Melasma on the Nape of the Neck in a Man
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Melanocytes and Their Diseases
Downloaded from http://perspectivesinmedicine.cshlp.org/ on October 2, 2021 - Published by Cold Spring Harbor Laboratory Press Melanocytes and Their Diseases Yuji Yamaguchi1 and Vincent J. Hearing2 1Medical, AbbVie GK, Mita, Tokyo 108-6302, Japan 2Laboratory of Cell Biology, National Cancer Institute, National Institutes of Health, Bethesda, Maryland 20892 Correspondence: [email protected] Human melanocytes are distributed not only in the epidermis and in hair follicles but also in mucosa, cochlea (ear), iris (eye), and mesencephalon (brain) among other tissues. Melano- cytes, which are derived from the neural crest, are unique in that they produce eu-/pheo- melanin pigments in unique membrane-bound organelles termed melanosomes, which can be divided into four stages depending on their degree of maturation. Pigmentation production is determined by three distinct elements: enzymes involved in melanin synthesis, proteins required for melanosome structure, and proteins required for their trafficking and distribution. Many genes are involved in regulating pigmentation at various levels, and mutations in many of them cause pigmentary disorders, which can be classified into three types: hyperpigmen- tation (including melasma), hypopigmentation (including oculocutaneous albinism [OCA]), and mixed hyper-/hypopigmentation (including dyschromatosis symmetrica hereditaria). We briefly review vitiligo as a representative of an acquired hypopigmentation disorder. igments that determine human skin colors somes can be divided into four stages depend- Pinclude melanin, hemoglobin (red), hemo- ing on their degree of maturation. Early mela- siderin (brown), carotene (yellow), and bilin nosomes, especially stage I melanosomes, are (yellow). Among those, melanins play key roles similar to lysosomes whereas late melanosomes in determining human skin (and hair) pigmen- contain a structured matrix and highly dense tation. -

Frequency of Different Types of Facial Melanoses Referring to the Department of Dermatology and Venereology, Nepal Medical Colle
Amatya et al. BMC Dermatology (2020) 20:4 https://doi.org/10.1186/s12895-020-00100-3 RESEARCH ARTICLE Open Access Frequency of different types of facial melanoses referring to the Department of Dermatology and Venereology, Nepal Medical College and Teaching Hospital in 2019, and assessment of their effect on health-related quality of life Bibush Amatya* , Anil Kumar Jha and Shristi Shrestha Abstract Background: Abnormalities of facial pigmentation, or facial melanoses, are a common presenting complaint in Nepal and are the result of a diverse range of conditions. Objectives: The objective of this study was to determine the frequency, underlying cause and impact on quality of life of facial pigmentary disorders among patients visiting the Department of Dermatology and Venereology, Nepal Medical College and Teaching Hospital (NMCTH) over the course of one year. Methods: This was a cross-sectional study conducted at the Department of Dermatology and Venereology, NMCT H. We recruited patients with facial melanoses above 16 years of age who presented to the outpatient department. Clinical and demographic data were collected and all the enrolled participants completed the validated Nepali version of the Dermatology Life Quality Index (DLQI). Results: Between January 5, 2019 to January 4, 2020, a total of 485 patients were recruited in the study. The most common diagnoses were melasma (166 patients) and post acne hyperpigmentation (71 patients). Quality of life impairment was highest in patients having melasma with steroid induced rosacea-like dermatitis (DLQI = 13.54 ± 1.30), while it was lowest in participants with ephelides (2.45 ± 1.23). Conclusion: Facial melanoses are a common presenting complaint and lead to substantial impacts on quality of life. -

An Unusual Presentation of a Unilateral Asymptomatic Riehl's
ts & C por a e se R S l Michael, Med Rep Case Stud 2018, 3:1 t a u c d i i DOI: 10.4172/2572-5130.1000152 d e s e M + Medical Reports and Case Studies ISSN: 2572-5130 Case Report Open Access An Unusual Presentation of a Unilateral Asymptomatic Riehl’s Melanosis in a 45 Year Old Male Chan Kam Tim Michael* Department of Dermatology, Hong Kong Academy of Medicine, Hong Kong *Corresponding author: Chan Kam Tim Michael, Department of Dermatology, Hong Kong Academy of Medicine, Hong Kong, Tel: +85221282129; E-mail: [email protected] Received Date: Feb 12, 2018; Accepted Date: Mar 12, 2018; Published Date: Mar 21, 2018 Copyright: © 2018 Michael CKT. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Introduction but of post-inflammatory hyperpigmentation, Acquired unilateral Nevus (Hori’s Nevus), Riehl’s melanosis, Drug-induced Pigmented contact dermatitis (PCD), also known as Riehl’s hyperpigmentation, Lichenoid dermatitis; as well as Melasma and melanosis, is a rare facial hyperpigmentation usually secondary to Ochronosis. cosmetics. There are few documented reports in the literature, and many cases without proven diagnosis may have been treated with pigment lasers, especially in beauty parlour settings. We report a case referred from a private practitioner who has a special interest in dermatology. The patient was diagnosed subsequently as having Riehl’s melanosis and treated with non-tyrosinase inhibitor bleaching agents, sun avoidance and mandatory abstinence from over-the-counter cosmetic products. -

