ENDOMETRIAL CYCLE Dr
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chapter V FOLLICULAR DYNAMICS and REPRODUCTIVE
Chapter V FOLLICULAR DYNAMICS AND REPRODUCTIVE TECHNOLOGIES IN BUFFALO Giuseppina Maria Terzano Istituto Sperimentale per la Zootecnia (Animal Production Research Institute) Via Salaria 31, 00016 Monterotondo (Rome), Italy The general characteristics of reproduction like seasonality, cyclicity and ovulation differ widely in mammals for the following reasons: a) reproductive activity may take place during the whole year or at defined seasons, according to the species and their adaptation to environmental conditions; thus, photoperiod plays a determinant role in seasonal breeders such as rodents, carnivores and ruminants (sheep, goats, buffaloes, deer, etc.,). An extreme situation is observed in foxes with only one ovulation per year, occurring in January or February; b) mammals may be distinguished according to the absence or presence of spontaneous ovulations: in the first group of mammals ( rabbits, hares, cats, mink, camels, Llama), the ovulation is induced by mating and cyclicity is not obvious; in the second group, ovulation occurs spontaneously in each cycle, separating the follicular phase from the luteal phase; c) the length of cycles is quite different among species: small rodents have short cycles of four or five days, farm animals and primates have longer cycles (sheep: 17 days; cow, goat, buffalo, horse and pig: 21 days; primates: 28 days), and dogs are characterized by long cycles of six to seven months, including a two month luteal phase (Concannon, 1993); d) ovulation rates differ widely among species and breeds within a given species: in sheep for example, Merinos d'Arles or Ile-de-France breeds have only one ovulation per cycle, whereas average rates of two to four ovulations per cycle are observed in prolific breeds like Romanov or Finn (Land et al., 1973). -

Chapter 24 Primary Sex Organs = Gonads Produce Gametes Secrete Hormones That Control Reproduction Secondary Sex Organs = Accessory Structures
Anatomy Lecture Notes Chapter 24 primary sex organs = gonads produce gametes secrete hormones that control reproduction secondary sex organs = accessory structures Development and Differentiation A. gonads develop from mesoderm starting at week 5 gonadal ridges medial to kidneys germ cells migrate to gonadal ridges from yolk sac at week 7, if an XY embryo secretes SRY protein, the gonadal ridges begin developing into testes with seminiferous tubules the testes secrete androgens, which cause the mesonephric ducts to develop the testes secrete a hormone that causes the paramesonephric ducts to regress by week 8, in any fetus (XX or XY), if SRY protein has not been produced, the gondal ridges begin to develop into ovaries with ovarian follicles the lack of androgens causes the paramesonephric ducts to develop and the mesonephric ducts to regress B. accessory organs develop from embryonic duct systems mesonephric ducts / Wolffian ducts eventually become male accessory organs: epididymis, ductus deferens, ejaculatory duct paramesonephric ducts / Mullerian ducts eventually become female accessory organs: oviducts, uterus, superior vagina C. external genitalia are indeterminate until week 8 male female genital tubercle penis (glans, corpora cavernosa, clitoris (glans, corpora corpus spongiosum) cavernosa), vestibular bulb) urethral folds fuse to form penile urethra labia minora labioscrotal swellings fuse to form scrotum labia majora urogenital sinus urinary bladder, urethra, prostate, urinary bladder, urethra, seminal vesicles, bulbourethral inferior vagina, vestibular glands glands Strong/Fall 2008 Anatomy Lecture Notes Chapter 24 Male A. gonads = testes (singular = testis) located in scrotum 1. outer coverings a. tunica vaginalis =double layer of serous membrane that partially surrounds each testis; (figure 24.29) b. -
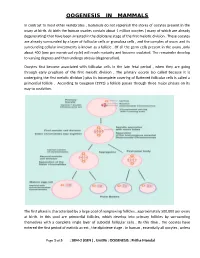
Oogenesis in Mammals
OOGENESIS IN MAMMALS In contrast to most other vertebrates , mammals do not replenish the stores of oocytes present in the ovary at birth. At birth the human ovaries contain about 1 million oocytes ( many of which are already degenerating) that have been arrested in the diplotene stage of the first meiotic division . These oocytes are already surrounded by a layer of follicular cells or granulosa cells , and the complex of ovum and its surrounding cellular investments is known as a follicle . Of all the germ cells present in the ovary ,only about 400 (one per menstrual cycle) will reach maturity and become ovulated. The remainder develop to varying degrees and then undergo atresia (degeneration). Oocytes first become associated with follicular cells in the late fetal period , when they are going through early prophase of the first meiotic division . The primary oocyte (so called because it is undergoing the first meiotic division ) plus its incomplete covering of flattened follicular cells is called a primordial follicle . According to Gougeon (1993) a follicle passes through three major phases on its way to ovulation. The first phase is characterized by a large pool of nongrowing follicles , approximately 500,000 per ovary at birth. In this pool are primordial follicles, which develop into primary follicles by surrounding themselves with a complete single layer of cuboidal follicular cells . By this time , the oocytes have entered the first period of meiotic arrest , the diplotene stage . In human , essentially all oocytes , unless Page 1 of 5 : SEM-2 (GEN ) , Unit#6 : OOGENESIS : Pritha Mondal they degenerate ,remain arrested in the diplotene stage until puberty ; some will not progress past the diplotene stage until the woman’s last reproductive cycle (age 45 to 55 years). -

