Nitrates for the Management of Acute Heart Failure Syndromes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Drug Class Review Antianginal Agents
Drug Class Review Antianginal Agents 24:12.08 Nitrates and Nitrites 24:04.92 Cardiac Drugs, Miscellaneous Amyl Nitrite Isosorbide Dinitrate (IsoDitrate ER®, others) Isosorbide Mononitrate (Imdur®) Nitroglycerin (Minitran®, Nitrostat®, others) Ranolazine (Ranexa®) Final Report May 2015 Review prepared by: Melissa Archer, PharmD, Clinical Pharmacist Carin Steinvoort, PharmD, Clinical Pharmacist Gary Oderda, PharmD, MPH, Professor University of Utah College of Pharmacy Copyright © 2015 by University of Utah College of Pharmacy Salt Lake City, Utah. All rights reserved. Table of Contents Executive Summary ......................................................................................................................... 3 Introduction .................................................................................................................................... 4 Table 1. Antianginal Therapies .............................................................................................. 4 Table 2. Summary of Agents .................................................................................................. 5 Disease Overview ........................................................................................................................ 8 Table 3. Summary of Current Clinical Practice Guidelines .................................................... 9 Pharmacology ............................................................................................................................... 10 Table 4. Pharmacokinetic Properties -

List of Union Reference Dates A
Active substance name (INN) EU DLP BfArM / BAH DLP yearly PSUR 6-month-PSUR yearly PSUR bis DLP (List of Union PSUR Submission Reference Dates and Frequency (List of Union Frequency of Reference Dates and submission of Periodic Frequency of submission of Safety Update Reports, Periodic Safety Update 30 Nov. 2012) Reports, 30 Nov. -
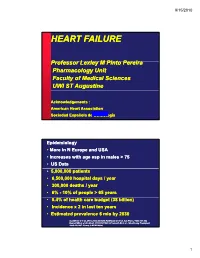
Heart Failure
9/15/2010 HEART FAILURE PfProfessor LlLexley M MPitP Pinto Perei ra Pharmacology Unit Faculty of Medical Sciences UWI ST Augustine Acknowledgements : American Heart Association Sociedad Española de CardiologíaJune, 1999 Epidemiology • More in N Europe and USA • Increases with age esp in males > 75 • US Data • 5,000,000 patients • 6,500,000 hospital days/ year • 300,000 deaths / year • 6% --10%10% of people > 65 years • 5.4%f% of health care budget (38 billion) • Incidence x 2 in last ten years • Estimated prevalence 6 mio by 2030 Gottdiener J et al. JACC 2000;35:1628, Haldeman GA et al. Am Heart J 1999;137:352 Kannel WB et al. Am Heart J 1991;121:951, O’Connell JB et al. J Heart Lung Transplant 1993;13:S107, Young J, MCNA 2004; 1 9/15/2010 Definition of heart failure Clinical syyyndrome that can result from any structural or functional cardiac disorder that impairs the ability of the ventricle to fill with or eject blood AHA / ACC HF guidelines 2001 Clinical symptoms / signs secondary to abnormal ventricular function ESC HF guidelines 2001 “Heart Failure” vs. “Congestive Heart Failure” All patients may NOT have volume overload at the time of initial or subsequent evaluation. Therefore the term “heart failure” is preferred over the older term “ihfil”“congestive heart failure.” CHF is a significant cause of morbidity and mortality Important cause of hospitalizations among elderly 2 9/15/2010 Causes of HF For a substantial proportion of patients, the causes of HF are: 1. Coronary artery disease 2. Hypertension 3. Dilated cardiomyopathy And there are other causes 1. -

Effects of Intravenous Nicorandil on the Mid-Term Prognosis of Patients
Circulation Journal ORIGINAL ARTICLE Official Journal of the Japanese Circulation Society http://www.j-circ.or.jp Heart Failure Effects of Intravenous Nicorandil on the Mid-Term Prognosis of Patients With Acute Heart Failure Syndrome Shiro Ishihara, MD; Tokushi Koga, MD; Shigeru Kaseda, MD; Eiji Nyuta, MD; Yoshie Haga, MD; Shinichiro Fujishima, MD; Takao Ishitsuka, MD; Seizo Sadoshima, MD Background: Acute heart failure syndrome (AHFS) remains a major clinical challenge because of its poor prognosis. Nicorandil, a hybrid compound of a potassium-channel opener and nitric oxide donor, has been reported to improve the prognosis of ischemic heart disease. We sought to evaluate the effect of intravenous nicorandil on the mid-term prognosis of AHFS. Methods and Results: A total of 402 consecutive patients who were hospitalized for AHFS were divided into 2 groups according to the use of intravenous nicorandil: 78 patients in the Nicorandil group and 324 patients in the Control group. During the 180-day follow-up, death or rehospitalization for heart failure occurred in 7 patients in the Nicorandil group (9.0%) and in 75 patients (23.2%) in the Control group. Event-free survival rates were significantly higher in the Nicorandil group than in the Control group (P=0.006). Multivariate Cox hazard analysis revealed that age (hazard ratio (HR)=1.066, P<0.0001), systolic blood pressure (HR=0.983, P=0.0023), New York Heart Association class III/IV (HR=6.550, P<0.0001), log creatinine (HR=3.866, P=0.0106), and use of intravenous nicorandil (HR=0.179, P<0.0001) were significant predictive factors for the occurrence of death or rehospitalization for heart failure. -

