FUNDAMENTALS of GEOMETRIC LAPAROSCOPY and SUTURING FUNDAMENTALS of GEOMETRIC LAPAROSCOPY and SUTURING of GEOMETRIC LAPAROSCOPY FUNDAMENTALS Resad P
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Chapter 1 History of Laparoscopic Surgery
Chapter 1 History of Laparoscopic Surgery Kiyokazu Nakajima, Jeffrey W. Milsom, and Bartholomäus Böhm Although laparoscopic surgery has transformed surgery only in the past two decades, its evolution is only the natural byproduct of the medical doctor’s curiosity to directly visualize and treat surgical dis- eases. The earliest known attempts to look inside the living human body date from 460 to 375 BC, from the Kos school of medicine led by Hippocrates in Greece.1,2 They described a rectal examination using a speculum remarkably similar to the instruments we use today. Similar specula were discovered in the ruins of Pompeii (70 AD) that were used to examine the vagina, the cervix, and the rectum, and obtain an inside view of the nose and ear.1 The Babylonian Talmud written in 500 AD described a lead siphon, named “Siphophert,” with a mouthpiece, which was bent inward and held a mechul (wooden drain).1,3 The apparatus was introduced into the vagina and was used to differentiate between vaginal and uterine bleeding. During these early years ambient light was used. The term “endoscopein” is attributed to Avicenna (Ibn Sina, 980–1037 AD) of Persia, although an Arabian physician, Albulassim (912–1013 AD), who placed a mirror in front of the exposed vagina, was the fi rst to use refl ected light as a source of illumination for an endoscopic examination. Giulio Caesare Aranzi in Venice (1530–1589) developed the fi rst endoscopic light in 1587. He used the Benedictine monk Don Panuce’s principle of the “camera obscura” for medical purposes – the -

Hybrid Procedure Offers a Less Invasive Alternative to Colectomy
The better way to get better Hybrid procedure offers a less invasive alternative to colectomy Insufflation gas provides important advantage The colonoscopy-laparoscopy procedure is made possible through the combined skills of the gastroenterologist and laparoscopic surgeon, and the use of CO2 rather than ambient air for insufflation — the introduction of gas into the colon to improve visibility. CO2 is more quickly absorbed by the gastrointestinal tract and results in less bowel distension, giving the laparoscopic surgeon a better field of vision within the abdominal cavity. © Copyright Olympus. Used with permission. “Some patients who would have required a bowel resection can instead benefit from this A new, minimally invasive procedure that is a hybrid of colonoscopy and less invasive procedure. We’re laparoscopy is proving to be a safe and effective alternative to open colectomy using this combined technique (removal of part of the colon) for patients with benign colon polyps that are as a way for patients to avoid colectomy,” explains James not removable endoscopically. Yoo, M.D., a colorectal surgeon Patients who undergo this hybrid procedure experience less pain and often go at UCLA. “This procedure home after only one or two days. Scarring and wound complications are minimal involves tiny incisions for the as the laparoscopic surgeon makes only small, keyhole incisions in the abdomen laparoscopic instruments and patients stay in the hospital only rather than the long incision characteristic of a traditional colectomy. a day or two.” WWW.UCLAHEALTH.ORG 1-800-UCLA-MD1 (1-800-825-2631) Who can benefit from the procedure? Participating When a routine colonoscopy reveals polyps, they are usually removed at the Physicians time of the procedure as a precaution against their progression to cancer. -