Poikiloderma of Civatte, Slapped Neck Solar Melanosis, Basal Melanin Stores
American Journal of Dermatology and Venereology 2019, 8(1): 8-13 DOI: 10.5923/j.ajdv.20190801.03 Slapped Neck Solar Melanosis: Is It a New Entity or a Variant of Poikiloderma of Civatte?? (Clinical and Histopathological Study) Khalifa E. Sharquie1,*, Adil A. Noaimi2, Ansam B. Kaftan3 1Department of Dermatology, College of Medicine, University of Baghdad 2Iraqi and Arab Board for Dermatology and Venereology, Dermatology Center, Medical City, Baghdad, Iraq 3Dermatology Center, Medical City, Baghdad, Iraq Abstract Background: Poikiloderma of Civatte although is a common complaint among population, especially European, still it was not reported in dark skin people as in Iraqi population. Objectives: To study all the clinical and histopathological features of Poikiloderma of Civatte in Iraqi population. Patients and Methods: This study is descriptive, clinical and histopathological study. It was carried out at the Dermatology Center, Medical City, Baghdad, Iraq, from September 2017 to October 2018. Thirty-one patients with Poikiloderma of Civatte were included and evaluated by history, physical examination, Wood’s light examination. Lesional skin biopsies were obtained from 9 patients, with histological examination of the sections stained with Hematoxylin and Eosin (H&E) and Fontana-Masson stain. Results: Thirty-one patients were included in this study, with mean age +/- SD was 53.32+/-10 years, and all patients were males. Twenty-six patients (84%) were with skin phenotype III&IV, The pigmentation was either mainly erythematous (22.5%), mainly dark brown pigmentation (29%), and mixed type of pigmentation (48.5%). These lesions were distributed on the sides of the neck and the face and the V shaped area of the chest. -
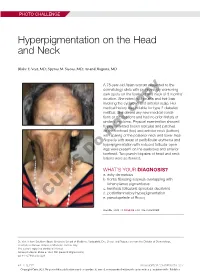
Hyperpigmentation on the Head and Neck
PHOTO CHALLENGE Hyperpigmentation on the Head and Neck Blake E. Vest, MD; Spyros M. Siscos, MD; Anand Rajpara, MD A 78-year-old Asian woman presented to the dermatology clinic with progressively worsening dark spots on the forehead and neck of 3 months’ duration. She noted mild pruritis and hair loss involving the eyebrows and anterior scalp. Her medical history was notable for type 2 diabetes mellitus. She deniedcopy any new medical condi- tions or medications and had no prior history of similar symptoms. Physical examination showed hyperpigmented brown macules and patches on the forehead (top) and anterior neck (bottom) withnot sparing of the posterior neck and lower face. Alopecia with areas of perifollicular erythema and hyperpigmentation with reduced follicular open- ings were present on the eyebrows and anterior Doforehead. Two punch biopsies of head and neck lesions were performed. WHAT’S YOUR DIAGNOSIS? a. ashy dermatosis b. frontal fibrosing alopecia overlapping with lichen planus pigmentosus c. keratosis follicularis spinulosa decalvans d. postinflammatory hyperpigmentation CUTIS e. pseudopelade of Brocq PLEASE TURN TO PAGE E3 FOR THE DIAGNOSIS Dr. Vest is from Southern Illinois University School of Medicine, Springfield. Drs. Siscos and Rajpara are from the Division of Dermatology, University of Kansas School of Medicine, Kansas City. The authors report no conflict of interest. Correspondence: Blake E. Vest, MD ([email protected]). doi:10.12788/cutis.0226 E2 I CUTIS® WWW.MDEDGE.COM/DERMATOLOGY Copyright Cutis 2021. No part of this publication may be reproduced, stored, or transmitted without the prior written permission of the Publisher. PHOTO CHALLENGE DISCUSSION THE DIAGNOSIS: Frontal Fibrosing Alopecia Overlapping With Lichen Planus Pigmentosus icroscopic examination revealed focal dermal of the skin have been reported, including the entire pigmentation, papillary fibrosis, and epidermal scalp, eyebrows, and eyelashes. -