Genetic Factors Influencing B-Type Natriuretic Peptide-Mediated Production of Cyclic Guanosine Monophosphate and Blood Pressure Effects in Heart Failure Patients
Henry Ford Health System Henry Ford Health System Scholarly Commons Cardiology Articles Cardiology/Cardiovascular Research 12-1-2015 Genetic Factors Influencing B-type Natriuretic Peptide-Mediated Production of Cyclic Guanosine Monophosphate and Blood Pressure Effects in Heart Failure Patients David E. Lanfear Henry Ford Health System, [email protected] Jia Li Henry Ford Health System, [email protected] Raza Abbas Ruicong She Henry Ford Health System, [email protected] Badri Padhukasahasram See next page for additional authors Follow this and additional works at: https://scholarlycommons.henryford.com/cardiology_articles Recommended Citation Lanfear DE, Li J, Abbas R, She R, Padhukasahasram B, Gupta RC, Langholz D, Tang WH, Williams LK, Sabbah HN, Chow SL. Genetic factors influencing b-type natriuretic peptide-mediated production of cyclic guanosine monophosphate and blood pressure effects in heart failure patients. J Cardiovasc Transl Res. 2015 ;8(9):545-53. This Article is brought to you for free and open access by the Cardiology/Cardiovascular Research at Henry Ford Health System Scholarly Commons. It has been accepted for inclusion in Cardiology Articles by an authorized administrator of Henry Ford Health System Scholarly Commons. Authors David E. Lanfear, Jia Li, Raza Abbas, Ruicong She, Badri Padhukasahasram, Ramesh C. Gupta, David Langholz, W HW Tang, Keoki L. Williams, Hani N. Sabbah, and Sheryl L. Chow This article is available at Henry Ford Health System Scholarly Commons: https://scholarlycommons.henryford.com/ cardiology_articles/409 J. of Cardiovasc. Trans. Res. (2015) 8:545–553 DOI 10.1007/s12265-015-9660-2 Genetic Factors Influencing B-type Natriuretic Peptide-Mediated Production of Cyclic Guanosine Monophosphate and Blood Pressure Effects in Heart Failure Patients David E. -

Customs Tariff - Schedule
CUSTOMS TARIFF - SCHEDULE 99 - i Chapter 99 SPECIAL CLASSIFICATION PROVISIONS - COMMERCIAL Notes. 1. The provisions of this Chapter are not subject to the rule of specificity in General Interpretative Rule 3 (a). 2. Goods which may be classified under the provisions of Chapter 99, if also eligible for classification under the provisions of Chapter 98, shall be classified in Chapter 98. 3. Goods may be classified under a tariff item in this Chapter and be entitled to the Most-Favoured-Nation Tariff or a preferential tariff rate of customs duty under this Chapter that applies to those goods according to the tariff treatment applicable to their country of origin only after classification under a tariff item in Chapters 1 to 97 has been determined and the conditions of any Chapter 99 provision and any applicable regulations or orders in relation thereto have been met. 4. The words and expressions used in this Chapter have the same meaning as in Chapters 1 to 97. Issued January 1, 2019 99 - 1 CUSTOMS TARIFF - SCHEDULE Tariff Unit of MFN Applicable SS Description of Goods Item Meas. Tariff Preferential Tariffs 9901.00.00 Articles and materials for use in the manufacture or repair of the Free CCCT, LDCT, GPT, UST, following to be employed in commercial fishing or the commercial MT, MUST, CIAT, CT, harvesting of marine plants: CRT, IT, NT, SLT, PT, COLT, JT, PAT, HNT, Artificial bait; KRT, CEUT, UAT, CPTPT: Free Carapace measures; Cordage, fishing lines (including marlines), rope and twine, of a circumference not exceeding 38 mm; Devices for keeping nets open; Fish hooks; Fishing nets and netting; Jiggers; Line floats; Lobster traps; Lures; Marker buoys of any material excluding wood; Net floats; Scallop drag nets; Spat collectors and collector holders; Swivels. -

