Governmentofsierraleone
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Gazette No. 6
The Sierra Leone Gazette Published by Authority Vol. CXLVI Thursday, 5th February, 2015 No. 6 G . N . Page CONTENTS NATIONAL ELECTORAL COMMISSION (NEC) G . N . Page 24 Public Service Notices ... ... 29-30 26 Declaration of Results ... 31-33 Office of the President BANK OF SIERRA LEONE 25 Day to be observed as Public Holiday 30 13-- COURT 23 Proforma Balance Sheet 31st January, to 28th November, 2014 respectively 34-44 12 Citation ... ... 30 Freetown. 5th February, 2015 Saccoh, Allieu F. B., Community Health Officer, 1.1.14. Barrie, Hawanatu A., House Officer, 1.11.14. Govt. Notice No. 24 Jalloh, Abdulai T., House Officer, 1.11.14. Kamara, Alusine R., House Officer, 1.11.14. Appointment Kamara, Ibrahim S., Nursing Officer, 1.8.14. Ministry of Defence Kanu, Abu Bakarr., House Officer, 1.11.14. Surrur, Hellen I., Higher Executive Officer, 1.1.15. Koroma, Abu Bakarr, House Officer, 1.11.14. Laggah, Michael, House Officer, 1.11.14. Ministry of Trade and Industry Sesay, Albertina, House Officer, 1.11.14. Bangura, Abdul A., Trade Monitor, 1.12.14. Sesay, Francess M. T., House Officer, 1.1.15. Bundu, Abdul Rahman., Trade Monitor, 1.12.14. Tanga, Wilma F., House Officer, 1.11.14. Kamara, Alusine M., Trade Monitor, 1.12.14. Surrur, Saida R., Higher Executive Officer, 1.1.15. Kamara, Taylor-Emerson., Trade Monitor, 1.12.14. Bundor, Jemba S., State Registered Nurse, 1.9.14. Kanu, Abu Bakarr., Trade Monitor, 1.12.14. Kalokoh, Marian S., State Registered Nurse, 1.9.14. Kargbo, Esheka., Trade Monitor, 1.12.14. -
Sierraleone Local Council Ward Boundary Delimitation Report
NATIONAL ELECTORAL COMMISSION Sierra Leone Local Council Ward Boundary Delimitation Report Volume Two Meets and Bounds April 2008 Table of Contents Preface ii A. Eastern region 1. Kailahun District Council 1 2. Kenema City Council 9 3. Kenema District Council 12 4. Koidu/New Sembehun City Council 22 5. Kono District Council 26 B. Northern Region 1. Makeni City Council 34 2. Bombali District Council 37 3. Kambia District Council 45 4. Koinadugu District Council 51 5. Port Loko District Council 57 6. Tonkolili District Council 66 C. Southern Region 1. Bo City Council 72 2. Bo District Council 75 3. Bonthe Municipal Council 80 4. Bonthe District Council 82 5. Moyamba District Council 86 6. Pujehun District Council 92 D. Western Region 1. Western Area Rural District Council 97 2. Freetown City Council 105 i Preface This part of the report on Electoral Ward Boundaries Delimitation process is a detailed description of each of the 394 Local Council Wards nationwide, comprising of Chiefdoms, Sections, Streets and other prominent features defining ward boundaries. It is the aspect that deals with the legal framework for the approved wards _____________________________ Dr. Christiana A. M Thorpe Chief Electoral Commissioner and Chair ii CONSTITUTIONAL INSTRUMENT No………………………..of 2008 Published: THE LOCAL GOVERNMENT ACT, 2004 (Act No. 1 of 2004) THE KAILAHUN DISTRICT COUNCIL (ESTABLISHMENT OF LOCALITY AND DELIMITATION OF WARDS) Order, 2008 Short title In exercise of the powers conferred upon him by subsection (2) of Section 2 of the Local Government Act, 2004, the President, acting on the recommendation of the Minister of Internal Affairs, Local Government and Rural Development, the Minister of Finance and Economic Development and the National Electoral Commission, hereby makes the following Order:‐ 1. -