Pigmented Contact Dermatitis and Chemical Depigmentation
18_319_334* 05.11.2005 10:30 Uhr Seite 319 Chapter 18 Pigmented Contact Dermatitis 18 and Chemical Depigmentation Hideo Nakayama Contents ca, often occurs without showing any positive mani- 18.1 Hyperpigmentation Associated festations of dermatitis such as marked erythema, with Contact Dermatitis . 319 vesiculation, swelling, papules, rough skin or scaling. 18.1.1 Classification . 319 Therefore, patients may complain only of a pigmen- 18.1.2 Pigmented Contact Dermatitis . 320 tary disorder, even though the disease is entirely the 18.1.2.1 History and Causative Agents . 320 result of allergic contact dermatitis. Hyperpigmenta- 18.1.2.2 Differential Diagnosis . 323 tion caused by incontinentia pigmenti histologica 18.1.2.3 Prevention and Treatment . 323 has often been called a lichenoid reaction, since the 18.1.3 Pigmented Cosmetic Dermatitis . 324 presence of basal liquefaction degeneration, the ac- 18.1.3.1 Signs . 324 cumulation of melanin pigment, and the mononucle- 18.1.3.2 Causative Allergens . 325 ar cell infiltrate in the upper dermis are very similar 18.1.3.3 Treatment . 326 to the histopathological manifestations of lichen pla- 18.1.4 Purpuric Dermatitis . 328 nus. However, compared with typical lichen planus, 18.1.5 “Dirty Neck” of Atopic Eczema . 329 hyperkeratosis is usually milder, hypergranulosis 18.2 Depigmentation from Contact and saw-tooth-shape acanthosis are lacking, hyaline with Chemicals . 330 bodies are hardly seen, and the band-like massive in- 18.2.1 Mechanism of Leukoderma filtration with lymphocytes and histiocytes is lack- due to Chemicals . 330 ing. 18.2.2 Contact Leukoderma Caused Mainly by Contact Sensitization . -

Hereditary Hearing Impairment with Cutaneous Abnormalities
G C A T T A C G G C A T genes Review Hereditary Hearing Impairment with Cutaneous Abnormalities Tung-Lin Lee 1 , Pei-Hsuan Lin 2,3, Pei-Lung Chen 3,4,5,6 , Jin-Bon Hong 4,7,* and Chen-Chi Wu 2,3,5,8,* 1 Department of Medical Education, National Taiwan University Hospital, Taipei City 100, Taiwan; [email protected] 2 Department of Otolaryngology, National Taiwan University Hospital, Taipei 11556, Taiwan; [email protected] 3 Graduate Institute of Clinical Medicine, National Taiwan University College of Medicine, Taipei City 100, Taiwan; [email protected] 4 Graduate Institute of Medical Genomics and Proteomics, National Taiwan University College of Medicine, Taipei City 100, Taiwan 5 Department of Medical Genetics, National Taiwan University Hospital, Taipei 10041, Taiwan 6 Department of Internal Medicine, National Taiwan University Hospital, Taipei 10041, Taiwan 7 Department of Dermatology, National Taiwan University Hospital, Taipei City 100, Taiwan 8 Department of Medical Research, National Taiwan University Biomedical Park Hospital, Hsinchu City 300, Taiwan * Correspondence: [email protected] (J.-B.H.); [email protected] (C.-C.W.) Abstract: Syndromic hereditary hearing impairment (HHI) is a clinically and etiologically diverse condition that has a profound influence on affected individuals and their families. As cutaneous findings are more apparent than hearing-related symptoms to clinicians and, more importantly, to caregivers of affected infants and young individuals, establishing a correlation map of skin manifestations and their underlying genetic causes is key to early identification and diagnosis of syndromic HHI. In this article, we performed a comprehensive PubMed database search on syndromic HHI with cutaneous abnormalities, and reviewed a total of 260 relevant publications. -

