Development of Rationally Designed Live Attenuated Vaccines for Lassa Fever and Venezuelan Equine Encephalitis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nigeria Hit by Unprecedented Lassa Fever Outbreak Leslie Roberts
NEWS At Olorgesailie in Kenya, big hand axes (left) gave way INFECTIOUS DISEASE to smaller, more precise blades and points (right). more extreme. More than 80% of mammal Nigeria hit by unprecedented species had vanished and new kinds of el- ephants, pigs, foxes, and springboks gathered at tree-lined streams. MSA tools—relatively Lassa fever outbreak sophisticated blades and points that would have been hafted onto spears—were plentiful. As efforts to contain it mount, researchers are racing to find The site yielded no human fossils in this out what is driving this year’s surge in cases and deaths key time frame, so researchers can’t be sure who the new toolmakers were. But discover- ies elsewhere offer a strong hint. For years By Leslie Roberts Already, Nigeria’s fragile health care sys- archaeologists had thought the MSA tools tem is overwhelmed. The one dedicated were too old to have been made by our spe- y early January, it was clear some- Lassa fever ward in the country at Irrua cies. Then, last year, fossils resembling H. sa- thing “really, really extraordinary” Specialist Teaching Hospital in Edo state piens were found near MSA tools and dated was going on in Nigeria, says Lorenzo has just 24 beds. Without access to proper to nearly 300,000 years ago at Jebel Irhoud Pomarico of the Alliance for Interna- training and personal protective equip- in Morocco (Science, 9 June 2017, p. 993)— tional Medical Action (ALIMA). Cases ment, health care workers continue to timing that fits the Olorgesailie chronology. of Lassa fever, a rare viral hemor- become infected—by now 16 cases have Features of the MSA tools also suggest they Brhagic disease, were skyrocketing across the been reported, with one additional death. -

August 2019 Vol 25, No 8, August 2019
® August 2019 Pregnancy and Maternal Health Pregnancy Vol 25, No 8, August 2019 EMERGING INFECTIOUS DISEASES Pages 1445–1624 DEPARTMENT OF HEALTH & HUMAN SERVICES MEDIA MAIL Public Health Service POSTAGE & FEES PAID Centers for Disease Control and Prevention (CDC) Mailstop D61, Atlanta, GA 30329-4027 PHS/CDC Official Business Permit No. G 284 Penalty for Private Use $300 Return Service Requested Gift of George N. and Helen M. Richard, 1964. Image © The Metropolitan Museum of Art. Image source: Art Resource, NY Resource, Art source: Image Art. of Museum Metropolitan The © Image 1964. Richard, M. Helen and N. George of Gift . Oil on canvas; 28 1/2 in x 35 7/8 in/72.4 cm x 91.1 cm. cm. 91.1 x cm in/72.4 7/8 35 x in 1/2 28 canvas; on Oil . (1890) First Steps, after Millet after Steps, First Vincent van Gogh (1853–1890). (1853–1890). Gogh van Vincent ISSN 1080-6040 Peer-Reviewed Journal Tracking and Analyzing Disease Trends Pages 1445–1624 EDITOR-IN-CHIEF D. Peter Drotman ASSOCIATE EDITORS EDITORIAL BOARD Paul M. Arguin, Atlanta, Georgia, USA Barry J. Beaty, Fort Collins, Colorado, USA Charles Ben Beard, Fort Collins, Colorado, USA Martin J. Blaser, New York, New York, USA Ermias Belay, Atlanta, Georgia, USA Christopher Braden, Atlanta, Georgia, USA David M. Bell, Atlanta, Georgia, USA Arturo Casadevall, New York, New York, USA Sharon Bloom, Atlanta, Georgia, USA Kenneth G. Castro, Atlanta, Georgia, USA Richard Bradbury, Atlanta, Georgia, USA Vincent Deubel, Shanghai, China Mary Brandt, Atlanta, Georgia, USA Christian Drosten, Charité Berlin, Germany Corrie Brown, Athens, Georgia, USA Isaac Chun-Hai Fung, Statesboro, Georgia, USA Charles H. -

Insights Into the Nigerian COVID19 Outbreak Authors