Laparoscopic Sentinel Node Mapping for Colorectal Cancer Using Infrared Ray Laparoscopy
ANTICANCER RESEARCH 26: 2307-2312 (2006) Laparoscopic Sentinel Node Mapping for Colorectal Cancer Using Infrared Ray Laparoscopy KOICHI NAGATA1, SHUNGO ENDO1, EIJI HIDAKA1, JUN-ICHI TANAKA1, SHIN-EI KUDO1 and AKIRA SHIOKAWA2 1Digestive Disease Center and 2Pathology Section, Showa University Northern Yokohama Hospital, Yokohama 224-8503, Japan Abstract. Background: Sentinel lymph node (SN) mapping colectomy (LAC). SNs were mapped by the submucosal by dye injection on conventional laparoscopy (CL) is often injection of dye on intra-operative colonoscopy, or by the precluded by the presence of mesenteric adipose tissue in use of a spinal needle and percutaneous subserosal injection patients with colorectal cancer. SN mapping on CL was of dye at a premarked site (pre-operative tattooing of compared with that on infrared ray laparoscopy (IRL) during polypectomy site with carbon). However, our experience laparoscopy-assisted colectomy (LAC). Patients and indicates that laparoscopic SN mapping by dye injection is Methods: Forty-eight patients with colorectal cancer who technically difficult because injection of the dye into the underwent LAC were enrolled. The tumor was identified by colon wall during LAC is cumbersome. Submucosal intra-operative fluoroscopy with marking clips. The tumor injection of dye on intra-operative colonoscopy makes LAC was stained intra-operatively by peritumoral injection of difficult and problematic. Distension of the small intestine indocyanine green dye. SNs were observed by CL and by IRL. with air on colonoscopy interferes with the operative field Results: In all 48 patients, dye injection and tumor and precludes laparoscopic procedures. Moreover, intra- localization during LAC were successful. The identification operative colonoscopic examinations require considerable of SNs on IRL was approximately five times better than that time, especially in patients with right-sided colon cancer. -
Operative Laparoscopy
Operative Laparoscopy Technique Procedure involves the placement of a laparoscope (special telescope with a video camera attached) into the abdomen at the belly button. The pelvis including the uterus, fallopian tubes, ovaries, bladder and appendix are all visualized to determine the source of the patient's problem. The treatment necessary is determined based upon what the surgeon sees during this exam. Potential treatments include ovarian cyst removal, ovarian removal, excision or destruction of endometriosis, and removal of scar tissue. Incisions 3-4 small incisions (less than one inch) are made on the abdomen for this procedure. Operative Time Operative times vary greatly depending on the findings at the time of surgery. Your surgeon will proceed with safety as his/her first priority. Average times range from 45-90 minutes. Anesthesia General anesthesia Preoperative Care Nothing by mouth after midnight The procedure is usually scheduled immediately after your menstrual period. Hospital Stay Day surgery or 23 hour observation Postoperative Care These guidelines are intended to give you a general idea of your postoperative course. Since every patient is unique and has a unique procedure, your recovery may differ. You will be prescribed both an anti-inflammatory and a narcotic pain medicine for postoperative use. We recommend that anti-inflammatory medications, such as ibuprofen, naproxen, etc., be used on a scheduled (regular) basis and that narcotic pain medicine be utilized on an "as needed" basis. Driving is allowed after your procedure only when you do not require the narcotic pain medicine to manage your pain. Patients may return to work in 2-3 days following the procedure. -

Procedure Coding in ICD-9-CM and ICD- 10-PCS
Procedure Coding in ICD-9-CM and ICD- 10-PCS ICD-9-CM Volume 3 Procedures are classified in volume 3 of ICD-9-CM, and this section includes both an Alphabetic Index and a Tabular List. This volume follows the same format, organization and conventions as the classification of diseases in volumes 1 and 2. ICD-10-PCS ICD-10-PCS will replace volume 3 of ICD-9-CM. Unlike ICD-10-CM for diagnoses, which is similar in structure and format as the ICD-9-CM volumes 1 and 2, ICD-10-PCS is a completely different system. ICD-10-PCS has a multiaxial seven-character alphanumeric code structure providing unique codes for procedures. The table below gives a brief side-by-side comparison of ICD-9-CM and ICD-10-PCS. ICD-9-CM Volume3 ICD-10-PCS Follows ICD structure (designed for diagnosis Designed and developed to meet healthcare coding) needs for a procedure code system Codes available as a fixed or finite set in list form Codes constructed from flexible code components (values) using tables Codes are numeric Codes are alphanumeric Codes are 3-4 digits long All codes are seven characters long ICD-9-CM and ICD-10-PCS are used to code only hospital inpatient procedures. Hospital outpatient departments, other ambulatory facilities, and physician practices are required to use CPT and HCPCS to report procedures. ICD-9-CM Conventions in Volume 3 Code Also In volume 3, the phrase “code also” is a reminder to code additional procedures only when they have actually been performed. -

