Review Article
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Segmental Overvekst Og Vaskulærmalformasjoner V02
2/1/2021 Segmental overvekst og vaskulærmalformasjoner v02 Avdeling for medisinsk genetikk Segmental overvekst og vaskulærmalformasjoner Genpanel, versjon v02 * Enkelte genomiske regioner har lav eller ingen sekvensdekning ved eksomsekvensering. Dette skyldes at de har stor likhet med andre områder i genomet, slik at spesifikk gjenkjennelse av disse områdene og påvisning av varianter i disse områdene, blir vanskelig og upålitelig. Disse genetiske regionene har vi identifisert ved å benytte USCS segmental duplication hvor områder større enn 1 kb og ≥90% likhet med andre regioner i genomet, gjenkjennes (https://genome.ucsc.edu). Vi gjør oppmerksom på at ved identifiseringav ekson oppstrøms for startkodon kan eksonnummereringen endres uten at transkript ID endres. Avdelingens websider har en full oversikt over områder som er affisert av segmentale duplikasjoner. ** Transkriptets kodende ekson. Ekson Gen Gen affisert (HGNC (HGNC Transkript Ekson** Fenotype av symbol) ID) segdup* ACVRL1 175 NM_000020.3 2-10 Telangiectasia, hereditary hemorrhagic, type 2 OMIM ADAMTS3 219 NM_014243.3 1-22 Hennekam lymphangiectasia- lymphedema syndrome 3 OMIM AKT1 391 NM_005163.2 2-14 Cowden syndrome 6 OMIM Proteus syndrome, somatic OMIM AKT2 392 NM_001626.6 2-14 Diabetes mellitus, type II OMIM Hypoinsulinemic hypoglycemia with hemihypertrophy OMIM AKT3 393 NM_005465.7 2-14 Megalencephaly-polymicrogyria- polydactyly-hydrocephalus syndrome 2 OMIM file:///data/SegOv_v02-web.html 1/7 2/1/2021 Segmental overvekst og vaskulærmalformasjoner v02 Ekson Gen Gen affisert (HGNC (HGNC -

WES Gene Package Multiple Congenital Anomalie.Xlsx
Whole Exome Sequencing Gene package Multiple congenital anomalie, version 5, 1‐2‐2018 Technical information DNA was enriched using Agilent SureSelect Clinical Research Exome V2 capture and paired‐end sequenced on the Illumina platform (outsourced). The aim is to obtain 8.1 Giga base pairs per exome with a mapped fraction of 0.99. The average coverage of the exome is ~50x. Duplicate reads are excluded. Data are demultiplexed with bcl2fastq Conversion Software from Illumina. Reads are mapped to the genome using the BWA‐MEM algorithm (reference: http://bio‐bwa.sourceforge.net/). Variant detection is performed by the Genome Analysis Toolkit HaplotypeCaller (reference: http://www.broadinstitute.org/gatk/). The detected variants are filtered and annotated with Cartagenia software and classified with Alamut Visual. It is not excluded that pathogenic mutations are being missed using this technology. At this moment, there is not enough information about the sensitivity of this technique with respect to the detection of deletions and duplications of more than 5 nucleotides and of somatic mosaic mutations (all types of sequence changes). HGNC approved Phenotype description including OMIM phenotype ID(s) OMIM median depth % covered % covered % covered gene symbol gene ID >10x >20x >30x A4GALT [Blood group, P1Pk system, P(2) phenotype], 111400 607922 101 100 100 99 [Blood group, P1Pk system, p phenotype], 111400 NOR polyagglutination syndrome, 111400 AAAS Achalasia‐addisonianism‐alacrimia syndrome, 231550 605378 73 100 100 100 AAGAB Keratoderma, palmoplantar, -

