Comorbidities in Psoriasis: the Recognition of Psoriasis As a Systemic Disease and Current Management
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Syphilis Staging and Treatment Syphilis Is a Sexually Transmitted Disease (STD) Caused by the Treponema Pallidum Bacterium
Increasing Early Syphilis Cases in Illinois – Syphilis Staging and Treatment Syphilis is a sexually transmitted disease (STD) caused by the Treponema pallidum bacterium. Syphilis can be separated into four different stages: primary, secondary, early latent, and late latent. Ocular and neurologic involvement may occur during any stage of syphilis. During the incubation period (time from exposure to clinical onset) there are no signs or symptoms of syphilis, and the individual is not infectious. Incubation can last from 10 to 90 days with an average incubation period of 21 days. During this period, the serologic testing for syphilis will be non-reactive but known contacts to early syphilis (that have been exposed within the past 90 days) should be preventatively treated. Syphilis Stages Primary 710 (CDC DX Code) Patient is most infectious Chancre (sore) must be present. It is usually marked by the appearance of a single sore, but multiple sores are common. Chancre appears at the spot where syphilis entered the body and is usually firm, round, small, and painless. The chancre lasts three to six weeks and will heal without treatment. Without medical attention the infection progresses to the secondary stage. Secondary 720 Patient is infectious This stage typically begins with a skin rash and mucous membrane lesions. The rash may manifest as rough, red, or reddish brown spots on the palms of the hands, soles of the feet, and/or torso and extremities. The rash does usually does not cause itching. Rashes associated with secondary syphilis can appear as the chancre is healing or several weeks after the chancre has healed. -

Psoriasis, a Systemic Disease Beyond the Skin, As Evidenced by Psoriatic Arthritis and Many Comorbities
1 Psoriasis, a Systemic Disease Beyond the Skin, as Evidenced by Psoriatic Arthritis and Many Comorbities – Clinical Remission with a Leishmania Amastigotes Vaccine, a Serendipity Finding J.A. O’Daly Astralis Ltd, Irvington, NJ USA 1. Introduction Psoriasis is a systemic chronic, relapsing inflammatory skin disorder, with worldwide distribution, affects 1–3% of the world population, prevalence varies according to race, geographic location, and environmental factors (Chandran & Raychaudhuri, 2010; Christophers & Mrowietz, 2003; Farber & Nall, 1974). In Germany, 33,981 from 1,344,071 continuously insured persons in 2005 were diagnosed with psoriasis; thus the one year prevalence was 2.53% in the study group. Up to the age of 80 years the prevalence rate (range: 3.99-4.18%) was increasing with increasing age and highest for the age groups from 50 to 79 years The total rate of psoriasis in children younger than 18 years was 0.71%. The prevalence rates increased in an approximately linear manner from 0.12% at the age of 1 year to 1.2% at the age of 18 years (Schäfer et al., 2011). In France, a case-control study in 6,887 persons, 356 cases were identified (5.16%), who declared having had psoriasis during the previous 12 months (Wolkenstein et al., 2009). The prevalence of psoriasis analyzed across Italy showed that 2.9% of Italians declared suffering from psoriasis (regional range: 0.8-4.5%) in a total of 4109 individuals (Saraceno et al., 2008). The overall rate of comorbidity in subjects with psoriasis aged less than 20 years was twice as high as in subjects without psoriasis. -

Understanding Vasculitis Factsheet
Vasculitis - The Facts This factsheet is intended as a simple There is no cure for PSV, but it can usually be introduction to vasculitis for those who have just controlled by use of steroids, chemotherapy and been diagnosed with vasculitis, members of their immune suppressing drugs. Long term drug therapy is family, friends, work colleagues and for others often required. If all goes well some patients go into who may want to know about the disease. “full remission” - ie they no longer need drugs. But relapse is common. What is Vasculitis Vasculitis is a rare inflammatory disease which affects People suffering from vasculitis often experience about 2-3000 new people each year in the UK. muscle weakness and chronic fatigue. Some Vasculitis means inflammation of the blood vessels. experience chronic pain due to nerve damage or Any vessels in any part of the body can be affected. severe migraines and headaches due to damaged blood vessels in the head. There are several different types of vasculitis. In the first type, the acute form, it can be caused by Others require dialysis or kidney transplants. Many infections, reaction to drugs or exposure to chemicals. have breathing problems and others are left with Often the problem is localised, such as a rash. In these permanent physical disabilities. cases the disease usually needs no treatment. Other types of vasculitis can be secondary to (or as a The most “common” types of these rare consequence of) other illnesses such as rheumatoid vasculitis diseases are: arthritis or some types of cancer. ° Granulomatosis with Polyangiitis (GPA) (previously known as Wegener’s Granulomatosis) The third group is known as Primary Systemic ° Eosinophilic Granulomatosis with Polyangiitis (EGPA) Vasculitis (PSV). -