FEMALE REPRODUCTIVE SYSTEM Female Reproduc�Ve System
Human Anatomy Unit 3 FEMALE REPRODUCTIVE SYSTEM Female Reproducve System • Gonads = ovaries – almond shaped – flank the uterus on either side – aached to the uterus and body wall by ligaments • Gametes = oocytes – released from the ovary during ovulaon – Develop within ovarian follicles Ligaments • Broad ligament – Aaches to walls and floor of pelvic cavity – Connuous with parietal peritoneum • Round ligament – Perpendicular to broad ligament • Ovarian ligament – Lateral surface of uterus ‐ ‐> medial surface of ovary • Suspensory ligament – Lateral surface of ovary ‐ ‐> pelvic wall Ovarian Follicles • Layers of epithelial cells surrounding ova • Primordial follicle – most immature of follicles • Primary follicle – single layer of follicular (granulosa) cells • Secondary – more than one layer and growing cavies • Graafian – Fluid filled antrum – ovum supported by many layers of follicular cells – Ovum surrounded by corona radiata Ovarian Follicles Corpus Luteum • Ovulaon releases the oocyte with the corona radiata • Leaves behind the rest of the Graafian follicle • Follicle becomes corpus luteum • Connues to secrete hormones to support possible pregnancy unl placenta becomes secretory or no implantaon • Becomes corpus albicans when no longer funconal Corpus Luteum and Corpus Albicans Uterine (Fallopian) Tubes • Ciliated tubes – Passage of the ovum to the uterus and – Passage of sperm toward the ovum • Fimbriae – finger like projecons that cover the ovary and sway, drawing the ovum inside aer ovulaon The Uterus • Muscular, hollow organ – supports -

