” Disorders of Pigmentation “Why Is My Skin This Color
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Successful Repigmentation of Vitiligo-Like Hypopigmentation in a Case of Acanthosis Nigricans
Brief Report follicles. Clin Exp Dermatol 2005;30:426-428. 4. Feldmann KA, Dawber RP, Pittelkow MR, Ferguson DJ. 2. Giehl KA, Ferguson DJ, Dawber RP, Pittelkow MR, Foehles J, Newly described weathering pattern in pili annulati hair de Berker DA. Update on detection, morphology and fragility shafts: a scanning electron microscopic study. J Am Acad in pili annulati in three kindreds. J Eur Acad Dermatol Dermatol 2001;45:625-627. Venereol 2004;18:654-658. 5. Werner K, St-Surin-Lord S, Sperling LC. Pili annulati associ- 3. Akoglu G, Emre S, Metin A, Erbil KM, Akpolat D, Firat A, et ated with hair fragility: cause or coincidence? Cutis 2013; al. Pili annulati with fragility: electron microscopic findings 91:36-38. of a case. Int J Trichology 2012;4:89-92. https://doi.org/10.5021/ad.2017.29.2.256 Successful Repigmentation of Vitiligo-Like Hypopigmentation in a Case of Acanthosis Nigricans Seung Hyun Chun, Ji Hyun Park, Jae Beom Park, Il-Hwan Kim Department of Dermatology, Korea University Ansan Hospital, College of Medicine, Korea University, Ansan, Korea Dear Editor: Although the patient had previously taken oral metformin Acanthosis nigricans (AN) is characterized by hyper- for a year, he was not taking any medication at the time of pigmented thickened skin with velvety texture in the visit. No similar skin lesions could be found in family flexural areas such as axillae, neck, groin, inner thigh, um- members of the patient. bilicus, and perianal area. Obesity, insulin resistance, and Skin biopsy was performed on both hyperpigmented and hyperinsulinemia are often found in association with AN1. -

Pigmented Purpuric Dermatosis
Journal of Paediatrics and Neonatal Disorders Volume 3 | Issue 2 ISSN: 2456-5482 Case Report Open Access Pigmented Purpuric Dermatosis Jacob M, Wright R, Mazur L and Aly F* Department of Pediatrics, the University of Texas Health Science Center at Houston (UT Health), USA *Corresponding author: Aly F, MD, FAAP, Assistant Professor, Department of Pediatrics, The University of Texas Health Science Center at Houston (UTHealth), USA, Tel: 5053402221, E-mail: [email protected]. edu Citation: Jacob M, Wright R, Mazur L, Aly F (2018) Pigmented Purpuric Dermatosis. J Paediatr Neonatal Dis 3(2): 203 Received Date: June 29, 2018 Accepted Date: August 28, 2018 Published Date: August 30, 2018 Abstract The pigmented purpuric dermatoses (PPD) are skin rashes that are benign but can often be mistaken for other purpura-causing diseases, which must be ruled out. Although they are more prevalent in adults, they can also be seen in children. Though these dermatoses rarely involve other organs, the rash can be distressing for the parents of an adolescent or child. We presented a case of a 15 year old girl with a pathological diagnosis of eczematid-like form of PPD, which clinically diagnosed as the Schamberg’s form of PPD. Biopsy is frequently necessary to reach a final diagnosis. Keywords: Pigmented Purpuric Dermatoses; Schamberg Disease; Eczematid-like Type; Rutoside; Ascorbic Acid List of abbreviations: PPD: Pigmented Purpuric Dermatoses Case Report A 15 year old female presented to the clinic with a six month history of a ‘rash’ on her arms and legs. It started on the feet and spread to her upper legs and arms. -