Celiac Disease and Nonceliac Gluten Sensitivitya Review
Clinical Review & Education JAMA | Review Celiac Disease and Nonceliac Gluten Sensitivity A Review Maureen M. Leonard, MD, MMSc; Anna Sapone, MD, PhD; Carlo Catassi, MD, MPH; Alessio Fasano, MD CME Quiz at IMPORTANCE The prevalence of gluten-related disorders is rising, and increasing numbers of jamanetwork.com/learning individuals are empirically trying a gluten-free diet for a variety of signs and symptoms. This review aims to present current evidence regarding screening, diagnosis, and treatment for celiac disease and nonceliac gluten sensitivity. OBSERVATIONS Celiac disease is a gluten-induced immune-mediated enteropathy characterized by a specific genetic genotype (HLA-DQ2 and HLA-DQ8 genes) and autoantibodies (antitissue transglutaminase and antiendomysial). Although the inflammatory process specifically targets the intestinal mucosa, patients may present with gastrointestinal signs or symptoms, extraintestinal signs or symptoms, or both, Author Affiliations: Center for Celiac suggesting that celiac disease is a systemic disease. Nonceliac gluten sensitivity Research and Treatment, Division of is diagnosed in individuals who do not have celiac disease or wheat allergy but who Pediatric Gastroenterology and Nutrition, MassGeneral Hospital for have intestinal symptoms, extraintestinal symptoms, or both, related to ingestion Children, Boston, Massachusetts of gluten-containing grains, with symptomatic improvement on their withdrawal. The (Leonard, Sapone, Catassi, Fasano); clinical variability and the lack of validated biomarkers for nonceliac gluten sensitivity make Celiac Research Program, Harvard establishing the prevalence, reaching a diagnosis, and further study of this condition Medical School, Boston, Massachusetts (Leonard, Sapone, difficult. Nevertheless, it is possible to differentiate specific gluten-related disorders from Catassi, Fasano); Shire, Lexington, other conditions, based on currently available investigations and algorithms. -