Ovarian Cancer Stroma: Pathophysiology and the Roles in Cancer Development
Cancers 2012, 4, 701-724; doi:10.3390/cancers4030701 OPEN ACCESS cancers ISSN 2072-6694 www.mdpi.com/journal/cancers Review Ovarian Cancer Stroma: Pathophysiology and the Roles in Cancer Development Mitsuko Furuya Department of Pathology, Yokohama City University Graduate School of Medicine, Yokohama 236-0004, Japan; E-Mail: [email protected]; Tel.: +81-45-787-2587; Fax: +81-45-786-0191 Received: 17 May 2012; in revised form: 29 June 2012 / Accepted: 12 July 2012 / Published: 18 July 2012 Abstract: Ovarian cancer represents one of the cancers with the worst prognostic in adult women. More than half of the patients who present with clinical signs such as abdominal bloating and a feeling of fullness already show advanced stages. The majority of ovarian cancers grow as cystic masses, and cancer cells easily spread into the pelvic cavity once the cysts rupture or leak. When the ovarian cancer cells disseminate into the peritoneal cavity, metastatic nests may grow in the cul-de-sac, and in more advanced stages, the peritoneal surfaces of the upper abdomen become the next largest soil for cancer progression. Ascites is also produced frequently in ovarian cancers, which facilitates distant metastasis. Clinicopathologic, epidemiologic and molecular studies on ovarian cancers have improved our understanding and therapeutic approaches, but still further efforts are required to reduce the risks in the patients who are predisposed to this lethal disease and the mortality of the patients in advanced stages. Among various molecules involved in ovarian carcinogenesis, special genes such as TP53, BRCA1 and BRCA2 have been well investigated. These genes are widely accepted as the predisposing factors that trigger malignant transformation of the epithelial cells of the ovary. -

Biology of the Corpus Luteum
PERIODICUM BIOLOGORUM UDC 57:61 VOL. 113, No 1, 43–49, 2011 CODEN PDBIAD ISSN 0031-5362 Review Biology of the Corpus luteum Abstract JELENA TOMAC \UR\ICA CEKINOVI] Corpus luteum (CL) is a small, transient endocrine gland formed fol- JURICA ARAPOVI] lowing ovulation from the secretory cells of the ovarian follicles. The main function of CL is the production of progesterone, a hormone which regu- Department of Histology and Embryology lates various reproductive functions. Progesterone plays a key role in the reg- Medical Faculty, University of Rijeka B. Branchetta 20, Rijeka, Croatia ulation of the length of estrous cycle and in the implantation of the blastocysts. Preovulatory surge of luteinizing hormone (LH) is crucial for Correspondence: the luteinization of follicular cells and CL maintenance, but there are also Jelena Tomac other factors which support the CL development and its functioning. In the Department of Histology and Embryology Medical Faculty, University of Rijeka absence of pregnancy, CL will cease to produce progesterone and induce it- B. Branchetta 20, Rijeka, Croatia self degradation known as luteolysis. This review is designed to provide a E-mail: [email protected] short overview of the events during the life span of corpus luteum (CL) and to make an insight in the synthesis and secretion of its main product – pro- Key words: Ovary, Corpus Luteum, gesterone. The major biologic mechanisms involved in CL development, Progesterone, Luteinization, Luteolysis function, and regression will also be discussed. INTRODUCTION orpus luteum (CL) is a transient endocrine gland, established by Cresidual follicular wall cells (granulosa and theca cells) following ovulation. -

Vocabulario De Morfoloxía, Anatomía E Citoloxía Veterinaria
Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) Servizo de Normalización Lingüística Universidade de Santiago de Compostela COLECCIÓN VOCABULARIOS TEMÁTICOS N.º 4 SERVIZO DE NORMALIZACIÓN LINGÜÍSTICA Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) 2008 UNIVERSIDADE DE SANTIAGO DE COMPOSTELA VOCABULARIO de morfoloxía, anatomía e citoloxía veterinaria : (galego-español- inglés) / coordinador Xusto A. Rodríguez Río, Servizo de Normalización Lingüística ; autores Matilde Lombardero Fernández ... [et al.]. – Santiago de Compostela : Universidade de Santiago de Compostela, Servizo de Publicacións e Intercambio Científico, 2008. – 369 p. ; 21 cm. – (Vocabularios temáticos ; 4). - D.L. C 2458-2008. – ISBN 978-84-9887-018-3 1.Medicina �������������������������������������������������������������������������veterinaria-Diccionarios�������������������������������������������������. 2.Galego (Lingua)-Glosarios, vocabularios, etc. políglotas. I.Lombardero Fernández, Matilde. II.Rodríguez Rio, Xusto A. coord. III. Universidade de Santiago de Compostela. Servizo de Normalización Lingüística, coord. IV.Universidade de Santiago de Compostela. Servizo de Publicacións e Intercambio Científico, ed. V.Serie. 591.4(038)=699=60=20 Coordinador Xusto A. Rodríguez Río (Área de Terminoloxía. Servizo de Normalización Lingüística. Universidade de Santiago de Compostela) Autoras/res Matilde Lombardero Fernández (doutora en Veterinaria e profesora do Departamento de Anatomía e Produción Animal. -

