division of Gastroenterology and Hepatology, MetroHealth Medical Center, Case Western Reserve University, Cleveland, Ohio, USA Medical therapy remains the most popular treatment for gastroesophageal reflux disease (GERD). Whilst interest in drug devel- opment for GERD has declined over the last few years primarily due to the conversion of most proton pump inhibitor (PPI)’s to generic and over the counter compounds, there are still numerous areas of unmet needs in GERD. Drug development has been focused on potent histamine type 2 receptor antagonist’s, extended release PPI’s, PPI combination, potassium-competitive acid blockers, transient lower esophageal sphincter relaxation reducers, prokinetics, mucosal protectants and esophageal pain modulators. It is likely that the aforementioned compounds will be niched for specific areas of unmet need in GERD, rather than compete with the presently available anti-reflux therapies. (J Neurogastroenterol Motil 2014;20:6-16) Key Words Erosive esophagitis; Gastroesophageal reflux; Heartburn; Proton pump inhibitors Most patients with GERD fall into 1 of 3 categories: non- erosive reflux disease (NERD), erosive esophagitis (EE), and Introduction Barrett’s esophagus (BE). The 2 main phenotypes of GERD, Gastroesophageal reflux disease (GERD) is a common con- NERD and EE, appear to have different pathophysiological and dition that develops when reflux of stomach contents cause trou- clinical characteristics. -

PRV0509 R9, May 2009 PREVACID Naprapac 500 (Lansoprazole
Page 1 of 34 (No. 1546) PRV0509 R9, May 2009 PREVACID® NapraPAC ®500 (lansoprazole delayed-release 15 mg capsules and naproxen 500 mg tablets kit) Rx only Cardiovascular Risk • NSAIDs (a nonsteroidal anti-inflammatory drug) may cause an increased risk of serious cardiovascular thrombotic events, myocardial infarction, and stroke, which can be fatal. This risk may increase with duration of use. Patients with cardiovascular disease or risk factors for cardiovascular disease may be at greater risk (see WARNINGS). • PREVACID NapraPAC is contraindicated for the treatment of peri-operative pain in the setting of coronary artery bypass graft (CABG) surgery (see WARNINGS). Gastrointestinal (GI) Risk • NSAIDs cause an increased risk of serious GI adverse events including bleeding and perforation of the stomach and intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Patients with a history of gastric and/or duodenal ulcers (especially patients with a history of bleeding or perforation) and geriatric patients are at greater risk for serious GI events (see WARNINGS and CLINICAL STUDIES, Risk Reduction of NSAID-Associated Gastric Ulcer(s)). PREVACID® NapraPAC ®500 is a combination package containing two individual drug products: PREVACID® (lansoprazole) Delayed-Release Capsules, a proton pump inhibitor (PPI), and NAPROSYN® (naproxen tablets), a nonsteroidal anti-inflammatory drug (NSAID) with analgesic and antipyretic properties. The information described in this labeling concerns only the use of these products as indicated in this combination package and does not include all individual use information. For information on use of the components when dispensed as individual medications outside this combination package, please see the package inserts for PREVACID Delayed-Release Capsules and NAPROSYN Tablets. -

Early Effects of Oral Administration of Omeprazole and Roxatidine on Intragastric Ph
Iida et al. / J Zhejiang Univ-Sci B (Biomed & Biotechnol) 2012 13(1):29-34 29 Journal of Zhejiang University-SCIENCE B (Biomedicine & Biotechnology) ISSN 1673-1581 (Print); ISSN 1862-1783 (Online) www.zju.edu.cn/jzus; www.springerlink.com E-mail: [email protected] Early effects of oral administration of omeprazole and roxatidine on intragastric pH Hiroshi IIDA1, Shingo KATO1, Yusuke SEKINO1, Eiji SAKAI1, Takashi UCHIYAMA1, Hiroki ENDO1, Kunihiro HOSONO1, Yasunari SAKAMOTO1, Koji FUJITA1, Masato YONEDA1, Tomoko KOIDE1, Hirokazu TAKAHASHI1, Chikako TOKORO1, Ayumu GOTO1, Yasunobu ABE1, Noritoshi KOBAYASHI1, Kensuke KUBOTA1, Eiji GOTOH2, Shin MAEDA1, Atsushi NAKAJIMA1, Masahiko INAMORI†‡1,3 (1Gastroenterology Division, Yokohama City University School of Medicine, Yokohama 236-0004, Japan) (2Department of Medical Education, Yokohama City University School of Medicine, Yokohama 236-0004, Japan) (3Office of Postgraduate Medical Education, Yokohama City University Hospital, Yokohama 236-0004, Japan) †E-mail: [email protected] Received Mar. 14, 2011; Revision accepted Aug. 30, 2011; Crosschecked Dec. 2, 2011 Abstract: Objective: The ideal medication for the treatment of acid-related diseases, e.g., peptic ulcers, stress- related gastric bleeding, functional dyspepsia, and gastroesophageal reflux disease, should have a rapid onset of action to promote hemostasis and relieve the symptoms. The aim of our study was to investigate the inhibitory effects on gastric acid secretion of a single oral administration of a proton pump inhibitor, omeprazole 20 mg, and an H2-receptor antagonist, roxatidine 75 mg. Methods: Ten Helicobacter pylori-negative male subjects participated in this randomized, two-way crossover study. Intragastric pH was monitored continuously for 6 h after single oral admini- stration of omeprazole 20 mg and roxatidine 75 mg. -