Conditions Related to Inflammatory Arthritis
Conditions Related to Inflammatory Arthritis There are many conditions related to inflammatory arthritis. Some exhibit symptoms similar to those of inflammatory arthritis, some are autoimmune disorders that result from inflammatory arthritis, and some occur in conjunction with inflammatory arthritis. Related conditions are listed for information purposes only. • Adhesive capsulitis – also known as “frozen shoulder,” the connective tissue surrounding the joint becomes stiff and inflamed causing extreme pain and greatly restricting movement. • Adult onset Still’s disease – a form of arthritis characterized by high spiking fevers and a salmon- colored rash. Still’s disease is more common in children. • Caplan’s syndrome – an inflammation and scarring of the lungs in people with rheumatoid arthritis who have exposure to coal dust, as in a mine. • Celiac disease – an autoimmune disorder of the small intestine that causes malabsorption of nutrients and can eventually cause osteopenia or osteoporosis. • Dermatomyositis – a connective tissue disease characterized by inflammation of the muscles and the skin. The condition is believed to be caused either by viral infection or an autoimmune reaction. • Diabetic finger sclerosis – a complication of diabetes, causing a hardening of the skin and connective tissue in the fingers, thus causing stiffness. • Duchenne muscular dystrophy – one of the most prevalent types of muscular dystrophy, characterized by rapid muscle degeneration. • Dupuytren’s contracture – an abnormal thickening of tissues in the palm and fingers that can cause the fingers to curl. • Eosinophilic fasciitis (Shulman’s syndrome) – a condition in which the muscle tissue underneath the skin becomes swollen and thick. People with eosinophilic fasciitis have a buildup of eosinophils—a type of white blood cell—in the affected tissue. -
Successful Treatment with Rituximab in a Patient with TTP Secondary to Severe ANCA-Associated Vasculitis
□ CASE REPORT □ Successful Treatment with Rituximab in a Patient with TTP Secondary to Severe ANCA-Associated Vasculitis Yukari Asamiya 1, Takahito Moriyama 1, Mari Takano 1, Chihiro Iwasaki 1, Kazuo Kimura 1, Yukako Ando 1, Akiko Aoki 1, Kan Kikuchi 2, Takashi Takei 1, Keiko Uchida 1 and Kosaku Nitta 1 Abstract We report a case of thrombotic thrombocytopenic purpura (TTP) secondary to antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis treated by rituximab. TTP secondary to ANCA-associated vasculitis is very rare and has a high mortality rate. We employed rituximab and successfully treated TTP secondary to ANCA-associated vasculitis, because standard therapies, such as steroid therapy, intravenous pulse cyclophos- phamide, and repeated plasma exchange (PE), did not suppress her disease activity. This is the first report to suggest that rituximab can achieve complete remission of TTP secondary to ANCA-associated vasculitis. Key words: ANCA-associated vasculitis, TTP, rituximab, renal failure, intrapulmonary hemorrhage, hemo- dialysis (Inter Med 49: 1587-1591, 2010) (DOI: 10.2169/internalmedicine.49.3135) pies such as steroids and therapeutic PE (4-6). However, ri- Introduction tuximab was employed mainly against idiopathic TTP, and there were few reports discussing treatment of secondary Antineutrophil cytoplasmic antibody (ANCA)-associated TTP; in particular, TTP with ANCA-associated vasculitis vasculitis is recognized as a multisystem autoimmune dis- was rare. Here, we report a patient with TTP secondary to ease characterized by ANCA production and small vessel in- myeloperoxidase-antineutrophil cytoplasmic antibody (MPO- flammation (1). It’s typical clinical manifestations are rap- ANCA) associated vasculitis who was treated using rituxi- idly progressive glomerulonephritis and the occasional de- mab combined with steroid pulse, IVCY and repeated PE. -

Oral and Maxillo-Facial Manifestations of Systemic Diseases: an Overview
medicina Review Oral and Maxillo-Facial Manifestations of Systemic Diseases: An Overview Saverio Capodiferro *,† , Luisa Limongelli *,† and Gianfranco Favia Department of Interdisciplinary Medicine, University of Bari Aldo Moro, Piazza G. Cesare, 11, 70124 Bari, Italy; [email protected] * Correspondence: [email protected] (S.C.); [email protected] (L.L.) † These authors contributed equally to the paper. Abstract: Many systemic (infective, genetic, autoimmune, neoplastic) diseases may involve the oral cavity and, more generally, the soft and hard tissues of the head and neck as primary or secondary localization. Primary onset in the oral cavity of both pediatric and adult diseases usually represents a true challenge for clinicians; their precocious detection is often difficult and requires a wide knowledge but surely results in the early diagnosis and therapy onset with an overall better prognosis and clinical outcomes. In the current paper, as for the topic of the current Special Issue, the authors present an overview on the most frequent clinical manifestations at the oral and maxillo-facial district of systemic disease. Keywords: oral cavity; head and neck; systemic disease; oral signs of systemic diseases; early diagnosis; differential diagnosis Citation: Capodiferro, S.; Limongelli, 1. Introduction L.; Favia, G. Oral and Maxillo-Facial Oral and maxillo-facial manifestations of systemic diseases represent an extensive and Manifestations of Systemic Diseases: fascinating study, which is mainly based on the knowledge that many signs and symptoms An Overview. Medicina 2021, 57, 271. as numerous systemic disorders may first present as or may be identified by head and https://doi.org/10.3390/ neck tissue changes. -