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 9 July 2020 doi:10.20944/preprints202007.0181.v1 Title: Insights into the Nigerian COVID19 outbreak Authors: Chinedu Ugwu A *1, 5, Adewole Adekola *2, Opeoluwa Adewale-Fasoro *3, Oyebola Oyesola *4 Jonathan L. Heeney5, Christian Happi 1, ⁋ Abstract : Given the pace of SARS-CoV-2 transmission and its relatively high mortality rate, COVID-19, has the potential to become the most severe pandemic in recent times. This virus’s spread across international borders has triggered different responses in countries around the globe with a spectrum of mild, moderate to severe outcomes. Nigeria, Africa’s most populous country with many densely populated cities, presents a unique situation for the explosive spread of SARS- CoV-2. However, at the point of this writing, the number of reported confirmed infection and mortality is comparatively lower to other countries with dense urban populations. The exact reasons for this are not clear but include societal, political and infrastructural factors that will influence the course of the outbreak in Nigeria. In this perspective, we have described the ongoing COVID-19 outbreak and its associated peculiarities. We identify critical steps that remain to be taken to contain and control the outbreak in Nigeria. Keywords: Nigeria, disease drivers, public health, COVID19 Affiliations: 1 Africa Centre of Excellence for Genomics of Infectious Disease, Redeemers’ University Ede, Osun State Nigeria 2 Royal Veterinary College, University of London, United Kingdom 3 Johns Hopkins Bloomberg School of Public Health, Baltimore, USA 4 Cornell University, Ithaca, NY 14850, United States and University of Washington, Seattle, WA, 98106, United States 5. -

West Africa Genomics Research
West Africa Ge nomics Research (WAGER) Network Characterizing Fevers of Unknown Origin (FUO) Through Microbial Metagenomics PI: Christian Happi Co-PI: Onikepe Folarin WAGER 2013 WAGER Network Redeemer’s University, Nigeria AFRICAN UNIVERSITY PARTNERS Redeemer’s University, Nigeria INTERNATIONAL Irrua Specialist Teaching Hospital, RESEARCH/TRAINING Nigeria Technology PARTNERS The Broad Institute of Harvard Universite Cheik Anta Diop, Transfer/Tr and MIT, Boston, USA Senegal aining/Sup port University of Sierra Leone, Sierra Harvard University, USA Leone WAGER 2013 Tulane University, USA OVERALL AIM Employ the power of new technologies and analytic methods for the benefit of patients and community caretakers. WAGER 2013 Objectives • Develop a rapid, field deployable, low cost and flexible diagnostic system for: – FUO causing diseases – Known drug resistance markers for malaria – Novel pathogens detected through high throughput metagenomic sequencing. • Develop Capacity in West African Institutions WAGER 2013 Develop Capacity in Genomics in West African Institutions – Transfer of technology in the area of genomics – Train personnel in area of genomics – Support and promote cutting edge genomics research on health in West Africa WAGER 2013 Introduction and Significance • High prevalence of infectious diseases in developing countries • All infectious pathogenic disease have common symptoms • Diagnosis possible only by culturing or targeted molecular approaches • This is challenging and problematic especially in developing countries WAGER 2013 • Better tool such as Microbial Metagenomics is therefore required for pathogen discovery in fever of unknown origin (FUO). – Is the unbiased characterisation of microbial nucleic acids. – does not require culturing. – No cloning. – a priori knowledge of the infecting microbes. WAGER 2013 • Better tool such as Microbial Metagenomics is therefore required for pathogen discovery in fever of unknown origin (FUO). -