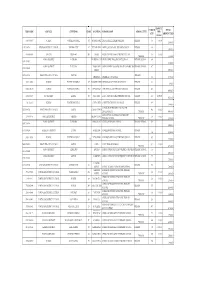
Emis Code Council Chiefdom Ward Location School Name
AMOUNT ENROLM TOTAL EMIS CODE COUNCIL CHIEFDOM WARD LOCATION SCHOOL NAME SCHOOL LEVEL PER ENT AMOUNT PAID CHILD 5103-2-09037 WARDC WATERLOO RURAL 391 ROGBANGBA ABDUL JALIL ACADEMY PRIMARY PRIMARY 369 10,000 3,690,000 1291-2-00714 KENEMA DISTRICT COUNCIL KENEMA CITY 67 FULAWAHUN ABDUL JALIL ISLAMIC PRIMARY SCHOOL PRIMARY 380 3,800,000 4114-2-06856 BO CITY TIKONKO 289 SAMIE ABDUL TAWAB HAIKAL PRIMARY SCHOOL 610 10,000 PRIMARY 6,100,000 KONO DISTRICT TANKORO DOWN BALLOP ABDULAI IBN ABASS PRIMARY SCHOOL PRIMARY SCHOOL 694 1391-2-02007 6,940,000 KONO DISTRICT TANKORO TAMBA ABU ABDULAI IBNU MASSOUD ANSARUL ISLAMIC MISPRIMARY SCHOOL 407 1391-2-02009 STREET 4,070,000 5208-2-10866 FREETOWN CITY COUNCIL WEST III PRIMARY ABERDEEN ABERDEEN MUNICIPAL 366 3,660,000 5103-2-09002 WARDC WATERLOO RURAL 397 KOSSOH TOWN ABIDING GRACE PRIMARY SCHOOL PRIMARY 62 620,000 5103-2-08963 WARDC WATERLOO RURAL 373 BENGUEMA ABNAWEE ISLAMIC PRIMARY SCHOOOL PRIMARY 405 4,050,000 4109-2-06695 BO DISTRICT KAKUA 303 KPETEMA ACEF / MOUNT HORED PRIMARY SCHOOL PRIMARY 411 10,000.00 4,110,000 Not found WARDC WATERLOO RURAL COLE TOWN ACHIEVERS PRIMARY TUTORAGE PRIMARY 388 3,880,000 ACTION FOR CHILDREN AND YOUTH 5205-2-09766 FREETOWN CITY COUNCIL EAST III CALABA TOWN 460 10,000 DEVELOPMENT PRIMARY 4,600,000 ADA GORVIE MEMORIAL PREPARATORY 320401214 BONTHE DISTRICT IMPERRI MORIBA TOWN 320 10,000 PRIMARY SCHOOL PRIMARY 3,200,000 KONO DISTRICT TANKORO BONGALOW ADULLAM PRIMARY SCHOOL PRIMARY SCHOOL 323 1391-2-01954 3,230,000 1109-2-00266 KAILAHUN DISTRICT LUAWA KAILAHUN ADULLAM PRIMARY -

Sierra Leone Year Report 2017
©- Sierra Leone Year Report 2017- Sierra Leone 2017 Year Report & Records of Interest (White necked Picatharte - Picathartes gymnocephalus ©David Monticelli) Momoh B. Sesay 1 ©- Sierra Leone Year Report 2017- INTRODUCTION This is the report of the activities, initiatives and the most interesting bird species that have been recorded in 2017 by myself or by others. The idea of this 39p. birding report - a first of its kind !- is : to give a global image of what has been seen and done in Sierra Leone in 2017; to hopefully open the way to new birding initiatives and field projects. The 2017 birding data have been collected from various internet platforms and sources as well as through contacting people. As a consequence, certain information is most probably missing. The enclosed annotated birdlist gives a fairly good snapshot of last year's available data. It also means you are definitely part of this year report initiative. So please, do contact us : for any further information or help; for giving us datas and feedbacks about your experience and any interesting birding records made around the country. Whatever the way you choose for birding Sierra Leone a lot is still to be done there. It is no terra incognita but for some tricky species, there still is no really reliable site in the country. I hope this first of his kind year report in this - magnificent and safe (!) - country of Sierra Leone will motivate more birdwatchers to come ! Best regards, Momoh B. Sesay I'm working as African Bird Club representative for Sierra Leone & as BirdLife International Field officer attached at Conservation Society of Sierra Leone (CSSL) helping Birdlife International on various projects - among other on the White-Necked Picarthertes at Kambui Hill Forest. -

Climate Change Vulnerability Assessment in Mangrove Regions of Sierra Leone