Cutaneous Manifestations of Systemic Disease
Cutaneous Manifestations of Systemic Disease Dr. Lloyd J. Cleaver D.O. FAOCD FAAD Northeast Regional Medical Center A.T.Still University/KCOM Assistant Vice President/Professor ACOI Board Review Disclosure I have no financial relationships to disclose I will not discuss off label use and/or investigational use in my presentation I do not have direct knowledge of AOBIM questions I have been granted approvial by the AOA to do this board review Dermatology on the AOBIM ”1-4%” of exam is Dermatology Table of Test Specifications is unavailable Review Syllabus for Internal Medicine Large amount of information Cutaneous Multisystem Cutaneous Connective Tissue Conditions Connective Tissue Diease Discoid Lupus Erythematosus Subacute Cutaneous LE Systemic Lupus Erythematosus Scleroderma CREST Syndrome Dermatomyositis Lupus Erythematosus Spectrum from cutaneous to severe systemic involvement Discoid LE (DLE) / Chronic Cutaneous Subacute Cutaneous LE (SCLE) Systemic LE (SLE) Cutaneous findings common in all forms Related to autoimmunity Discoid LE (Chronic Cutaneous LE) Primarily cutaneous Scaly, erythematous, atrophic plaques with sharp margins, telangiectasias and follicular plugging Possible elevated ESR, anemia or leukopenia Progression to SLE only 1-2% Heals with scarring, atrophy and dyspigmentation 5% ANA positive Discoid LE (Chronic Cutaneous LE) Scaly, atrophic plaques with defined margins Discoid LE (Chronic Cutaneous LE) Scaly, erythematous plaques with scarring, atrophy, dyspigmentation DISCOID LUPUS Subacute Cutaneous -

SKIN VERSUS PEMPHIGUS FOLIACEUS and the AUTOIMMUNE GANG Lara Luke, BS, RVT, Dermatology, Purdue Veterinary Teaching Hospital
VETERINARY NURSING EDUCATION SKIN VERSUS PEMPHIGUS FOLIACEUS AND THE AUTOIMMUNE GANG Lara Luke, BS, RVT, Dermatology, Purdue Veterinary Teaching Hospital This program was reviewed and approved by the AAVSB Learning Objective: After reading this article, the participant will be able to dis- RACE program for 1 hour of continuing education in jurisdictions which recognize AAVSB RACE approval. cuss and compare autoimmune diseases that have dermatological afects, includ- Please contact the AAVSB RACE program if you have any ing Pemphigus Foliaceus (PF), Pemphigus Erythematosus (PE), Discoid Lupus comments/concerns regarding this program’s validity or relevancy to the veterinary profession. Erythematosus (DLE), Systemic Lupus Erythematosus (SLE). In addition, the reader will become familiar with diagnostic and treatment techniques. FUNCTION OF THE SKIN Te skin is the largest organ of the body. Along with sensory function, it provides a barrier between the inside and outside world. Te epidermis is composed of the following fve layers: stratum basale, stratum spinosum, stratum granulosum, stratum lucidum, and stratum corneum. Te stratum lucidum is found only on the nasal planum and footpads. When the cells of the epidermis are disrupted by systemic disease, the barrier is also disrupted. Clinical signs of skin disease will bring the patient into the veterinarian’s ofce for diagnosis. 32 THE NAVTA JOURNAL | NAVTA.NET VETERINARY NURSING EDUCATION THE PEMPHIGUS COMPLEX article.3 Histologically it shares characteris- Pemphigus Foliaceus tics of both PF and DLE.1 This classifcation PF is an immune mediated pustular disor- is still considered controversial and PE may der included in a group of diseases known just be a localized variant of PF.1 as the pemphigus complex. -
Syphilis Imitating Urticarial Vasculitis
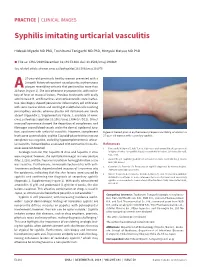
PRACTICE | CLINICAL IMAGES Syphilis imitating urticarial vasculitis Hideaki Miyachi MD PhD, Toshibumi Taniguchi MD PhD, Hiroyuki Matsue MD PhD n Cite as: CMAJ 2019 December 16;191:E1384. doi: 10.1503/cmaj.190469 See related article at www.cmaj.ca/lookup/doi/10.1503/cmaj.191075 27-year-old previously healthy woman presented with a 2-month history of recurrent raised pruritic erythematous plaques resembling urticaria that persisted for more than 24A hours (Figure 1). She was otherwise asymptomatic, with no his- tory of fever or mucosal lesions. Previous treatments with orally administered H1 antihistamines and corticosteroids were ineffec- tive. Skin biopsy showed perivascular inflammatory cell infiltration with some nuclear debris and swelling of endothelial cells involving postcapillary venules, whereas plasma cell infiltration was nearly absent (Appendix 1, Supplementary Figure 1, available at www. cmaj.ca/lookup/suppl/doi:10.1503/cmaj.190469/-/DC1). Direct immunofluorescence showed the deposition of complement and fibrinogen around blood vessels and in the dermal–epidermal junc- tion, consistent with urticarial vasculitis. However, complement Figure 1: Raised pruritic erythematous plaques resembling urticaria in a levels were unremarkable, and the C1q solid-phase test for immune 27-year-old woman with secondary syphilis. complexes was negative, excluding hypocomplementemic urticar- ial vasculitis. Autoantibodies associated with connective tissue dis- References eases were not detected. 1. Tanizaki R, Nichijima T, Aoki T, et al. High-dose oral amoxicillin plus probenecid Serologic tests for HIV, hepatitis B virus and hepatitis C virus is highly effective for syphillis in patients with HIV infection. Clin Infect Dis 2015; 61:177-83. were negative; however, the rapid plasma reagin test was positive (titer, 1:128), and the Treponema pallidum hemagglutination assay 2. -