Description of the Vanseq Subpanels Offered at Seattle Children’S Hospital
Description of the VANseq subpanels offered at Seattle Children’s Hospital Capillary Malformations (4 genes): EPHB4, GNA11, GNAQ, RASA1 Capillary malformation-arteriovenous malformation (CM-AVM) syndrome is associated with multiple small (1-2 cm diameter) capillary malformations and is due to loss of function mutations in EPHB4 or RASA1. Approximately 20% of individuals have AVMs, which can be life-threatening. Other features (telangiectasias, lymphedema, non- immune hydrops) have been associated. RASA1 and EPHB4 mutations are also associated with Parkes-Weber syndrome. Somatic activating mutations at codon 183 in the GNAQ gene cause isolated capillary malformations or Sturge Weber Syndrome. Somatic activating mutations at the same residue in GNA11 cause capillary malformation with overgrowth. LM/VM/AVM (17 genes) - Lymphatic Malformations, Venous Malformations, Arteriovenous Malformations: ACVRL1, ARAF, BRAF, ELMO2, ENG, EPHB4, GDF2, GLMN, HRAS, KRAS, MAP2K1, MAP3K3, NRAS, PIK3CA, PTEN, RASA1, TEK (TIE2) Most individuals with isolated lymphatic, venous, or arteriovenous malformations possess somatic, activating mutations in genes associated with cell growth and division. For many of these conditions, sequencing of affected, lesional tissue is required for mutation detection, and coordination with pathology is required. Although there are strong gene-phenotype correlations within this group, there is increasing recognition of phenotypic expansion and overlap. The most commonly mutated gene in this group of conditions is PIK3CA. • ~80% of isolated lymphatic malformations have pathogenic, tissue restricted variant in PIK3CA. • Most venous malformations have activating mutations in TEK (TIE2). TEK mutations can be isolated and somatic or multifocal, inherited in a dominant fashion. • Activating, somatic mutations in MAP2K1 are primarily associated with isolated extracranial AVMs. -

Parkes Weber Syndrome Associated with Two Somatic Pathogenic Variants in RASA1
Washington University School of Medicine Digital Commons@Becker Open Access Publications 8-1-2020 Parkes Weber syndrome associated with two somatic pathogenic variants in RASA1 Josue A. Flores Daboub Johanes F. Grimmer Alice Frigerio Whitney Wooderchak-Donahue Ryan Arnold See next page for additional authors Follow this and additional works at: https://digitalcommons.wustl.edu/open_access_pubs Authors Josue A. Flores Daboub, Johanes F. Grimmer, Alice Frigerio, Whitney Wooderchak-Donahue, Ryan Arnold, Jeff Szymanski, Nicola Longo, and Pinar Bayrak-Toydemir Downloaded from molecularcasestudies.cshlp.org on September 10, 2020 - Published by Cold Spring Harbor Laboratory Press COLD SPRING HARBOR Molecular Case Studies | RESEARCH REPORT Parkes Weber syndrome associated with two somatic pathogenic variants in RASA1 Josue A. Flores Daboub,1 Johanes Fred Grimmer,2 Alice Frigerio,3 Whitney Wooderchak-Donahue,4,5 Ryan Arnold,6 Jeff Szymanski,7 Nicola Longo,1,4 and Pinar Bayrak-Toydemir4,5 1Division of Pediatric Genetics, University of Utah School of Medicine, Salt Lake City, Utah 84108, USA; 2Division of Ear, Nose, and Throat, University of Utah, Salt Lake City, Utah 84108, USA; 3Division of Dermatology, University of Utah School of Medicine, Salt Lake City, Utah 84108, USA; 4Department of Pathology, 5ARUP Institute for Clinical and Experimental Pathology, University of Utah, Salt Lake City, Utah 84108, USA; 6Primary Children’s Hospital Interventional Radiology, Salt Lake City, Utah 84113, USA; 7Department of Radiation Oncology, Washington University, St. Louis, Missouri 63130, USA Abstract Parkes Weber syndrome is associated with autosomal dominant inheritance, caused by germline heterozygous inactivating changes in the RASA1 gene, characterized by multiple micro arteriovenous fistulas and segmental overgrowth of soft tissue and skel- etal components. -
El Paso Community College Syllabus Part II Official Course Description
DHYG 1239; Revised Fall 2016/Spring 2017 El Paso Community College Syllabus Part II Official Course Description SUBJECT AREA Dental Hygiene COURSE RUBIC AND NUMBER DHYG 1239 COURSE TITLE General and Oral Pathology COURSE CREDIT HOURS 2 2 : 1 Credits Lec Lab I. Catalog Description Offers a general study of disturbances in human body development, diseases of the body, and disease prevention measures with emphasis on the oral cavity and associated structures. A grade of "C" or better is required in this course to take the next course. Prerequisites: BIOL 2401 and BIOL 2402 and CHEM 1306 and 1106. Corequisites: DHYG 1103 and DHYG 1201 and DHYG 1219 and DHYG 1304 and DHYG 1431. (2:1). Lab fee. II. Course Objectives Upon satisfactory completion of the course, the student will be able to: A. Introduction to Preliminary Diagnosis of Oral Lesions 1. Define each of the terms in the vocabulary list for this chapter. 2. List and define the eight diagnostic categories that contribute to the diagnostic process. 3. Name a diagnostic category and give an example of a lesion, anomaly, or condition for which this category contributes greatly to the diagnosis. 4. Describe the clinical appearance of Fordyce=s granules (spots), torus palatinus, mandibular tori, and lingual varicosities, and identify them on a slide. 5. Describe the radiographic picture and historical data (including the age, sex, and race of the patient) that are relevant to periapical cementl dysplasia (cementoma). 6. Define Avariant of normal@ and give three examples of such lesions involving the tongue. 7. List and describe the clinical characteristics and identify a clinical picture of fissured tongue, median rhomboid glossitis, geographic tongue, ectopic geographic tongue, and hairy tongue. -