Retrospective Cohort Study of Lassa Fever in Pregnancy, Southern Nigeria Sylvanus Okogbenin, Joseph Okoeguale, George Akpede, Andres Colubri, Kayla G
RESEARCH Retrospective Cohort Study of Lassa Fever in Pregnancy, Southern Nigeria Sylvanus Okogbenin, Joseph Okoeguale, George Akpede, Andres Colubri, Kayla G. Barnes, Samar Mehta, Reuben Eifediyi, Felix Okogbo, Joseph Eigbefoh, Mojeed Momoh, Mojeed Rafiu, Donatus Adomeh, Ikponmwosa Odia, Chris Aire, Rebecca Atafo, Martha Okonofua, Meike Pahlman, Beate Becker-Ziaja, Danny Asogun, Peter Okokhere, Christian Happi, Stephan Günther, Pardis C. Sabeti, Ephraim Ogbaini-Emovon In support of improving patient care, this activity has been planned and implemented by Medscape, LLC and Emerging Infectious Diseases. Medscape, LLC is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team. Medscape, LLC designates this Journal-based CME activity for a maximum of 1.00 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity. Successful completion of this CME activity, which includes participation in the evaluation component, enables the participant to earn up to 1.0 MOC points in the American Board of Internal Medicine's (ABIM) Maintenance of Certification (MOC) program. Participants will earn MOC points equivalent to the amount of CME credits claimed for the activity. It is the CME activity provider's responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit. All other clinicians completing this activity will be issued a certificate of participation. To participate in this journal CME activity: (1) review the learning objectives and author disclosures; (2) study the education content; (3) take the post-test with a 75% minimum passing score and complete the evaluation at http://www.medscape.org/journal/eid; and (4) view/print certificate. -

Curriculum Vitae of Onikepe Abiola Folarin A
CURRICULUM VITAE OF ONIKEPE ABIOLA FOLARIN A. PERSONAL DATA: 1. Name: FOLARIN Onikepe Abiola 2. Date of Birth: 25th September, 1973 3. Marital Status: Married 4. Postal Address: Department of Biological Sciences, College of Natural Sciences, Redeemer’s University. P.M.B. 203, Ede, Osun State, Nigeria 5. Email Address: [email protected] 6. Mobile phone numbers: (234) 803 565 9134 7. No. of children and their ages: Two (2) children (Fifteen and Eleven years) 8. Name and address of Spouse: Mr. Olalekan Adebisi Folarin, No. 6 Joseph Adediran Way off Basorun Road, Ibadan, Oyo State 9. Name and address of Next of Kin: Mr. Olalekan Adebisi Folarin No. 6 Joseph Adediran Way off Basorun Road, Ibadan, Oyo State 10. Nationality: Nigerian 11. State of Origin: Oyo State B. EDUCATIONAL BACKGROUND: 1. Higher Educational Institutions attended with dates: o University of Ibadan, Ibadan 2000 – 2006 o University of Ibadan, Ibadan 1998 – 1999 o University of Ibadan, Ibadan 1991 – 1997 1 2. Academic and Professional Qualifications: Academic Qualification o Ph.D. (Biochemistry/Molecular Biology) 2006 o M. Sc. (Biochemistry) 1999 o B.Sc. (Biochemistry) 1997 Professional Qualification o Advanced Molecular Biology Training Course 2007 o Molecular Biology and Genomics training course 2014 o MiSeq Next Generation Sequencing Training 2015 o Advanced Genomics Training Course 2015 o MalariaX: Defeating Malaria from the Genes to the Globe 2017 3. Other Distinctions and Awards: o WHO/TDR award for Malaria Molecular Biology Training 2002 Workshop/course, Kampala, Uganda o Nigeria Federal Government Postgraduate Scholarship 2002 o MIM Travel Award for the 4th MIM Pan-African Conference on 2005 Malaria o UNCTAD Fellowship for Advanced Molecular Biology Training 2007 Course in Cape Town, South Africa o Boroughs Wellcome and Bill and Melinda Gates Awards, Genome 2010 Epidemiology Meeting (GEM), Wellcome Trust Conference Centre, Hinxton, UK. -