The Costs and Benefits of Moving to the ICD-10 Code Sets
CHILDREN AND ADOLESCENTS This PDF document was made available from www.rand.org as a public CIVIL JUSTICE service of the RAND Corporation. EDUCATION ENERGY AND ENVIRONMENT Jump down to document HEALTH AND HEALTH CARE 6 INTERNATIONAL AFFAIRS POPULATION AND AGING The RAND Corporation is a nonprofit research PUBLIC SAFETY SCIENCE AND TECHNOLOGY organization providing objective analysis and effective SUBSTANCE ABUSE solutions that address the challenges facing the public TERRORISM AND HOMELAND SECURITY and private sectors around the world. TRANSPORTATION AND INFRASTRUCTURE U.S. NATIONAL SECURITY Support RAND Purchase this document Browse Books & Publications Make a charitable contribution For More Information Visit RAND at www.rand.org Explore RAND Science and Technology View document details Limited Electronic Distribution Rights This document and trademark(s) contained herein are protected by law as indicated in a notice appearing later in this work. This electronic representation of RAND intellectual property is provided for non-commercial use only. Permission is required from RAND to reproduce, or reuse in another form, any of our research documents for commercial use. This product is part of the RAND Corporation technical report series. Reports may include research findings on a specific topic that is limited in scope; present discus- sions of the methodology employed in research; provide literature reviews, survey instruments, modeling exercises, guidelines for practitioners and research profes- sionals, and supporting documentation; -

Minimally Invasive Single-Site Surgery for the Digestive System: a Technological Review
8/10/2018 Minimally invasive single-site surgery for the digestive system: A technological review J Minim Access Surg. 2011 Jan-Mar; 7(1): 40–51. PMCID: PMC3002006 doi: 10.4103/0972-9941.72381 PMID: 21197242 Minimally invasive single-site surgery for the digestive system: A technological review Parag W Dhumane, Michele Diana, Joel Leroy, and Jacques Marescaux IRCAD/EITS, Hôpitaux Universitaires, 1 Place de l’Hôpital, 67091 Strasbourg Cedex, France Address for correspondence: Dr. Joel Leroy, IRCAD/EITS, Hôpitaux Universitaires, 1 Place de l’Hôpital, 67091 Strasbourg Cedex, France. E-mail: [email protected] Received 2010 Jul 19; Accepted 2010 Aug 2. Copyright © Journal of Minimal Access Surgery This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Abstract Go to: Minimally Invasive Single Site (MISS) surgery is a better terminology to explain the novel concept of scarless surgery, which is increasingly making its way into clinical practice. But, there are some difficulties. We review the existing technologies for MISS surgery with regards to single-port devices, endoscope and camera, instruments, retractors and also the future perspectives for the evolution of MISS surgery. While we need to move ahead cautiously and wait for the development of appropriate technology, we believe that the “Ultimate form of Minimally Invasive Surgery” will be a hybrid form of MISS surgery and Natural Orifice Transluminal Endoscopic Surgery, complimented by technological innovations from the fields of robotics and computer-assisted surgery. -