Treatment of Poikiloderma of Civatte with Ablative Fractional Laser Resurfacing: Prospective Study and Review of the Literature Emily P
JUNE 2009 527 Vo l u m e 8 • Is s u e 6 CO P YR IGHT © 2009 ORIGINAL ARTICLES JOURN A L OF DRUGS IN DER MA TOLOGY Treatment of Poikiloderma of Civatte With Ablative Fractional Laser Resurfacing: Prospective Study and Review of the Literature emily P. Tierney MD and C. William Hanke MD MPH Laser and Skin Surgery Center of Indiana, Carmel, IN ABSTRACT Background: Previous laser treatments for Poikiloderma of Civatte (PC) (i.e., Pulsed dye, Intense Pulsed Light, KTP and Argon) are limited by side effect profiles and/or efficacy. Given the high degree of safety and efficacy of ablative fractional photothermolysis (AFP) for photoaging, we set out to assess the efficacy of PC with AFP. Design: A prospective pilot study for PC in 10 subjects with a series of 1−3 treatment sessions. Treatment sessions were adminis- tered at 6−8 week intervals with blinded physician photographic analysis of improvement at 2 months post-treatment. Evaluation was performed of five clinical indicators, erythema/telangiecatasia, dyschromia, skin texture, skin laxity and cosmetic outcome. Results: The number of treatments required for improvement of PC ranged from 1 to 3, with an average of 1.4. For erythema/te- langiecatasia, the mean score improved 65.0% (95% CI: 60.7%, 69.3%) dyschromia, 66.7% (95% CI: 61.8%, 71.6%), skin texture, 51.7% (95% CI: 48.3%, 55.1%) and skin laxity, 52.5% (95% CI: 49.6%, 55.4%). For cosmetic outcome, the mean score improved 66.7% (95% CI: 62.6%, 70.8%) at 2 months post treatment. -
Xeroderma Pigmentosum: an Insight Into DNA Repair Processes
ACCME/Disclosures The USCAP requires that anyone in a position to influence or control the content of CME disclose any relevant financial relationship WITH COMMERCIAL INTERESTS which they or their spouse/partner have, or have had, within the past 12 months, which relates to the content of this educational activity and creates a conflict of interest. Dr. Jennifer O. Black declares she has no conflict(s) of interest to disclose. Xeroderma Pigmentosum: An Insight into DNA Repair Processes Jennifer O. Black, MD Assistant Professor Division of Pediatric Pathology and Laboratory Medicine Children’s Hospital Colorado University of Colorado Anschutz Medical Campus Aurora, Colorado Introduction: Xeroderma Pigmentosum Xeroderma Pigmentosum (XP): • Initially described 1874 • Rare autosomal recessive disorder • Prevalence: 1-45/million, variable ethnic frequency • UV radiation sensitivity disorder characterized by: • Severe skin burning following minimal sun exposure • Early freckling (before 2 years of age) • Skin cancer at an early age Kraemer KH, DiGiovann JJ. Photochemistry and Photobiology 91:452-459, 2015 Introduction: Xeroderma Pigmentosum XP Clinical Spectrum: • Skin Changes: o Early freckling and subsequent checkered pigmentation o Thin, dry, contracted skin o Telangiectasias o Skin cancers: o Squamous cell carcinoma o Basal cell carcinoma o Melanoma Courtesy Dr. Bahig M. Shehata, Children’s Healthcare of Atlanta Introduction: Xeroderma Pigmentosum Squamous Cell Carcinoma Robbins and Cotran Pathologic Basis of Disease. Lazar, Alexander J.F.; -

Journal of Pigmentary Disorders Yayli, Pigmentary Disorders 2015, 2:1 DOI: 10.4172/2376-0427.1000158
igmentar f P y D l o i a so n r r d u e r o J s Journal of Pigmentary Disorders Yayli, Pigmentary Disorders 2015, 2:1 DOI: 10.4172/2376-0427.1000158 ISSN: 2376-0427 Review Open Access Treatment of Hyperpigmentation in Darker Skins Savas Yayli* Department of Dermatology, Faculty of Medicine, Karadeniz Technical University, Trabzon, Turkey *Corresponding author: Savas Yayli, Department of Dermatology, Faculty of Medicine, Karadeniz Technical University, Trabzon, Turkey, Tel: 90 462 377 53 88; E- mail: [email protected] Rec date: Dec 14, 2014; Acc date: Dec 28, 2014; Pub date: Jan 02, 2015 Copyright: © 2015 Yayli S, This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Introduction many newer agents are in the market [6]. Beside those newers, fixed TC including hydroquinone 4%, tretinoine 0.05%, flucinolon Darker skin or skin of colour means higher Fitzpatrick skin types in acetonide 0.01% is shown as the therapy with highest evidence – still a wide range of racial and ethnic groups referring to persons from little controlled studies - in Latin guide of melasma or recent reviews. African, Asian, Native American, Middle Eastern and Hispanic If there is an irritation or allergy to one of compounds of this TC, one backgrounds. Darker skin types are characterized by higher content of may use it as dual combinations. In Latin guide for treatment of melanin, higher eumelanin to pheomelanin ratio. This is an advantage melasma, second line therapies are TC plus peels or for protection against ultraviolet (UV) radiation, however it also microdermabrasion, and lastly lasers and light sources [4,7]. -