Nigeria's Largest Lassa Fever Outbreak Sparked by Rats
10/18/2018 Nigeria’s largest Lassa fever outbreak sparked by rats NEWS · 17 OCTOBER 2018 Nigeria’s largest Lassa fever outbreak sparked by rats Analysis calms fears that the virus had mutated into a super-bug that could move more easily from person to person. Amy Maxmen A health worker arrives at the Institute of Lassa Fever Research and Control in Nigeria with blood samples for testing. Credit: Pius Utomi Ekpei/AFP/Getty Get the most important science stories of the day, free in your inbox. Sign up for Nature Briefing https://www.nature.com/articles/d41586-018-07024-6 1/4 10/18/2018 Nigeria’s largest Lassa fever outbreak sparked by rats Rats fuelled the largest outbreak of deadly Lassa fever in Nigeria this year, according to the most extensive and rapid genomic analysis of the Lassa virus conducted thus far. The study1, published on 17 October in the New England Journal of Medicine, eases fears that Lassa had mutated into a super-bug that was spreading swiftly between people. Instead, the viral genomes harvested from 220 patients were surprisingly diverse, indicating that most people had not acquired their infections from someone else. The unprecedented speed of this analysis has helped officials to combat the spread of Lassa fever, and the virus’s genetic information will assist researchers as they develop vaccines against the illness. About 514 people fell ill with the disease between January through the end of September, and 134 of them have died. “Getting whole genome sequences from this number of samples quickly, and at a site of an outbreak, is exciting and important,” says Peter Daszak, the president of EcoHealth Alliance, an organization based in New York City focused on emerging diseases. -

Fy Sept Edition Kk Original FINAL-1 Ver 15 PRINT Sm.Cdr
WRaPMarching towards a HIV/AIDS free- futureUp Walter In this issue Reed s Moving up with research studies 2 s DHIS in NMOD-USDOD Program 3 s Commmon Malaria 4 Program s JWARG in Nigeria 6 s Infectious diseases 10 Nigeria s And much more... NewsletterofUSDepartmentofDefenseWalterReedProgram-Nigeria Vol. 5, End of FY 16 Edition 2016 Newsletter of U.S. Department of Defense Walter Reed Program-Nigeria (DoD WRP-N) FOREWORD s the fiscal year comes to a bioresponse capability to challenges presented today. Aclose, the military to detect, provide surveillance The enduring military to military partnership reflects on a n d r e s p o n d t o f u t u r e military partnership between the past 12 months to look at infectious disease outbreaks Walter Reed and the Health our successes, challenges and that affect the military and the Implementation Programme way forward. communities in which they has a bright future and is poised serve. to continue to succeed in their The Walter Reed Program- ongoing and future missions, Nigeia (WRP-N) saw significant In missions all around the some of which are summarized growth in program activities country and sub-region, the in this newsletter. and added a new component, Nigerian military medical corps spearheaded by headquarters continues to respond to the call Thank you for your continued leadership, known as the Joint of duty, while the government support of our partnership. West African Research Group manages a significantly - Robbie Nelson (JWARG). In addtion to JWARG, reduced budget due to the Country Director the partnership is initiating a devaluation of the Naira, WRP-N second Ebola vaccine trial, and resulting from lower prices and a malaria slide bank protocol to production of crude oil. -