Genetic Insights Into Cerebrovascular Disorders: a Comprehensive Review
Genetic Insights into Cerebrovascular Disorders: a Comprehensive Review 1,2 3 4 5 Fawaz Al-Mufti, MD *, Ahmed Alkanaq, MD , Krishna Amuluru, MD , Rolla Nuoman, MD , 6 7 7 Ahmed Abdulrazzaq, DDS , Tamarah Sami, DDS , Halla Nuoaman, MD , Caroline Hayes- 5 2 8 Rosen, MD , Charles J. Prestigiacomo, MD , and Chirag D. Gandhi, MD 1 Rutgers University - Robert Wood Johnson Medical School, Department of Neurology, Division of Neuroendovascular Surgery and Neurocritical Care, New Brunswick, New Jersey, USA 2 Rutgers University - New Jersey Medical School, Department of Neurosurgery, Newark, New Jersey, USA 3 Rutgers University - Robert Wood Johnson Medical School, New Brunswick, New Jersey, USA Journal of Vascular and Interventional Neurology, Vol. 5 Vol. and Interventional Neurology, Journal of Vascular 4 University of Pittsburgh Medical Center- Hamot, Department of Neurointerventional Radiology, Erie, Pennsylvania, USA 5 Rutgers University - New Jersey Medical School, Department of Neurology, Division of Child Neurology, Newark, New Jersey, USA 6 Rutgers University - School of Dental Medicine, Newark, New Jersey, USA 7 Rutgers University - Robert Wood Johnson Medical School, Department of Neurology, New Brunswick, New Jersey, USA 8 Westchester Medical Center, New York Medical College, Department of Neurosurgery, Valhalla, New York, USA Keywords Cerebrovascular malformations; hereditary diseases Introduction Genetic vascular disorders are usually present at birth; The prevalence of intracranial vascular malformation structurally, they tend to grow proportionately with the has been shown to be increasing over time. This is child, and do not regress spontaneously. The malforma- believed to be due to the advancement in radiological tions vary greatly in number, size, and location, and can procedures. Many studies examining neurological syn- also occur in the context of syndromes. -

Understanding Chronic Venous Disease: a Critical Overview of Its Pathophysiology and Medical Management
Journal of Clinical Medicine Review Understanding Chronic Venous Disease: A Critical Overview of Its Pathophysiology and Medical Management Miguel A. Ortega 1,2,3,† , Oscar Fraile-Martínez 1,2,† , Cielo García-Montero 1,2,† , Miguel A. Álvarez-Mon 1,2,*, Chen Chaowen 1, Fernando Ruiz-Grande 4,5, Leonel Pekarek 1,2 , Jorge Monserrat 1,2 , Angel Asúnsolo 2,4,6 , Natalio García-Honduvilla 1,2,‡ , Melchor Álvarez-Mon 1,2,7,‡ and Julia Bujan 1,2,‡ 1 Department of Medicine and Medical Specialities, Faculty of Medicine and Health Sciences, University of Alcalá, 28801 Alcalá de Henares, Spain; [email protected] (M.A.O.); [email protected] (O.F.-M.); [email protected] (C.G.-M.); [email protected] (C.C.); [email protected] (L.P.); [email protected] (J.M.); [email protected] (N.G.-H.); [email protected] (M.Á.-M.); [email protected] (J.B.) 2 Ramón y Cajal Institute of Sanitary Research (IRYCIS), 28034 Madrid, Spain; [email protected] 3 Cancer Registry and Pathology Department, Hospital Universitario Principe de Asturias, 28806 Alcalá de Henares, Spain 4 Department of Surgery, Medical and Social Sciences, Faculty of Medicine and Health Sciences, University of Alcalá, 28801 Alcalá de Henares, Spain; [email protected] 5 Department of Vascular Surgery, Príncipe de Asturias Hospital, 28801 Alcalá de Henares, Spain 6 Department of Epidemiology and Biostatistics, Graduate School of Public Health and Health Policy, The City University of New York, New York, NY 10027, USA 7 Citation: Ortega, M.A.; Immune System Diseases—Rheumatology and Internal Medicine Service, University Hospital Príncipe de Fraile-Martínez, O.; García-Montero, Asturias, (CIBEREHD), 28806 Alcalá de Henares, Spain * Correspondence: [email protected] C.; Álvarez-Mon, M.A.; Chaowen, C.; † These authors contributed equality in this work. -