NIH Public Access Author Manuscript Curr Emerg Hosp Med Rep
NIH Public Access Author Manuscript Curr Emerg Hosp Med Rep. Author manuscript; available in PMC 2015 June 01. NIH-PA Author ManuscriptPublished NIH-PA Author Manuscript in final edited NIH-PA Author Manuscript form as: Curr Emerg Hosp Med Rep. 2014 June ; 2(2): 126–132. doi:10.1007/s40138-014-0040-z. Vasodilators in Acute Heart Failure: Review of the Latest Studies Phillip D. Levy, Said Laribi, and Alexandre Mebazaa Associate Professor of Emergency Medicine, Assistant Director of Clinical Research, Cardiovascular Research Institute, Associate Director of Clinical Research, Department of Emergency, Medicine, Wayne State University School of Medicine, 4201 St. Antoine; UHC – 6G, Detroit, MI 48201 Abstract Vasodilators play an important role in the management of acute heart failure, particularly when increased afterload is the precipitating cause of decompensation. The time-honored approach to afterload reduction has been largely focused on use of intravenous nitrovasodilators and, when properly dosed, this class of agents does provide substantial symptom relief for patients with acute hypertensive heart failure. Despite this, nitrovasodilators have never been shown to diminish mortality or provide any post-discharge outcome benefit leading to an on-going search for viable and more effective alternatives. While no new vasodilators have been approved for use in acute heart failure since nesiritide more than a decade ago, a number of novel agents have been developed, with some showing significant promise in recent clinical trials. In this review, we summarize the latest study data as it relates to vasodilator therapy and provide a glimpse into the not too distant future state of acute heart failure care. -

Appendix B – New Zealand and United Kingdom: Legislation
APPENDIX B – NEW ZEALAND AND UNITED KINGDOM: LEGISLATION AND POLICY (Appendices N.Z. - 35 to U.K. -41) SCOPE OF PRACTICE FOR REGISTERED NURSES IN THE EXTENDED CLASS (NURSE PRACTITIONERS): A JURISDICTIONAL REVIEW - NOVEMBER 2007 TABLE OF CONTENTS Page NZ – 35 Nursing Council of New Zealand: Scope of Practice………….. 3 NZ – 36 Nurse Council of New Zealand: Nurse Practitioner Endorsement – Guidelines for Applicants …………….………… 9 NZ – 37 Extract from New Zealand Gazette, 10/11/2005, No. 188 p. 4750: Medicines (Designated Prescriber: Nurse Preactitioners) Notice 2005 .…………………….………………………………….. 34 NZ – 38 Regulations of New Zealand: Medicines (Designated Prescriber: Nurse Practitioners) Regulation 2005 - Schedule Substances That are Nurse Practitioner Medicines if They are Prescription Medicines ………………………….……...…………. 35 UK – 39 Nursing and Midwifery Council: Advanced Nursing Practice Update 19, June 2007……………………………………..………. 71 UK – 40 Nursing and Midwifery Council: Nurse Prescribing and the Supply and Administration of Medication Position Statement..…………………………………………………….……. 73 UK – 41 Nursing and Midwifery Council: Guidelines for the Administraion of Medicine Nurse , January 2004…………………………………………………………..……... 82 2 ABC000002002 Scopes of Practice Page 1 of 6 Appendix N.Z.- 35 Nurs(n9 Counci,t of New ZeaLand Scopes of practice :_;, On 18th September 2004 the current registers were replaced by four scopes of practice under the Health Practitioners ._...... Competence Assurance Act 2003. There has been a smooth .... transition for nurses to the new scopes of practice. Every nurse who was on the register or roll was transferred onto the new _ register with the appropriate scope and conditions on 18 September. These are outlined in the table below. The four scopes of practice are" registered nurse, nurse ._... -