MEDICATION GUIDE Lansoprazole (Lan-SO-Pruh-Zole) Delayed
MEDICATION GUIDE Lansoprazole (lan-SO-pruh-zole) Delayed-release Capsules, USP Read this Medication Guide before you start taking lansoprazole delayed-release capsules and each time you get a refill. There may be new information. This information does not take the place of talking to your doctor about your medical condition or your treatment. What is the most important information that I should know about lansoprazole delayed-release capsules? Lansoprazole delayed-release capsules may help your acid-related symptoms, but you could still have serious stomach problems. Talk with your doctor. Lansoprazole delayed-release capsules can cause serious side effects, including: • Diarrhea. Lansoprazole delayed-release capsules may increase your risk of getting severe diarrhea. This diarrhea may be caused by an infection (Clostridium difficile ) in your intestines. Call your doctor right away if you have watery stool, stomach pain, and fever that does not go away. • Bone fractures. People who take multiple daily doses of proton pump inhibitor medicines for a long period of time (a year or longer) may have an increased risk of fractures of the hip, wrist or spine. You should take lansoprazole delayed-release capsules exactly as prescribed, at the lowest dose possible for your treatment and for the shortest time needed. Talk to your doctor about your risk of bone fracture if you take lansoprazole delayed-release capsules. Lansoprazole delayed-release capsules can have other serious side effects. See "What are the possible side effects of lansoprazole delayed-release capsules?" What is lansoprazole delayed-release capsule? Lansoprazole delayed-release capsule is a prescription medicine called a proton pump inhibitor (PPI). -

Histamine H2-Antagonists, Proton Pump Inhibitors and Other Drugs That Alter Gastric Acidity
Jack DeRuiter, Principles of Drug Action 2, Fall 2001 HISTAMINE H2-ANTAGONISTS, PROTON PUMP INHIBITORS AND OTHER DRUGS THAT ALTER GASTRIC ACIDITY I. Introduction Peptide ulcer disease (PUD) is a group of upper gastrointestinal tract disorders that result from the erosive action of acid and pepsin. Duodenal ulcer (DU) and gastric ulcer (GU) are the most common forms although PUD may occur in the esophagus or small intestine. Factors that are involved in the pathogenesis and recurrence of PUD include hypersecretion of acid and pepsin and GI infection by Helicobacter pylori, a gram-negative spiral bacterium. H. Pylori has been found in virtually all patients with DU and approximately 75% of patients with GU. Some risk factors associated with recurrence of PUD include cigarette smoking, chronic use of ulcerogenic drugs (e.g. NSAIDs), male gender, age, alcohol consumption, emotional stress and family history. The goals of PUD therapy are to promote healing, relieve pain and prevent ulcer complications and recurrences. Medications used to heal or reduce ulcer recurrence include antacids, antimuscarinic drugs, histamine H2-receptor antagonists, protective mucosal barriers, proton pump inhibitors, prostaglandins and bismuth salt/antibiotic combinations. A characteristic feature of the stomach is its ability to secrete acid as part of its involvement in digesting food for absorption later in the intestine. The presence of acid and proteolytic pepsin enzymes, whose formation from pepsinogen is facilitated by the low gastric pH, is generally assumed to be required for the hydrolysis of proteins and other foods. The acid secretory unit of the gastric + + mucosa is the parietal (oxyntic) cell. -

PREVACID (Lansoprazole)
HIGHLIGHTS OF PRESCRIBING INFORMATION ----------------------------CONTRAINDICATIONS---------------------------- These highlights do not include all the information needed to use • Contraindicated in patients with known severe hypersensitivity to PREVACID and PREVACID SOLUTAB safely and effectively. See any component of the PREVACID or PREVACID SoluTab full prescribing information for PREVACID and PREVACID formulations. (4) SOLUTAB. • Patients receiving rilpivirine-containing products. (4, 7) PREVACID (lansoprazole) delayed-release capsules, for oral use PREVACID SOLUTAB (lansoprazole) delayed-release orally ---------------------WARNINGS AND PRECAUTIONS------------------- disintegrating tablets • Gastric Malignancy: In adults, symptomatic response with Initial U.S. Approval: 1995 PREVACID or PREVACID SoluTab does not preclude the presence of gastric malignancy. Consider additional follow-up and --------------------------RECENT MAJOR CHANGES--------------------------- diagnostic testing. (5.1) Contraindications (4) 07/2017 • Acute Interstitial Nephritis: Acute interstitial nephritis has been Warnings and Precautions observed in patients taking PPIs. (5.2) Interactions with Investigations for Neuroendocrine • Clostridium difficile-Associated Diarrhea: PPI therapy may be Tumors (5.8) 07/2017 associated with increased risk of Clostridium-difficile associated Patients with Phenylketonuria (5.10) 07/2017 diarrhea. (5.3) • Bone Fracture: Long-term and multiple daily dose PPI therapy --------------------------INDICATIONS AND USAGE----------------------------