Cutaneous Manifestations of Systemic Diseases 428 C2 Notes Dr
Cutaneous Manifestations of systemic diseases 428 C2 Notes Dr. Eman Almukhadeb Cutaneous Manifestations of systemic diseases Dr. Eman Almukhadeb CUTANEOUS MANIFESTATIONS OF DIABETES MELLITUS: Specific manifestations: 1 Cutaneous Manifestations of systemic diseases 428 C2 Notes Dr. Eman Almukhadeb 1. Diabetes dermopathy or “SHIN SPOTS”: Most common cutaneous manifestation of diabetes; M > F, males over age 50 years with long standing diabetes. They are: bilateral, symmetrical, atrophic red-brownish macules and patches, over the shins mainly but can occur at any sites, asymptomatic. There is no effective treatment. 2. Necrobiosis Lipoidica Diabeticorum (NLD): Patients classically present with single or multiple red-brown papules, which progress to sharply demarcated yellow-brown atrophic, telangiectatic erythematic plaques with a violaceous, irregular border. Usually it’s unilateral. Common sites include shins followed by ankles, calves, thighs and feet. Very atrophic plaque so any trauma will lead to ulceration, it occurs in about 35% of cases. Cutaneous anesthesia, hypohidrosis and partial alopecia can be found Pathology: Palisading granulomas containing degenerating collagen. The nonenzymatic glycosylation of dermal collagen and elastin will lead to degeneration of the collagen and atrophy (necrobiosis). 2 Cutaneous Manifestations of systemic diseases 428 C2 Notes Dr. Eman Almukhadeb Approximately 60% of NLD patients have diabetes and 20% have glucose intolerance. Conversely, up to 3% of diabetics have NLD, so if a patient has NLD its common that he is diabetic, but not every diabetic patient have NLD. (Important) Women are more affected than men. Treatment: Ulcer prevention (by avoiding trauma). No impact of tight glucose control on likelihood of developing NLD. There are multiple treatment options available and all of them reported to be effective: o Intralesional steroids o Systemic aspirin: 300mg/day and dipyridamole: 75 mg/day. -

Melanocytes and Their Diseases
Downloaded from http://perspectivesinmedicine.cshlp.org/ on October 2, 2021 - Published by Cold Spring Harbor Laboratory Press Melanocytes and Their Diseases Yuji Yamaguchi1 and Vincent J. Hearing2 1Medical, AbbVie GK, Mita, Tokyo 108-6302, Japan 2Laboratory of Cell Biology, National Cancer Institute, National Institutes of Health, Bethesda, Maryland 20892 Correspondence: [email protected] Human melanocytes are distributed not only in the epidermis and in hair follicles but also in mucosa, cochlea (ear), iris (eye), and mesencephalon (brain) among other tissues. Melano- cytes, which are derived from the neural crest, are unique in that they produce eu-/pheo- melanin pigments in unique membrane-bound organelles termed melanosomes, which can be divided into four stages depending on their degree of maturation. Pigmentation production is determined by three distinct elements: enzymes involved in melanin synthesis, proteins required for melanosome structure, and proteins required for their trafficking and distribution. Many genes are involved in regulating pigmentation at various levels, and mutations in many of them cause pigmentary disorders, which can be classified into three types: hyperpigmen- tation (including melasma), hypopigmentation (including oculocutaneous albinism [OCA]), and mixed hyper-/hypopigmentation (including dyschromatosis symmetrica hereditaria). We briefly review vitiligo as a representative of an acquired hypopigmentation disorder. igments that determine human skin colors somes can be divided into four stages depend- Pinclude melanin, hemoglobin (red), hemo- ing on their degree of maturation. Early mela- siderin (brown), carotene (yellow), and bilin nosomes, especially stage I melanosomes, are (yellow). Among those, melanins play key roles similar to lysosomes whereas late melanosomes in determining human skin (and hair) pigmen- contain a structured matrix and highly dense tation. -

Update on Challenging Disorders of Pigmentation in Skin of Color Heather Woolery-Lloyd, M.D
Update on Challenging Disorders of Pigmentation in Skin of Color Heather Woolery-Lloyd, M.D. Director of Ethnic Skin Care Voluntary Assistant Professor Miller/University of Miami School of Medicine Department of Dermatology and Cutaneous Surgery What Determines Skin Color? What Determines Skin Color? No significant difference in the number of melanocytes between the races 2000 epidermal melanocytes/mm2 on head and forearm 1000 epidermal melanocytes/mm2 on the rest of the body differences present at birth Jimbow K, Quevedo WC, Prota G, Fitzpatrick TB (1999) Biology of melanocytes. In I. M. Freedberg, A.Z. Eisen, K. Wolff,K.F. Austen, L.A. Goldsmith, S. I. Katz, T. B. Fitzpatrick (Eds.), Dermatology in General Medicine 5th ed., pp192-220, New York, NY: McGraw Hill Melanosomes in Black and White Skin Black White Szabo G, Gerald AB, Pathak MA, Fitzpatrick TB. Nature1969;222:1081-1082 Jimbow K, Quevedo WC, Prota G, Fitzpatrick TB (1999) Biology of melanocytes. In I. M. Freedberg, A.Z. Eisen, K. Wolff, K.F. Austen, L.A. Goldsmith, S. I. Katz, T. B. Fitzpatrick (Eds.), Dermatology in General Medicine 5th ed., pp192- 220, New York, NY: McGraw Hill Role of Melanin-Advantages Melanin absorbs and scatters energy from UV and visible light to protect epidermal cells from UV damage Disadvantages Inflammation or injury to the skin is almost immediately accompanied by alteration in pigmentation Hyperpigmentation Hypopigmentation Dyschromias Post-Inflammatory hyperpigmentation Acne Melasma Lichen Planus Pigmentosus Progressive Macular Hypomelanosis -