Cerebral Vasculitis Associated with Shingles J D M Edgar, J J Crosbie, S a Hawkins
The Ulster Medical Joumal, Volume 59, No. 1, pp. 77- 81, April 1990. Case report Cerebral vasculitis associated with shingles J D M Edgar, J J Crosbie, S A Hawkins Accepted 9 August 1989. Shingles is a common manifestation of infection with herpes zoster virus (more correctly varicella-zoster virus) in middle-aged or elderly people. We describe three patients who developed brain stem encephalitis and cerebral vasculitis due to infection with this agent during a 12-month period. CASE 1 A 77-year-old lady initially presented to her family doctor in January 1987. She complained of a painful left ear with associated hearing loss and dizziness. There were vesicles on the left pinna, and she had a left lower motor neurone facial palsy. She was treated for five days with oral acyclovir and topical idoxuridine, but her symptoms did not resolve. Two weeks after the onset she became ataxic, with double vision and nausea. She was admitted to an ear, nose and throat ward, and a neurological opinion was sought. She was fully alert and orientated. There were vesicles on the left pinna. She had gaze -evoked nystagmus on horizontal and vertical gaze, maximum on left lateral gaze. There was a complete left lower motor neurone facial palsy. There was a right carotid artery bruit. There were no other cranial nerve lesions. Power and sensation were fully intact, tendon reflexes were symmetrical but the left plantar response was extensor. She had marked truncal ataxia and left - sided inco - ordination. Computerised tomography scan of the head showed evidence of cerebral atrophy but no focal lesion. -

Skin Manifestations of Systemic Disease
THEME WEIRD SKIN STUFF Adriene Lee BSc(Med), MBBS(Hons), FACD, is visiting dermatologist, St Vincent's Hospital and Monash Medical Centre, and Lecturer, Department of General Practice, Monash University, Victoria. [email protected] Skin manifestations of systemic disease Dermatologic complaints are a common reason for Background presentation to a general practitioner. In such cases, one needs Dermatologic complaints are a common reason for presentation to determine if the complaint may be a manifestation of a more to a general practitioner. In some cases, one needs to determine serious underlying systemic disease. Disorders of the every if the complaint may be a manifestation of a more serious underlying systemic disease. organ system may cause skin symptoms and signs, some of which are due to treatment of these conditions. It is beyond the Objective scope of this review to cover all potential skin manifestations of This article aims to highlight common dermatologic systemic disease. This article highlights the more common, presentations where further assessment is needed to exclude classic and important manifestations in three different groups: an underlying systemic disease, to discuss classic cutaneous features of specific systemic diseases, and to outline rare • ‘When to look further’ – where dermatologic presentations cutaneous paraneoplastic syndromes. require further assessment to exclude underlying systemic disease, and guide appropriate management Discussion • ‘What to look for’ – where certain systemic diseases have Skin manifestations of systemic disease are wide, varied, classic cutaneous findings specific and nonspecific. Generalised pruritus and cutaneous • ‘What not to miss’ – where specific cutaneous signs might be vasculitis are more common cutaneous presentations where an underlying systemic disease may be present and will the initial presentation of an underlying malignancy.