Climate Change Vulnerability Assessment in Mangrove regions of Sierra Leone Full Report January 2018 This work was conducted under the USAID-funded West Africa Biodiversity and Climate Change (WA BiCC) project. The report is an unabridged version of the official USAID report by the same name published as an Abridged Report in May 2017, and available at http://www.ciesin.columbia.edu/wa-bicc/wa-bicc-ccva-abridged-ff.pdf. The report was prepared by the Center for International Earth Science Information Network (CIESIN) of the Earth Institute of Columbia University. The vulnerability assessment was led by CIESIN under contract with Tetra Tech, and CIESIN also led the analysis and report development. In addition to the CIESIN lead researcher, Sylwia Trzaska, the field research was conducted by a team comprised of representatives from the WA BiCC technical unit in Freetown, Fourah Bay College, Njala University, the National Protected Areas Authority (NPAA), Environmental Protection Agency (EPA), the Ministry of Agriculture, Forestry and Food Security, the Ministry of Lands, Country Planning and Environment, the Ministry of Fisheries and Marine Resources, Conservation Society of Sierra Leone and other stakeholders. The authors of the report are Sylwia Trzaska, Alex de Sherbinin, Paola Kim-Blanco, Valentina Mara, Emilie Schnarr, Malanding Jaiteh, and Pinki Mondal at CIESIN. The team wishes to acknowledge the contributions of Zebedee Njisuh, Aiah Lebbie, Samuel Weekes, George Ganda and Michael Balinga. A full list of field research staff can be found in Annex 5 of this report. Without their hard work and dedication under challenging conditions, this vulnerability assessment would not have been possible. -

The Sierra Leone Gazette Published by Authority
The Sierra Leone Gazette Published by Authority Vol. CXLV Thursday, 25th September, 2014 No. 50 CONTENTS G . N . Page G . N . Page 207 Public Service Notices ... ... 431-432 NATIONAL ELECTORAL COMMISSION (NEC) 211- MINISTRY OF LOCAL GOVERNMENT AND 212 Village Head Election Results ... 435 RURAL DEVELOPMENT 208-210 SUPPLEMENTS 432 205 Bye-Laws for the prevention of Ebola and other diseases ... ... 433-434 Statutory Instrument COURT S.I. No. 6 The Regulation of Wages and industrial Relations 206- Acts 202 High Court Notices .............. 434-436 The Universities (Amendment) Act, 2014 The Polytechnics (Amendment) Act 2014 Freetown 25th September, 2014 Judiciary Department Kanu, Santigie, Messenger, 1.1.13. Kargbo, Saio, Driver, 1.9.13. Govt. Notice No. 207 Ministry of Local Government and Rural Development Appointment Kumawai, John A., Labourer, 1.2.14. Ministry of Agriculture Forestry and Food Security Fofanah, Mariama, Third Grade Clerk, 1.3.14. Nyalla, Mustapha, Senior Monitoring and Evaluation Officer, 1.4.14 Ministry of Mines and Mineral Resources Gaima, Mohamed,Government Mining Engineer, Ministry of Health and Sanitation 1.9.13. Fullah, Veronica, State Enrolled Community Health Kamara, Mohamed M., Geologist, 1.4.13. Nurse, 1.7.13. Swarray, Ahmed, Geologist, 1.4.13. Turay, Emmanuel, Geologist, 1.4.13. Sankoh, Isata Y., State Enrolled Community Health Nurse, 1.4.13. Ministry of Tourism and Culture Bah, Rugiatu, State Enrolled Community Health Nurse, Bundu-Sama, Claude Fatorma, Tourist Guide, 1.1.14. 1.4.13. Wesley, Taylor-John, Tourist Guide, 1.2.14. Allieu, Elizabeth, House Officer, 1.4.14. Confirmation of Appointment Ministry of Internal Affairs Ministry of Agriculture , Forestry and Food Security Conteh, David, Prison Officer, 1.1.14. -