Chapter 3 Bacterial and Viral Infections
GBB03 10/4/06 12:20 PM Page 19 Chapter 3 Bacterial and viral infections A mighty creature is the germ gain entry into the skin via minor abrasions, or fis- Though smaller than the pachyderm sures between the toes associated with tinea pedis, His customary dwelling place and leg ulcers provide a portal of entry in many Is deep within the human race cases. A frequent predisposing factor is oedema of His childish pride he often pleases the legs, and cellulitis is a common condition in By giving people strange diseases elderly people, who often suffer from leg oedema Do you, my poppet, feel infirm? of cardiac, venous or lymphatic origin. You probably contain a germ The affected area becomes red, hot and swollen (Ogden Nash, The Germ) (Fig. 3.1), and blister formation and areas of skin necrosis may occur. The patient is pyrexial and feels unwell. Rigors may occur and, in elderly Bacterial infections people, a toxic confusional state. In presumed streptococcal cellulitis, penicillin is Streptococcal infection the treatment of choice, initially given as ben- zylpenicillin intravenously. If the leg is affected, Cellulitis bed rest is an important aspect of treatment. Where Cellulitis is a bacterial infection of subcutaneous there is extensive tissue necrosis, surgical debride- tissues that, in immunologically normal individu- ment may be necessary. als, is usually caused by Streptococcus pyogenes. A particularly severe, deep form of cellulitis, in- ‘Erysipelas’ is a term applied to superficial volving fascia and muscles, is known as ‘necrotiz- streptococcal cellulitis that has a well-demarcated ing fasciitis’. This disorder achieved notoriety a few edge. -

Reticulate Hyperpigmentation of the Skin After Topical Application Of
Letters to the Editor 301 Reticulate Hyperpigmentation of the Skin After Topical Application of Benzoyl Peroxide Sir, Our two patients appeared to develop an irritant response on Benzoyl peroxide (BP) is an e¡ective and frequently used topical thetrunk afterapplication of 5% benzoyl peroxide. One medication for the treatment of acne vulgaris. It is a strong, patient applied BP to his face withnoirritation,consistentwith broad spectrum bactericidal agent that signi¢cantly decreases the ¢ndings of Hausteinetal.(3). Both patients then developed the number of Propionibacterium acnes in both the follicle and apattern of reticulate hyperpigmentation after their initial der- on surface skin (1). A common side e¡ect after usage is irritation matitis subsided. Biopsy in both cases was consistent with of the skin, usually manifested as a stinging or burning, and postin£ammatory hyperpigmentation. sometimes accompanied by erythema and scaling. Benzoyl per- Postin£ammatory hyperpigmentation develops after acute oxide is a strong irritant, but a weak allergen, rarely causing a or chronic in£ammation and trauma to the skin. The intensity contact dermatitis (2, 3). Tolerance can be achieved by gradually of the hypermelanosistendstobe more pronounced in darker- increasing the frequency of application over time. We describe skinnedindividuals. Other conditions that produce a pattern of two cases in which topical application of benzoyl peroxide reticulate hyperpigmentation include Riehl's melanosis, resulted in an unusual pattern of reticulate hyperpigmentation which is characterized by reticulate brown-black pigmenta- of the skin, most likely as a sequela of an irritant contact derma- tion of the face and neck. This is thought to be a result of a titis. -