Blueprint Genetics Noonan Syndrome Panel
Noonan Syndrome Panel Test code: CA0501 Is a 35 gene panel that includes assessment of non-coding variants. Is ideal for patients with a clinical suspicion of a RASopathy including Noonan syndrome with or without lentigines, cardio- facio-cutaneous (CFC) syndrome, Costello syndrome, Noonan-like syndromes or other syndromes causing differential diagnostic challenges such as Legius syndrome, Baraitser-Winter syndromes and neurofibromatosis. About Noonan Syndrome Noonan syndrome is one of the most common syndromes with an estimated prevalence of 1 in 1,000 to 1 in 2,500 live births. It is clinically and genetically heterogeneous condition characterized by cardiovascular abnormalities, distinctive facial features, chest deformity, short stature, and other co-morbidities. Among the Noonan syndrome associated genes, many different genotype-phenotype correlations have been established although no phenotypic features are exclusively associated with one genotype. There are, however, significant differences in the risk of various Noonan syndrome manifestations based on the causative gene. Availability 4 weeks Gene Set Description Genes in the Noonan Syndrome Panel and their clinical significance Gene Associated phenotypes Inheritance ClinVar HGMD ACTB* Baraitser-Winter syndrome AD 55 60 ACTG1* Deafness, Baraitser-Winter syndrome AD 27 47 BRAF* LEOPARD syndrome, Noonan syndrome, Cardiofaciocutaneous syndrome AD 134 65 CBL Noonan syndrome-like disorder with or without juvenile myelomonocytic AD 24 43 leukemia CCNK Intellectual disability AD CDC42 -

Blueprint Genetics Pulmonary Artery Hypertension (PAH) Panel
Pulmonary Artery Hypertension (PAH) Panel Test code: CA0601 Is a 23 gene panel that includes assessment of non-coding variants. Is ideal for patients with a clinical diagnosis of idiopathic or familial pulmonary arterial hypertension. About Pulmonary Artery Hypertension (PAH) Pulmonary arterial hypertension (PAH) is characterized by widespread obstruction and obliteration of small pulmonary arteries leading to increased pulmonary vascular resistance, elevated pulmonary arterial pressure and eventually right ventricle failure and death. The clinical diagnosis of PAH can be established by the presence of mean pulmonary artery pressure >25 mmHg at rest or >30 mmHg during exercise when other known causes of pulmonary hypertension are excluded. Initial symptoms of pulmonary arterial hypertension are dyspnea (60%), fatigue (19%), syncope (8%), chest pain (7%), palpitation (5%), and edema (3%) and they correlate with the degree of RV failure. Mean age at diagnosis is 36 years but all age groups can be affected. There is no cure for PAH and current medications form, for some patients, only a bridge to lung transplantation. Availability 4 weeks Gene Set Description Genes in the Pulmonary Artery Hypertension (PAH) Panel and their clinical significance Gene Associated phenotypes Inheritance ClinVar HGMD ABCC8 Hyperinsulinemic hypoglycemia, Diabetes, permanent neonatal, AD/AR 170 641 Hypoglycemia, leucine-induced, Diabetes mellitus, transient neonatal, Pulmonary arterial hypertension (PAH) ACVRL1 Hereditary hemorrhagic telangiectasia AD 140 430 AQP1 -
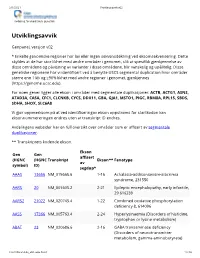
Utviklingsavvik V02
2/1/2021 Utviklingsavvik v02 Avdeling for medisinsk genetikk Utviklingsavvik Genpanel, versjon v02 * Enkelte genomiske regioner har lav eller ingen sekvensdekning ved eksomsekvensering. Dette skyldes at de har stor likhet med andre områder i genomet, slik at spesifikk gjenkjennelse av disse områdene og påvisning av varianter i disse områdene, blir vanskelig og upålitelig. Disse genetiske regionene har vi identifisert ved å benytte USCS segmental duplication hvor områder større enn 1 kb og ≥90% likhet med andre regioner i genomet, gjenkjennes (https://genome.ucsc.edu). For noen gener ligger alle ekson i områder med segmentale duplikasjoner: ACTB, ACTG1, ASNS, ATAD3A, CA5A, CFC1, CLCNKB, CYCS, DDX11, GBA, GJA1, MSTO1, PIGC, RBM8A, RPL15, SBDS, SDHA, SHOX, SLC6A8 Vi gjør oppmerksom på at ved identifiseringav ekson oppstrøms for startkodon kan eksonnummereringen endres uten at transkript ID endres. Avdelingens websider har en full oversikt over områder som er affisert av segmentale duplikasjoner. ** Transkriptets kodende ekson. Ekson Gen Gen affisert (HGNC (HGNC Transkript Ekson** Fenotype av symbol) ID) segdup* AAAS 13666 NM_015665.6 1-16 Achalasia-addisonianism-alacrimia syndrome, 231550 AARS 20 NM_001605.2 2-21 Epileptic encephalopathy, early infantile, 29 616339 AARS2 21022 NM_020745.4 1-22 Combined oxidative phosphorylation deficiency 8, 614096 AASS 17366 NM_005763.4 2-24 Hyperlysinaemia (Disorders of histidine, tryptophan or lysine metabolism) ABAT 23 NM_020686.6 2-16 GABA transaminase deficiency (Disorders of neurotransmitter metabolism, gamma-aminobutyrate) -