Sierra Leone’S Biodiversity Strategy and Action Plan
Sierra Leone’s Biodiversity Strategy and Action Plan REPUBLIC OF SIERRA LEONE Sierra Leone’s Second National Biodiversity Strategy and Action Plan 2017-2026 Environment Protection Agency Sierra Leone Office of the President The Government of Sierra Leone November 2017 NBSAP 2017 -2026 i Sierra Leone’s Biodiversity Strategy and Action Plan GOVERNMENT OF SIERRA LEONE Environment Protection Agency Sierra Leone, Office of the President Freetown, Sierra Leone Tel: 232-76-677235 Website:www.epa.gov.sl November, 2017 NBSAP 2017-2026 i Sierra Leone’s Biodiversity Strategy and Action Plan REVISED NBSAP (2017-2026) DELIVERY TEAM Project Supervisor Madam Haddijatou Jallow, Executive Chairperson, EPA-SL Project Coordinator Mr Momodu A. Bah, Director, EPA-SL & CBD National Focal Point Project Manager (PM) Dr. Ralph Bona – Consultant Environmentalist Document Compilers Dr. Arnold Okoni-Williams – Consultant Ecologist Dr. Ralph Bona (PM) Document Reviewers Prof A.B. Karim – Consultant (FBC, USL) Mr. Edward Aruna – Consultant (RAP-SL) NBSAP 2017-2026 ii Sierra Leone’s Biodiversity Strategy and Action Plan FOREWORD I have the honour to present the revised National Biodiversity Strategy and Action Plan (NBSAP 2017-2026) for Sierra Leone, which has been developed based on national needs and priorities for the implementation of the Convention on Biological Diversity (CBD) objectives and Aichi Targets. Sierra Leoneans are becoming increasingly aware of the inextricable relationship between our survival and way of life on the one hand, and biodiversity and the environment on the other. Now than ever before, we are aware that our prosperity and economic development, welfare, spirituality, tradition and culture, health and food security can only thrive in a healthy, biodiversity-rich environment. -

2011 Survey of Availability of Modern
2011 Survey of Availability of Modern Contracep•ves and Essen•al Life-Saving Maternal and Reproduc•ve Health Medicines in Service Delivery Points in Sierra Leone: ANALYTICAL REPORT AND TABLES March 2012 UNFPA SIERRA LEONE PREFACE This is the second annual report of the ‘Survey of Modern Contra ceptives and Essential Lifesaving Maternal and Reproductive Health Medicines in Service Delivery Points’ in Sierra Leone. As part of the reporting system of the Global Programme on Reproductive Health Commodity Security (GPRHCS), it generates time series data on reproduct ive health commodity security including the three country level indicators of: (a) Percentage of Service Delivery Points (SDPs) offering at least three modern contraceptive methods; (b) Percentage of SDPs where five selected lifesaving (including th ree essential) lifesaving maternal/reproductive health medicines are available in all facilities providing delivery services, and (c) Percentage of SDPs with ‘no stock-outs’ of modern contraceptives in the last six months prior to the survey (April-September 2011). Government of Sierra Leone and UNFPA appreciate the invaluab le contributions of individuals and institutions towards the success of the 2011 su rvey round in Sierra Leone. We are grateful to the Steering Committee of the surveys on rep roductive health commodity security (RHCS). The co-Chairs of the Reproductive Health Division (RHD) and Parliamentary Committee on Health and Sanitation (MoHS) with th eir membership comprising of stakeholders in the health sector are appreciated f or their oversight functions. We also recognize the technical inputs of the Technical Commit tee that is chaired jointly by the Department of Policy, Planning and Information (DPPI) of Mo HS and Statistics Sierra Leone (SSL). -