Endoscopy Matrix
Endoscopy Matrix CPT Description of Endoscopy Diagnostic Therapeutic Code (Surgical) 31231 Nasal endoscopy, diagnostic, unilateral or bilateral (separate procedure) X 31233 Nasal/sinus endoscopy, diagnostic with maxillary sinusoscopy (via X inferior meatus or canine fossa puncture) 31235 Nasal/sinus endoscopy, diagnostic with sphenoid sinusoscopy (via X puncture of sphenoidal face or cannulation of ostium) 31237 Nasal/sinus endoscopy, surgical; with biopsy, polypectomy or X debridement (separate procedure) 31238 Nasal/sinus endoscopy, surgical; with control of hemorrhage X 31239 Nasal/sinus endoscopy, surgical; with dacryocystorhinostomy X 31240 Nasal/sinus endoscopy, surgical; with concha bullosa resection X 31241 Nasal/sinus endoscopy, surgical; with ligation of sphenopalatine artery X 31253 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including frontal sinus exploration, with removal of tissue from frontal sinus, when performed 31254 Nasal/sinus endoscopy, surgical; with ethmoidectomy, partial (anterior) X 31255 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior 31256 Nasal/sinus endoscopy, surgical; with maxillary antrostomy X 31257 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including sphenoidotomy 31259 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including sphenoidotomy, with removal of tissue from the sphenoid sinus 31267 Nasal/sinus endoscopy, surgical; with removal of -

Laparoscopic Surgery for Endometriosis
Laparoscopic surgery for endometriosis Introduction This leaflet covers laparoscopic surgery for endometriosis. It provides information for women who have been offered or are considering laparoscopic surgery for the treatment of endometriosis. Medical terms have been highlighted in italics. Diagnosis of endometriosis Endometriosis is best diagnosed and assessed by actually looking at the disease. This is the only means of making a definite diagnosis. Laparoscopy is an operation in which a small telescope (laparoscope) is inserted into the abdomen to look directly at the tissues. A laparoscopy is carried out under general anaesthetic. At the same time various procedures can be performed in order to destroy or remove the endometriosis, endometriotic cysts and release scar tissue (adhesions). Is laparoscopy always needed to diagnose endometriosis? Laparoscopy is the best test to diagnose endometriosis. Endometriosis can sometimes be felt on vaginal examination or an endometriotic cyst seen on an ultrasound scan. A normal vaginal examination or a normal scan does not exclude endometriosis. A blood test measuring a protein, CA 125, may assist, however a raised level is not specific to endometriosis. It indicates irritation or inflammation inside the body and can be raised in endometriosis, as well as appendicitis, pelvic infection and ovarian cysts. A raised level does not mean a diagnosis of cancer. Laparoscopic surgery is only one type of surgical procedure for endometriosis. It does not, as is commonly thought, turn a major operation into a minor one. It has the advantage of smaller cuts on the tummy (abdomen) and slightly shorter recovery than a bikini line cut (laparotomy). Laparoscopic surgery may not be suitable for all patients. -

Laparoscopic Instruments
Laparoscopic Instruments Product Catalog Aesculap Laparoscopy 2 Table of Contents Introduction 4-5 Ligation 101-107 Advanced Energy 7-9 DS Clips 102-105 Caiman® Vessel Sealers 8-9 Challenger™ Ti-P 106-107 Monopolar Instruments 11-69 Access & Closure 109-123 Advanced Energy Single Use 12-15 Access Instruments 110 Reposable 16-17 Insufflation 111 Reusable 18-73 Rigid Trocars 112-113 3.5 mm mini 20-23 3.5 mm 113 Scissors 24-29 5 mm 114 Dissecting Forceps 30-35 10 mm 115 Monopolar Instruments Grasping Forceps 36-57 12 mm 116 Biopsy Forceps 58-61 HASSON 117 Spare parts 3.5 mm, 5 mm & 10 mm 62-63 Accessories & Spare Parts 118 Assembly/Disassembly 64-66 Additional Instruments 119 Electrodes 68-69 Flexible Trocars 120-121 Bipolar Instruments Bipolar Instruments 70-74 7 mm & 13 mm 120 Single use 70-71 Accessories & Spare Parts 121 Reusable 72-74 Closure 122-123 Assembly/Disassembly 74 Instruments 123 Specialty Instruments 75-100 Endoscopes 125-127 Slide Lock Graspers 76 Specialty Instruments Endoscopes 126 Bulldog Clips 77 Light Cables 127 Video-Assisted Thorascopic Surgery (VATS) 78-89 Care & Storage 129-138 Advanced Urology 90-91 Services 139-143 Needle Holders & Suturing 92-93 Ligation Index 144-151 Retractors 94-95 Nathanson Retractors 96-97 Suction/Irrigation 98 Suction/Irrigation with Monopolar 99 Closure & Miscellaneous Instruments 100 Access Endoscopes Storage & Care 3 History Blending Old World Craftsmanship with Modern Technology Aesculap AG World Headquarters in Tuttlingen, Germany Our founding father: Aesculap Gottfried Jetter As the -