Inherited Vascular Disorder NGS Panel
Inherited Vascular Disorder Next Generation Sequencing (NGS) Rev 1.00 Panels: Information for Ordering Providers Background Inherited vascular disorders are a heterogenous group of conditions that affect blood vessel development and function. Many of these disorders increase an individual’s risk to develop vascular anomalies, which can be classified as either vascular tumours or vascular malformations. Vascular malformations can be further defined based on the type of blood vessel that is affected and the speed of blood flow: venous, capillary, and lymphatic malformations are slow-flow lesions whereas arteriovenous malformations and arteriovenous fistulas are high- flow lesions.1 The panels listed below include genes related to vascular malformations, pulmonary arterial hypertension, and/or cerebral small vessel disease. Associated clinical features or genetic conditions are listed for each gene and the inheritance pattern for each condition (AD – autosomal dominant, AR – autosomal recessive, XL – X- linked). Please be advised that order restrictions apply for the following panels. Carrier testing/presymptomatic testing is currently restricted to Clinical Genetics. Testing for symptomatic patients is restricted based on clinical specialty. Please refer to the APL Test Directory for specific ordering restrictions for each panel. Cerebral Cavernous Malformation Panel Cerebral cavernous malformations (CCMs) are comprised of enlarged capillaries in the brain and spinal cord that have abnormal shape and structure. The blood vessel walls are abnormally thin and lack intervening brain parenchyma. CCMs are typically identified between the second and fifth decades of life when individuals present with associated neurological symptoms including seizures, focal neurologic deficits, nonspecific headaches, and cerebral hemorrhage. Familial CCM should be suspected in an individual with multiple CCMs, or one CCM and at least one other family member with one or more CCMs. -

Genetics of Vascular Anomalies
Seminars in Pediatric Surgery 29 (2020) 150967 Contents lists available at ScienceDirect Seminars in Pediatric Surgery journal homepage: www.elsevier.com/locate/sempedsurg Genetics of vascular anomalies ∗ Ha-Long Nguyen a, Laurence M. Boon a,b, Miikka Vikkula a,b,c, a Human Molecular Genetics, de Duve Institute, University of Louvain, Brussels, Belgium b Center for Vascular Anomalies, Division of Plastic Surgery, VASCERN VASCA European Reference Centre, Saint Luc University Hospital, Brussels, Belgium c WELBIO (Walloon Excellence in Lifesciences and Biotechnology), de Duve Institute, University of Louvain, Brussels, Belgium a b s t r a c t Vascular anomalies are developmental defects of the vasculature and encompass a variety of disorders. The identification of genes mutated in the different malformations provides insight into the etiopathogenic mechanisms and the specific roles the associated proteins play in vascular development and maintenance. A few familial forms of vascular anomalies exist, but most cases occur sporadically. It is becoming evident that somatic mosaicism plays a major role in the formation of vascular lesions. The use of Next Generating Sequencing for high throughput and “deep” screening of both blood and lesional DNA and RNA has been instrumental in detecting such low frequency somatic changes. The number of novel causative mutations identified for many vascular anomalies has soared within a 10-year period. The discovery of such genes aided in unraveling a holistic overview of the pathogenic mechanisms, by which in vitro and in vivo models could be generated, and opening the doors to development of more effective treatments that do not address just symptoms. Moreover, as many mutations and the implicated signaling pathways are shared with cancers, current oncological therapies could potentially be repurposed for the treatment of vascular anomalies.