Sierra Leone Planning Map 54 69
13°0'0"W 12°30'0"W 12°0'0"W 11°30'0"W 11°0'0"W 10°30'0"W 10°0'0"W 9°30'0"W Gberia Timbako ") 71 72 74 Bafodia ") Sierra Leone Planning Map 54 69 Kabala ") 65 Koinadugu Bendugu N ") 70 ") N " 68 " 0 0 Eastern Province Northern Province Southern Province ' Kamakwie ' 0 ") 0 3 3 ID Chiefdom Name ID Chiefdom Name ID Chiefdom Name ° 53 ° 9 9 Kailahun District Bombali District Bo District 73 G6u4 inea 1 JALAHUN 45 BOMBALI SHEBORA 98 BADJIA 52 KOINADUGU 2 JAWIE 46 MAKARI GBANTI 99 BAGBE 3 MANDU 47 PAKI MASABONG 100 BAGBO 4 UPPER BAMBARA 48 LEIBASGAYAHUN 101 BAOMA 63 5 MALEMA 49 SANDA TENDAREN 102 BUMPE 66 6 DIA 50 MAGBAIAMBA NGOWAHUA 103 GBO 51 50 BOMBALI 7 LUAWA 51 GBANTI KAMARANKA 104 JIAMA-BONGOR 57 8 KISSI TENG 52 SANDA LOKO 105 KAKUA 9 KISSI KAMA 53 SELLA LIMBA 106 KOMBOYA KAMBIA 10 KISSI TONGI 54 TAMBAKKA 107 LUGBU 49 Kambia 75 ") 62 81 Pendembu 67 11 PENGUIA 55 GBENDEMBU NGOWAHUN 108 NIAWA LENGA 60 ") 12 PEJE WEST 56 SAFROKO LIMBA 109 SIELENGA 13 PEJE BONGRE 57 BIRIWA 110 TIKONKO Bumbuna 96 ") 14 YAWEI 111 VALUNIA N 61 N Kambia District " Rokupr " 0 ") 0 ' 55 ' Kenema District 58 MAMBOLO 112 WUNDE 0 0 ° 59 48 95 ° 9 9 15 GORAMA MENDE 59 SAMU 56 42 Bonthe District Mambolo Mange 16 WANDOR 60 GBINLEH-DIXON 113 KPANDA KEMO ") ") 79 80 Makeni 17 SIMBARU 61 MAGBEMA 114 YAWBEKO ") 58 Guinea 18 KANDO LEPPEAMA 62 MASUNGBALA 115 JONG 97 19 DODO 63 TONKO LIMBA 116 BENDUCHA 82 85 46 34 47 40 20 LOWER BAMBARA 64 BRAMAIA 117 NONGOBA BULLOM Port Loko 21 MALEGOHUN Koinadugu District 118 SITTIA ") Foredugu ") 38 45 Magburaka 22 SMALL BO 65 KASSUNKO 119 -

The Sierra Leone Gazette Published by Authority
The Sierra Leone Gazette Published by Authority Vol. CXLVI Thursday, 12th February, 2015 No. 7 CONTENTS G . N . Page BANK OF SIERRA LEONE G . N . Page 27 Public Service Notices ... ... 45-46 13— Office of the President 23 Proforma Balance Sheet 31st January, to 28th November, 2014 respectively 50-60 25 Day to be observed as Public Holiday 46 SUPPLEMENT COURT 12 Citation ... ... 46 Trade Marks T.M. No. 5 NATIONAL ELECTORAL COMMISSION (NEC) Registration of Trade Marks 26 Declaration of Results ... 47-49 Freetown. 12th February, 2015 Saccoh, Allieu F. B., Community Health Officer, 1.1.14. Barrie, Hawanatu A., House Officer, 1.11.14. Govt. Notice No. 27 Jalloh, Abdulai T., House Officer, 1.11.14. Kamara, Alusine R., House Officer, 1.11.14. Appointment Kamara, Ibrahim S., Nursing Officer, 1.8.14. Ministry of Defence Kanu, Abu Bakarr., House Officer, 1.11.14. Surrur, Hellen I., Higher Executive Officer, 1.1.15. Koroma, Abu Bakarr, House Officer, 1.11.14. Laggah, Michael, House Officer, 1.11.14. Ministry of Trade and Industry Sesay, Albertina, House Officer, 1.11.14. Bangura, Abdul A., Trade Monitor, 1.12.14. Sesay, Francess M. T., House Officer, 1.1.15. Bundu, Abdul Rahman., Trade Monitor, 1.12.14. Tanga, Wilma F., House Officer, 1.11.14. Kamara, Alusine M., Trade Monitor, 1.12.14. Surrur, Saida R., Higher Executive Officer, 1.1.15. Kamara, Taylor-Emerson., Trade Monitor, 1.12.14. Bundor, Jemba S., State Registered Nurse, 1.9.14. Kanu, Abu Bakarr., Trade Monitor, 1.12.14. Kalokoh, Marian S., State Registered Nurse, 1.9.14. -

Ebola Response System Strengthening Along Western Area Peninsula Coastline LESSONS LEARNED