Dermatology DDX Deck, 2Nd Edition 65
63. Herpes simplex (cold sores, fever blisters) PREMALIGNANT AND MALIGNANT NON- 64. Varicella (chicken pox) MELANOMA SKIN TUMORS Dermatology DDX Deck, 2nd Edition 65. Herpes zoster (shingles) 126. Basal cell carcinoma 66. Hand, foot, and mouth disease 127. Actinic keratosis TOPICAL THERAPY 128. Squamous cell carcinoma 1. Basic principles of treatment FUNGAL INFECTIONS 129. Bowen disease 2. Topical corticosteroids 67. Candidiasis (moniliasis) 130. Leukoplakia 68. Candidal balanitis 131. Cutaneous T-cell lymphoma ECZEMA 69. Candidiasis (diaper dermatitis) 132. Paget disease of the breast 3. Acute eczematous inflammation 70. Candidiasis of large skin folds (candidal 133. Extramammary Paget disease 4. Rhus dermatitis (poison ivy, poison oak, intertrigo) 134. Cutaneous metastasis poison sumac) 71. Tinea versicolor 5. Subacute eczematous inflammation 72. Tinea of the nails NEVI AND MALIGNANT MELANOMA 6. Chronic eczematous inflammation 73. Angular cheilitis 135. Nevi, melanocytic nevi, moles 7. Lichen simplex chronicus 74. Cutaneous fungal infections (tinea) 136. Atypical mole syndrome (dysplastic nevus 8. Hand eczema 75. Tinea of the foot syndrome) 9. Asteatotic eczema 76. Tinea of the groin 137. Malignant melanoma, lentigo maligna 10. Chapped, fissured feet 77. Tinea of the body 138. Melanoma mimics 11. Allergic contact dermatitis 78. Tinea of the hand 139. Congenital melanocytic nevi 12. Irritant contact dermatitis 79. Tinea incognito 13. Fingertip eczema 80. Tinea of the scalp VASCULAR TUMORS AND MALFORMATIONS 14. Keratolysis exfoliativa 81. Tinea of the beard 140. Hemangiomas of infancy 15. Nummular eczema 141. Vascular malformations 16. Pompholyx EXANTHEMS AND DRUG REACTIONS 142. Cherry angioma 17. Prurigo nodularis 82. Non-specific viral rash 143. Angiokeratoma 18. Stasis dermatitis 83. -
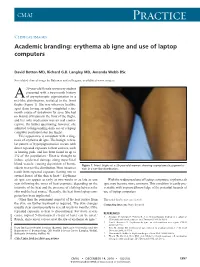
Erythema Ab Igne and Use of Laptop Computers
CMAJ Practice Clinical images Academic branding: erythema ab igne and use of laptop computers David Botten MD, Richard G.B. Langley MD, Amanda Webb BSc See related clinical image by Beleznay and colleagues, available at www.cmaj.ca 20-year-old female university student presented with a two-month history A of asymptomatic pigmentation in a net-like distribution, isolated to the front thighs (Figure 1). She was otherwise healthy, apart from having recently completed a six- month course of isotretinoin for acne. She had no history of trauma to the front of the thighs, and her only medication was an oral contra- ceptive. On further questioning, however, she admitted to longstanding daily use of a laptop computer positioned atop her thighs. This appearance is consistent with a diag- nosis of erythema ab igne. The benign, reticu- lar pattern of hyperpigmentation occurs with direct repeated exposure to heat sources, such as heating pads, and has been found in up to 3% of the population.1 Heat is thought to induce epidermal damage along superficial blood vessels, causing deposition of hemo- Figure 1: Front thighs of a 20-year-old woman showing asymptomatic pigmenta- siderin in a net-like distribution. Most instances tion in a net-like distribution. result from repeated exposure (lasting one to several hours) of the skin to heat.2,3 Erythema ab igne can appear as early as two weeks or as late as one With the widespread use of laptop computers, erythema ab year following the onset of heat exposure, depending on the igne may become more common. -

Clinicopathological Correlation of Acquired Hyperpigmentary Disorders
Symposium Clinicopathological correlation of acquired Dermatopathology hyperpigmentary disorders Anisha B. Patel, Raj Kubba1, Asha Kubba1 Department of Dermatology, ABSTRACT Oregon Health Sciences University, Portland, Oregon, Acquired pigmentary disorders are group of heterogenous entities that share single, most USA, 1Delhi Dermatology Group, Delhi Dermpath significant, clinical feature, that is, dyspigmentation. Asians and Indians, in particular, are mostly Laboratory, New Delhi, India affected. Although the classic morphologies and common treatment options of these conditions have been reviewed in the global dermatology literature, the value of histpathological evaluation Address for correspondence: has not been thoroughly explored. The importance of accurate diagnosis is emphasized here as Dr. Asha Kubba, the underlying diseases have varying etiologies that need to be addressed in order to effectively 10, Aradhana Enclave, treat the dyspigmentation. In this review, we describe and discuss the utility of histology in the R.K. Puram, Sector‑13, diagnostic work of hyperpigmentary disorders, and how, in many cases, it can lead to targeted New Delhi ‑ 110 066, India. E‑mail: and more effective therapy. We focus on the most common acquired pigmentary disorders [email protected] seen in Indian patients as well as a few uncommon diseases with distinctive histological traits. Facial melanoses, including mimickers of melasma, are thoroughly explored. These diseases include lichen planus pigmentosus, discoid lupus erythematosus, drug‑induced melanoses, hyperpigmentation due to exogenous substances, acanthosis nigricans, and macular amyloidosis. Key words: Facial melanoses, histology of hyperpigmentary disorders and melasma, pigmentary disorders INTRODUCTION focus on the most common acquired hyperpigmentary disorders seen in Indian patients as well as a few Acquired pigmentary disorders are found all over the uncommon diseases with distinctive histological traits. -