Next-Generation Sequencing Aids Researchers in the Fight Against
May 2015 Next-Generation Sequencing Aids Researchers in the Fight Against the Ebola Virus Genomic studies with the HiSeq® and MiSeq® Systems are enabling researchers to track Ebola outbreaks and understand the impact of the virus’s rapid mutation rate. Introduction Excellence for Genomics of infectious Diseases (ACEGID), Redeemer’s University, Ede, Osun State, Nigeria, have spent much of the last year The 2014 Ebola outbreak sickened and killed thousands of people using the HiSeq System to understand how this virus spreads and in West Africa, struck major urban centers and sent countries into changes over time. chaos, and caused an international and humanitarian crisis. But first, the virus infected a child. Through careful history taking, researchers In the Center of the Storm identified a two-year old boy as the first case in what would become the largest Ebola outbreak to date. He lived in a small village in Guinea, The pair first met at a conference in Senegal on computational not far from the border of Sierra Leone and Liberia. In late December genomics, where they began looking for signals in the human genome 2013, he became sick with fever, vomiting, and signs of hemorrhage. that might confer malaria resistance. Their work, however, revealed The boy died after several days, followed closely by several other a signal that Lassa fever, another hemorrhagic virus endemic to family members. This strain of the virus is believed to have jumped West Africa, was placing a strong evolutionary pressure on humans. to humans from an infected fruit bat, its natural wildlife reservoir.1 Within a month, they put together an Institutional Review Board (IRB) Since the outbreak began nearly 18 months ago, the World Health application and had a field site set up in Nigeria. -

The Origins and Future of Sentinel: an Early-Warning System for Pandemic Preemption and Response
viruses Article The Origins and Future of Sentinel: An Early-Warning System for Pandemic Preemption and Response Yolanda Botti-Lodovico 1,†, Parvathy Nair 2,†, Dolo Nosamiefan 3,†, Matthew Stremlau 4,†, Stephen Schaffner 1,5,6,† , Sebastian V. Agignoae 1,7, John Oke Aiyepada 8, Fehintola V. Ajogbasile 3,9, George O. Akpede 8,10, Foday Alhasan 11, Kristian G. Andersen 12,13, Danny A. Asogun 14, Oladele Oluwafemi Ayodeji 15, Aida S. Badiane 16, Kayla Barnes 1,6, Matthew R. Bauer 17, Antoinette Bell-Kareem 18, Muoebonam Ekene Benard 8, Ebo Ohomoime Benevolence 8, Osiemi Blessing 8, Chloe K. Boehm 1,19, Matthew L. Boisen 20, Nell G. Bond 18, Luis M. Branco 20, Michael J. Butts 1,5, Amber Carter 1, Andres Colubri 1,21, Awa B. Deme 16, Katherine C. DeRuff 1, Younousse Diédhiou 16, Akhilomen Patience Edamhande 8, Siham Elhamoumi 1, Emily J. Engel 18, Philomena Eromon 3, Mosoka Fallah 22, Onikepe A. Folarin 3,9, Ben Fry 23, Robert Garry 18 , Amy Gaye 16, Michael Gbakie 11, Sahr M. Gevao 24, Gabrielle Gionet 1, Adrianne Gladden-Young 1, Augustine Goba 25, Jules Francois Gomis 16, Anise N. Happi 3, Mary Houghton 1, Chikwe Ihekwuazu 8, Christopher Ojemiega Iruolagbe 26, Jonathan Jackson 27, Simbirie Jalloh 25, Jeremy Johnson 1, Lansana Kanneh 11, Adeyemi Kayode 3,9, Molly Kemball 1,5, Ojide Chiedozie Kingsley 28, Veronica Koroma 11, Dylan Kotliar 1,5, Samar Mehta 29, Hayden C. Metsky 1, Airende Michael 8, Marzieh Ezzaty Mirhashemi 1, Kayvon Modjarrad 30, Mambu Momoh 25,31, Cameron A. Myhrvold 1,19 , Okonofua Grace Naregose 8, Tolla Ndiaye 16, Mouhamadou Ndiaye 16, Aliou Ndiaye 16, Erica Normandin 1,32, Ikponmwosa Odia 8, Judith Uche Oguzie 3,9, Sylvanus A. -

Mathematical Modelling of Some Diseases Related to Water