Ebola Response System Strengthening along Western Area Peninsula Coastline LESSONS LEARNED Social Mobilization in the Freetown Peninsula during the Ebola Epidemic 2014-2015 Laura Sustersic for Welthungerhilfe Sierra Leone Freetown April 2015 TABLE OF CONTENTS 1 INTRODUCTION .......................................................................................................................... 3 2. BACKGROUND................................................................................................................................ 3 2.1 Official response structure and guidelines for Social Mobilization ................................... 4 3. STATEMENT OF PROBLEM AND PROJECT DESCRIPTION ............................................... 5 3.1 Beneficiaries .......................................................................................................................................... 5 3.2 Map communities and Task Forces ............................................................................................... 7 3.3 Structure and Activities ..................................................................................................................... 8 4. ESTIMATING IMPACTS ............................................................................................................. 10 4.1 Mid-term KAP Study ......................................................................................................................... 10 4.2 Cases and unsafe practices reported by Task Forces .......................................................... -
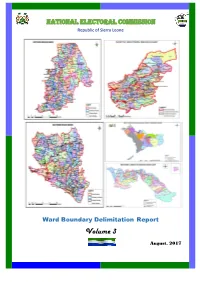
2017 Ward Description, Maps and Population
NATIONAL ELECTORAL COMMISSION Republic of Sierra Leone Ward Boundary Delimitation Report Volume 3 August, 2017 Foreword The National Electoral Commission (NEC) is submitting this report on the delimitation of constituency and ward boundaries in adherence to its constitutional mandate to delimit electoral constituency and ward boundaries, to be done “not less than five years and not more than seven years”; and complying with the timeline as stipulated in the NEC Electoral Calendar (2015-2019). The report is subject to Parliamentary approval, as enshrined in the 1991 Constitution of Sierra Leone (Act No 6 of 1991); which inter alia states delimitation of electoral boundaries to be done by NEC, while Section 38 (1) empowers the Commission to divide the country into constituencies for the purpose of electing Members of Parliament (MPs) using Single Member First- Past –the Post (FPTP) system. The Local Government Act of 2004, Part 1 –preliminary, assigns the task of drawing wards to NEC; while the Public Elections Act, 2012 (Section 14, sub-sections 1 &2) forms the legal basis for the allocation of council seats and delimitation of wards in Sierra Leone. The Commission appreciates the level of technical assistance, collaboration and cooperation it received from Statistics Sierra Leone (SSL), the Boundary Delimitation Technical Committee (BDTC), the Boundary Delimitation Monitoring Committee (BDMC), donor partners, line Ministries, Departments and Agencies and other key actors in the boundary delimitation exercise. The hiring of a Consultant, Dr Lisa Handley, an internationally renowned Boundary delimitation expert, added credence and credibility to the process as she provided professional advice which assisted in maintaining international standards and best practices.