Congenital Horner Syndrome with Heterochromia Iridis Associated with Ipsilateral Internal Carotid Artery Hypoplasia
CASE REPORT Print ISSN 1738-6586 / On-line ISSN 2005-5013 J Clin Neurol 2014 Open Access Congenital Horner Syndrome with Heterochromia Iridis Associated with Ipsilateral Internal Carotid Artery Hypoplasia Fabrice C. Deprez,a Julie Coulier,b Denis Rommel,a Antonella Boschib aDepartments of Radiology and bOphthalmology, Cliniques Universitaires Saint-Luc, UCL, Brussels, Belgium BackgroundzzHorner syndrome (HS), also known as Claude-Bernard-Horner syndrome or Received August 5, 2013 oculosympathetic palsy, comprises ipsilateral ptosis, miosis, and facial anhidrosis. Revised April 15, 2014 Accepted April 21, 2014 Case ReportzzWe report herein the case of a 67-year-old man who presented with congenital HS associated with ipsilateral hypoplasia of the internal carotid artery (ICA), as revealed by Correspondence heterochromia iridis and confirmed by computed tomography (CT). Fabrice C. Deprez, MD Department of Radiology, ConclusionszzCT evaluation of the skull base is essential to establish this diagnosis and dis- Cliniques Universitaires Saint-Luc, tinguish aplasia from agenesis/hypoplasia (by the absence or hypoplasia of the carotid canal) or UCL, Avenue Hippocrate 10, from acquired ICA obstruction as demonstrated by angiographic CT. 1200 Woluwe-Saint-Lambert, J Clin Neurol 2014 Belgium Tel +32.472.93.34.80 Key Wordszzcongenital horner syndrome, internal carotid artery agenesis, Fax +32.81.42.35.05 heterochromia iridis, computed tomography. E-mail [email protected] Introduction spindly left ICA, which was misinterpreted as ICA thrombosis (Fig. 1). The left anterior cerebral artery and MCA were sup- Horner syndrome (HS), also known as Claude-Bernard-Horn- plied by a large posterior communicating artery from the bas- er syndrome or oculosympathetic palsy, comprises ipsilateral ilar artery. -

Reversal of Laser-Induced Hypopigmentation with a Narrow-Band UV-B Light Source in a Patient with Skin Type VI
Reversal of Laser-Induced Hypopigmentation with a Narrow-Band UV-B Light Source in a Patient with Skin Type VI Ã y yz ANETTA RESZKO, MD, PHD, SEAN A. SUKAL, MD, PHD, AND ROY G. GERONEMUS,MD Dr. Geronemus is on the Lumenis Medical Advisory Board. evus of Ota (nevus fuscoceruleus ophthalmo- tion after clearance of a nevus of Ota with a QSRL Nmaxillaris) is a benign dermal melanocytic in an African American Skin Type VI male with a hematoma clinically appearing as a bluish-brown narrow-band ultraviolet B (NB UV-B) source. discoloration in the ophthalmic and/or maxillary branches of the trigeminal nerve. The condition first Case described by Ota and Tanino occurs predominantly in Asians with estimated frequency of 0.014% to A 36-year-old African American male, Fitzpatrick 0.034%, but can be found in other ethnicities.1 Skin Type VI, with no significant medical history, Historical therapies for nevus of Ota include surgery, presented for treatment of a 10 Â 16-cm Tanino dermabrasion, electrodesiccation, skin grafting, and Stage III (V1 and V2 distribution) nevus of Ota cryotherapy and are all associated with a significant (Figure 1). The patient was treated with a QSRL, at a risk of dyschromia and scarring.2–5 fluence of 3 to 5 J, spot size 6.5 mm with no greater than 10% overlap between pulses. After 20 treat- The introduction of the theory of selective ment sessions, of which several were partial treat- photothermolysis and subsequent development of ments of the same area of the nevus of Ota over a Q-switched lasers revolutionized the treatment period of 6 years, the lesion was completely cleared.