Handling of Instruments
Limbs & Things TM learning online Handling of Instruments Overview If you are new to suturing, you will need to learn to recognize each of the instruments you are going to use, understand their function and practise the basic techniques of using them. 1 Scalpel A scalpel is a razor-edged blade on a handle. There are two types of surgical scalpel: reusable and disposable. Reusable scalpels consist of a blade that is replaced after every use, attached to a stainless steel handle that can be sterilised and re-used multiple times. In a hospital setting, this type is more likely to be used in order to reduce waste and to allow doctors to work with a variety of blades and handle sizes. Disposable surgical scalpels are usually single-piece with a plastic handle. This is the type provided in our Hands-on Kit for practice. Although you will use the same scalpel multiple times for practice, in a clinical setting you would dispose of the entire scalpel after a single use. 1.1 Principles A scalpel is essential for incising the skin and for sharp dissection. Held flat, it can also be useful for carefully undermining the skin edge to relieve tension. A razor edged blade engages over a flange on the scalpel handle. Several sizes of scalpel handle are available and size 3 is appropriate for most purposes. Each handle can be fitted with disposable blades of different shapes. The scalpel can be held in one of two ways: - For making large incisions e.g. laparotomy, and subcutaneous fat dissection, hold the scalpel like a table knife, with your index finger guiding the blade. -
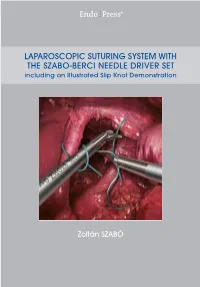
LAPAROSCOPIC SUTURING SYSTEM with the SZABO-BERCI NEEDLE DRIVER SET Including an Illustrated Slip Knot Demonstration
® LAPAROSCOPIC SUTURING SYSTEM WITH THE SZABO-BERCI NEEDLE DRIVER SET including an Illustrated Slip Knot Demonstration Zoltán SZABÓ LAPAROSCOPIC SUTURING SYSTEM WITH THE SZABO-BERCI NEEDLE DRIVER SET including an Illustrated Slip Knot Demonstration Zoltán SZABO, Ph.D., F.I.C.S San Francisco, California, U.S.A. 4 Laparoscopic Suturing System with the SZABO-BERCI Needle Driver Set Clinical cases: Laparoscopic Suturing System with the Barry N. Gardiner, M.D. SZABO-BERCI Needle Driver Set San Ramon, California, U.S.A. including an Illustrated Slip Knot Demonstration and Zoltán Szabó, Ph.D., F.I.C.S Steven A. Stanten, M.D. San Francisco, California, U.S.A Oakland, California, U.S.A. Correspondence address of the author: Zoltán Szabó, Ph.D., F.I.C.S., M.O.E.T. Institute Microsurgery & Operative Endoscopy Training Director: Zoltán Szabó 153, States Street San Francisco, CA 94114, U.S.A. Phone: 001 (415) 626-34 00 Fax: 001 (415) 626-34 44 E-mail: [email protected] All rights reserved. 1st edition 1993 © 2015 GmbH P.O. Box, 78503 Tuttlingen, Germany Important notes: Phone: +49 (0) 74 61/1 45 90 Medical knowledge is ever changing. As new research and clinical Fax: +49 (0) 74 61/708-529 experience broaden our knowledge, changes in treatment and therapy E-Mail: [email protected] may be required. The authors and editors of the material herein have consulted sources believed to be reliable in their efforts to provide No part of this publication may be translated, reprinted information that is complete and in accord with the standards or reproduced, transmitted in any form or by any means, accept ed at the time of publication.