Escola Internacional de Doutoramento Fa¨ı¸calNda¨ırou TESE DE DOUTORAMENTO Modelado matem´atico de certas enfermidades relacionadas coa auga Mathematical modelling of some diseases related to water Dirixida polos doutores: Iv´anCarlos Area Carracedo (Universidade de Vigo) e Delfim Fernando Marado Torres (Universidade de Aveiro, Portugal) Ano: 2020 Escola Internacional de Doutoramento Iv´anCarlos Area Carracedo e Delfim Fernando Marado Torres FAN CONSTAR que o presente traballo titulado “Modelado matem´atico de certas enfermidades relacionadas coa auga” “Mathematical modelling of some diseases related to water”, que presenta Fa¨ı¸calNda¨ırou para a obtenci´ondo t´ıtulo de Doutor/a, foi elaborado baixo a s´ua direcci´onno pro- grama de doutoramento Programa de Doutoramento en Auga, Sustentabilidade e Desenvolvemento (O03D040P06). Ourense, 17 de setembro de 2020. Os Directores da tese de doutoramento Dr. Iv´anCarlos Area Carracedo Dr. Delfim Fernando Marado Torres Summary This thesis dissertation focusses on the study of some infectious diseases dynamics from a double point of view: modelization and control. Our main aim is to formulate new mathematical models and combining them with existing ones in order to analyze the dynamics of diseases related to water. We consider compartmental models described by ordinary di↵erential equations and perform rigorous qualitative and quantitative techniques for acquiring insights into the dynamics of these models. My contribution to the material in this thesis is contained in the following original papers: P1) F. Nda¨ırou, I. Area and D. F. M. Torres. Mathematical Modeling of Japanese Encephalitis Under Aquatic Environmental E↵ects.Submitted; P2) F. Nda¨ırou, I. -
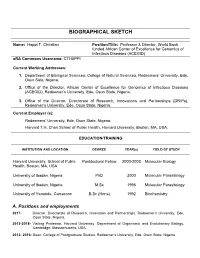
Biographical Sketch
BIOGRAPHICAL SKETCH Name: Happi T. Christian Position/Title: Professor & Director, World Bank funded African Center of Excellence for Genomics of Infectious Diseases (ACEGID) eRA Commons Username: CTHAPPI Current Working Addresses: 1. Department of Biological Sciences, College of Natural Sciences, Redeemers’ University, Ede, Osun Sate, Nigeria. 2. Office of the Director, African Center of Excellence for Genomics of Infectious Diseases (ACEGID), Redeemer’s University, Ede, Osun State, Nigeria. 3. Office of the Director, Directorate of Research, Innovations and Partnerships (DRIPs), Redeemer’s University, Ede, Osun State, Nigeria. Current Employer (s): Redeemers’ University, Ede, Osun State, Nigeria. Harvard T.H. Chan School of Public Health, Harvard University, Boston, MA, USA. EDUCATION/TRAINING INSTITUTION AND LOCATION DEGREE YEAR(s) FIELD OF STUDY Harvard University, School of Public Postdoctoral Fellow 2000-2003 Molecular Biology Health, Boston, MA, USA University of Ibadan, Nigeria PhD 2000 Molecular Parasitology University of Ibadan, Nigeria M.Sc 1995 Molecular Parasitology University of Yaounde, Cameroon B.Sc (Hons) 1992 Biochemistry A. Positions and employments 2017- Director, Directorate of Research, Innovation and Partnerships, Redeemer’s University, Ede, Osun State, Nigeria. 2013-2018- Visiting Professor, Harvard University, Department of Organismic and Evolutionary Biology, Cambridge, Massachusetts, USA. 2012- 2016: Dean, College of Postgraduate Studies, Redeemer’s University, Ede, Osun State, Nigeria. 2012- Present: Senior Associate Member, The Broad Institute of Harvard and MIT, Cambridge, Massachusetts, USA. 2011- Present: Professor of Molecular Biology and Genomics, Department of Biological Sciences, College of Natural Sciences, Redeemers’ University, Ede, Osun State, Nigeria. 2011-Present: Fellow, Exxon-Mobil Corp, USA, Malaria Leadership Programme, Harvard Malaria Initiative, Harvard University, Boston, MA, USA.