Grade 5 the Journey of an Egg
Grade 5 The Journey of an Egg Learner Outcomes W-5.3 Identify the basic components of the human reproductive system, and describe the basic functions of the various components; e.g. fertilization, conception How To Use This lesson plan contains several activities to achieve the learner outcome above. You may choose to do some or all of the activities, based on the needs of your students and the time available. Some of the activities build on the ones that come before them, but all can be used alone. For a quick lesson, combine activities A, C, D and G. Classroom Activities & Timing A. Ground Rules (5-10 minutes) See also the B. Anatomy Vocabulary Matching Game (15-20 minutes) Differing Abilities C. Anatomy Diagrams (15-20 minutes) lesson plans on Puberty and D. The Egg’s Journey (20-30 minutes) Reproduction. E. Class Discussion (5-15 minutes) F. Eggs and Ovaries Kahoot! Quiz (15-20 minutes) G. Question Box (5-10 minutes) Required Materials POSTERS: Anatomy Definitions CARDS: Anatomy Vocabulary HANDOUT and ANSWER KEY: Reproductive System Diagrams HANDOUT: The Menstrual Cycle ©2020 2 Grade 5 The Journey of an Egg HANDOUT: The Egg’s Journey KAHOOT! QUIZ and ANSWER KEY: Eggs and Ovaries All the student handouts are also available in the Grade 5 Workbook. All the diagrams are also available as slides in Grade 5 Diagrams. Background Information for Teachers Inclusive Language Language is complex, evolving and powerful. In these lessons, inclusive language is used to be inclusive of all students, including those with diverse gender identities, gender expressions and sexual orientations. -

The Effectiveness and Safety of the Early Follicular Phase Full-Dose Down
The effectiveness and safety of the early follicular phase full-dose down- regulation protocol for controlled ovarian hyperstimulation: a randomized, paralleled controlled, multicenter trial 2018-12-29 Background Since the first “tube baby”, Louise Brown, was born in the United Kingdom in 1978, many infertile couples have been benefitted from in vitro fertilization and embryo transfer (IVF-ET) and intracytoplasmic sperm injection (ICSI). It is reported that there are over 5 million babies born with the help of assisted reproductive technology (ART). According to the 2015 national data published by Human Fertility and Embryology Authority (HFEA, 48,147 women received 61,726 IVF/ICSI cycles and gave birth to 17,041 newborns [1]. In the United States, 169,602 IVF/ICSI cycles were performed in 2014 and 68,791 tubal babies were born [2]. China has a huge population base, and therefore has a substantial number of infertile couples. Although a late starter, China is developing rapidly in ART and playing a more and more important role in the area of reproductive medicine. In spite of the continuous development in ART, so far, the overall success rate of IVF/ICSI is still hovering around 25-40%. The live birth rate per stimulated cycle is 25.6% in the UK in 2015, fluctuating from 1.9% in women aged 45 and elder to 32.2% in women younger than 35 years old [1]. The IVF/ICSI success rate in 2014 in the US is similar [2]. In China, according to the data submitted by 115 reproductive medicine centers on the ART data reporting system developed by Chinese Society of Reproductive Medicine, the delivery rate is about 40% [3]. -