Reasanz; INN Serelaxin
22 May 2014 EMA/303748/2014 Committee for Medicinal Products for Human Use (CHMP) Assessment report Reasanz International non-proprietary name: serelaxin Procedure No. EMEA/H/C/002817 Note Assessment report as adopted by the CHMP with all information of a commercially confidential nature deleted. 30 Churchill Place ● Canary Wharf ● London E14 5EU ● United Kingdom Telephone +44 (0)20 3660 6000 Facsimile +44 (0)20 3660 5520 Send a question via our website www.ema.europa.eu/contact An agency of the European Union Product information Name of the medicinal product: Reasanz Applicant: Novartis Europharm Ltd Wimblehurst Road Horsham West Sussex RH12 5AB UNITED KINGDOM Active substance: serelaxin International Nonproprietary Name/Common serelaxin Name: Pharmaco-therapeutic group (ATC Code): C01DX21 Therapeutic indication (as applied for) : Reasanz is indicated for the treatment of acute heart failure and to reduce mortality in patients with acute heart failure. Pharmaceutical form: Concentrate for solution for infusion Strengths: 1 mg/ml Route of administration: Intravenous use Packaging: vial (glass) Package size: 1 vial Assessment report EMA/303748/2014 Page 2/112 Table of contents 1. Background information on the procedure ............................................ 10 1.1. Submission of the dossier .................................................................................... 10 1.2. Steps taken for the assessment of the product ....................................................... 11 Steps taken for the re-examination procedure -

(12) Patent Application Publication (10) Pub. No.: US 2009/0215844 A1 Davis Et Al
US 20090215844A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2009/0215844 A1 Davis et al. (43) Pub. Date: Aug. 27, 2009 (54) COMPOSITIONS COMPRISING NEBVOLOL (60) Provisional application No. 60/577,423, filed on Jun. 4, 2004. (75) Inventors: Eric Davis, Morgantown, WV (US); John O'Donnell, Morgantown, WV (US); Peter Publication Classification Bottini, Morgantown, WV (US) (51) Int. Cl. A63L/353 (2006.01) Correspondence Address: A6II 3/40 (2006.01) FROST BROWN TODD, LLC A6II 3/4I (2006.01) 2200 PNCCENTER, 201 E. FIFTH STREET CINCINNATI, OH 45202 (US) (52) U.S. Cl. .......... 514/381: 514/456; 514/412: 514/423 (73) Assignee: Mylan Laboratories, Inc., Morgantown, WV (US) (57) ABSTRACT (21) Appl. No.: 12/366,866 Nebivolol has been shown to be beneficial in the treatment of cardiovascular diseases such hypertension, congestive heart (22) Filed: Feb. 6, 2009 failure, arterial stiffness and endothelial dysfunction. The present invention features a pharmaceutical composition Related U.S. Application Data comprising nebivolol and at least one other active agent, (62) Division of application No. 1 1/141,235, filed on May wherein the at least one other active agent is a cardiovascular 31, 2005. agent. Patent Application Publication Aug. 27, 2009 Sheet 1 of 4 US 2009/0215844 A1 Figure 1 50 Black Nebivolol (1.0 M) 500 white + tiebivoloi (1.0 (i)} s Black, Untreated S Swhite, untreated . 9 400 S 350. g 300 5 250 O 200 2. Untreated 1.0 Ramipriat Treatment (um) 'p < 0.05 and tip- 0.01 vs preincubation with nei olo alone (n =6) Patent Application Publication Aug. -

CUSTOMS TARIFF - SCHEDULE 99 - I
CUSTOMS TARIFF - SCHEDULE 99 - i Chapter 99 SPECIAL CLASSIFICATION PROVISIONS - COMMERCIAL Notes. 1. The provisions of this Chapter are not subject to the rule of specificity in General Interpretative Rule 3 (a). 2. Goods which may be classified under the provisions of Chapter 99, if also eligible for classification under the provisions of Chapter 98, shall be classified in Chapter 98. 3. Goods may be classified under a tariff item in this Chapter and be entitled to the Most-Favoured-Nation Tariff or a preferential tariff rate of customs duty under this Chapter that applies to those goods according to the tariff treatment applicable to their country of origin only after classification under a tariff item in Chapters 1 to 97 has been determined and the conditions of any Chapter 99 provision and any applicable regulations or orders in relation thereto have been met. 4. The words and expressions used in this Chapter have the same meaning as in Chapters 1 to 97. Issued January 1, 2016 99 - 1 CUSTOMS TARIFF - SCHEDULE Tariff Unit of MFN Applicable SS Description of Goods Item Meas. Tariff Preferential Tariffs 9901.00.00 Articles and materials for use in the manufacture or repair of the Free CCCT, LDCT, GPT, UST, following to be employed in commercial fishing or the commercial MT, MUST, CIAT, CT, harvesting of marine plants: CRT, IT, NT, SLT, PT, COLT, JT, PAT, HNT, Artificial bait; KRT: Free Carapace measures; Cordage, fishing lines (including marlines), rope and twine, of a circumference not exceeding 38 mm; Devices for keeping nets open; Fish hooks; Fishing nets and netting; Jiggers; Line floats; Lobster traps; Lures; Marker buoys of any material excluding wood; Net floats; Scallop drag nets; Spat collectors and collector holders; Swivels. -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data.