Incontinentia Pigmenti
Incontinentia Pigmenti Authors: Prof Nikolaos G. Stavrianeas1,2, Dr Michael E. Kakepis Creation date: April 2004 1Member of The European Editorial Committee of Orphanet Encyclopedia 2Department of Dermatology and Venereology, A. Sygros Hospital, National and Kapodistrian University of Athens, Athens, Greece. [email protected] Abstract Keywords Definition Epidemiology Etiology Clinical features Course and prognosis Pathology Differential diagnosis Antenatal diagnosis Treatment References Abstract Incontinentia pigmenti (IP) is an X-linked dominant single-gene disorder of skin pigmentation with neurologic, ophthalmologic, and dental involvement. IP is characterized by abnormalities of the tissues and organs derived from the ectoderm and mesoderm. The locus for IP is genetically linked to the factor VIII gene on chromosome band Xq28. Mutations in NEMO/IKK-y, which encodes a critical component of the nuclear factor-kB (NF-kB) signaling pathway, are responsible for IP. IP is a rare disease (about 700 cases reported) with a worldwide distribution, more common among white patients. Characteristic skin lesions are usually present at birth in approximately 90% of patients, or they develop in early infancy. The skin changes evolve in 4 stages in a fixed chronological order. Skin, hair, nails, dental abnormalities, seizures, developmental delay, mental retardation, ataxia, spastic abnormalities, microcephaly, cerebral atrophy, hypoplasia of the corpus callosum, periventricular cerebral edema may occur in more than 50% of reported cases. Ocular defects, atrophic patchy alopecia, dwarfism, clubfoot, spina bifida, hemiatrophy, and congenital hip dislocation, are reported. Treatment of cutaneous lesions is usually not required. Standard wound care should be provided in case of inflammation. Regular dental care is necessary. Pediatric ophthalmologist or retinal specialist consultations are essential. -

Lepromatous Leprosy with Erythema Nodosum Leprosum Presenting As
Lepromatous Leprosy with Erythema Nodosum Leprosum Presenting as Chronic Ulcers with Vasculitis: A Case Report and Discussion Anny Xiao, DO,* Erin Lowe, DO,** Richard Miller, DO, FAOCD*** *Traditional Rotating Intern, PGY-1, Largo Medical Center, Largo, FL **Dermatology Resident, PGY-2, Largo Medical Center, Largo, FL ***Program Director, Dermatology Residency, Largo Medical Center, Largo, FL Disclosures: None Correspondence: Anny Xiao, DO; Largo Medical Center, Graduate Medical Education, 201 14th St. SW, Largo, FL 33770; 510-684-4190; [email protected] Abstract Leprosy is a rare, chronic, granulomatous infectious disease with cutaneous and neurologic sequelae. It can be a challenging differential diagnosis in dermatology practice due to several overlapping features with rheumatologic disorders. Patients with leprosy can develop reactive states as a result of immune complex-mediated inflammatory processes, leading to the appearance of additional cutaneous lesions that may further complicate the clinical picture. We describe a case of a woman presenting with a long history of a recurrent bullous rash with chronic ulcers, with an evolution of vasculitic diagnoses, who was later determined to have lepromatous leprosy with reactive erythema nodosum leprosum (ENL). Introduction accompanied by an intense bullous purpuric rash on management of sepsis secondary to bacteremia, Leprosy is a slowly progressive disease caused by bilateral arms and face. For these complaints she was with lower-extremity cellulitis as the suspected infection with Mycobacterium leprae (M. leprae). seen in a Complex Medical Dermatology Clinic and source. A skin biopsy was taken from the left thigh, Spread continues at a steady rate in several endemic clinically diagnosed with cutaneous polyarteritis and histopathology showed epidermal ulceration countries, with more than 200,000 new cases nodosa.