Women's Menstrual Cycles
1 Women’s Menstrual Cycles About once each month during her reproductive years, a woman has a few days when a bloody fluid leaves her womb and passes through her vagina and out of her body. This normal monthly bleeding is called menstruation, or a menstrual period. Because the same pattern happens each month, it is called the menstrual cycle. Most women bleed every 28 days. But some bleed as often as every 20 days or as seldom as every 45 days. Uterus (womb) A woman’s ovaries release an egg once a month. If it is Ovary fertilized she may become pregnant. If not, her monthly bleeding will happen. Vagina Menstruation is a normal part of women’s lives. Knowing how the menstrual cycle affects the body and the ways menstruation changes over a woman’s lifetime can let you know when you are pregnant, and help you detect and prevent health problems. Also, many family planning methods work best when women and men know more about the menstrual cycle (see Family Planning). 17 December 2015 NEW WHERE THERE IS NO DOCTOR: ADVANCE CHAPTERS 2 CHAPTER 24: WOMEN’S MENSTRUAL CYCLES Hormones and the menstrual cycle In women, the hormones estrogen and progesterone are produced mostly in the ovaries, and the amount of each one changes throughout the monthly cycle. During the first half of the cycle, the ovaries make mostly estrogen, which causes the lining of the womb to thicken with blood and tissue. The body makes the lining so a baby would have a soft nest to grow in if the woman became pregnant that month. -

The Reproductive System
27 The Reproductive System PowerPoint® Lecture Presentations prepared by Steven Bassett Southeast Community College Lincoln, Nebraska © 2012 Pearson Education, Inc. Introduction • The reproductive system is designed to perpetuate the species • The male produces gametes called sperm cells • The female produces gametes called ova • The joining of a sperm cell and an ovum is fertilization • Fertilization results in the formation of a zygote © 2012 Pearson Education, Inc. Anatomy of the Male Reproductive System • Overview of the Male Reproductive System • Testis • Epididymis • Ductus deferens • Ejaculatory duct • Spongy urethra (penile urethra) • Seminal gland • Prostate gland • Bulbo-urethral gland © 2012 Pearson Education, Inc. Figure 27.1 The Male Reproductive System, Part I Pubic symphysis Ureter Urinary bladder Prostatic urethra Seminal gland Membranous urethra Rectum Corpus cavernosum Prostate gland Corpus spongiosum Spongy urethra Ejaculatory duct Ductus deferens Penis Bulbo-urethral gland Epididymis Anus Testis External urethral orifice Scrotum Sigmoid colon (cut) Rectum Internal urethral orifice Rectus abdominis Prostatic urethra Urinary bladder Prostate gland Pubic symphysis Bristle within ejaculatory duct Membranous urethra Penis Spongy urethra Spongy urethra within corpus spongiosum Bulbospongiosus muscle Corpus cavernosum Ductus deferens Epididymis Scrotum Testis © 2012 Pearson Education, Inc. Anatomy of the Male Reproductive System • The Testes • Testes hang inside a pouch called the scrotum, which is on the outside of the body -
Variability in the Length of Menstrual Cycles Within and Between Women - a Review of the Evidence Key Points
Variability in the Length of Menstrual Cycles Within and Between Women - A Review of the Evidence Key Points • Mean cycle length ranges from 27.3 to 30.1 days between ages 20 and 40 years, follicular phase length is 13-15 days, and luteal phase length is less variable and averages 13-14 days1-3 • Menstrual cycle lengths vary most widely just after menarche and just before menopause primarily as cycles are anovulatory 1 • Mean length of follicular phase declines with age3,11 while luteal phase remains constant to menopause8 • The variability in menstrual cycle length is attributable to follicular phase length1,11 Introduction Follicular and luteal phase lengths Menstrual cycles are the re-occurring physiological – variability of menstrual cycle changes that happen in women of reproductive age. Menstrual cycles are counted from the first day of attributable to follicular phase menstrual flow and last until the day before the next onset of menses. It is generally assumed that the menstrual cycle lasts for 28 days, and this assumption Key Points is typically applied when dating pregnancy. However, there is variability between and within women with regard to the length of the menstrual cycle throughout • Follicular phase length averages 1,11,12 life. A woman who experiences variations of less than 8 13-15 days days between her longest and shortest cycle is considered normal. Irregular cycles are generally • Luteal phase length averages defined as having 8 to 20 days variation in length of 13-14 days1-3 cycle, whereas over 21 days variation in total cycle length is considered very irregular.