African Potato)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Biogeography of the Monocotyledon Astelioid Clade (Asparagales): a History of Long-Distance Dispersal and Diversification with Emerging Habitats
Zurich Open Repository and Archive University of Zurich Main Library Strickhofstrasse 39 CH-8057 Zurich www.zora.uzh.ch Year: 2021 Biogeography of the monocotyledon astelioid clade (Asparagales): A history of long-distance dispersal and diversification with emerging habitats Birch, Joanne L ; Kocyan, Alexander Abstract: The astelioid families (Asteliaceae, Blandfordiaceae, Boryaceae, Hypoxidaceae, and Lanari- aceae) have centers of diversity in Australasia and temperate Africa, with secondary centers of diversity in Afromontane Africa, Asia, and Pacific Islands. The global distribution of these families makes this an excellent lineage to test if current distribution patterns are the result of vicariance or long-distance dispersal and to evaluate the roles of tertiary climatic and geological drivers in lineage diversification. Sequence data were generated from five chloroplast regions (petL-psbE, rbcL, rps16-trnK, trnL-trnLF, trnS-trnSG) for 104 ingroup species sampled across global diversity. The astelioid phylogeny was inferred using maximum parsimony, maximum likelihood, and Bayesian inference methods. Divergence dates were estimated with a relaxed clock applied in BEAST. Ancestral ranges were reconstructed in ’BioGeoBEARS’ applying the corrected Akaike information criterion to test for the best-fit biogeographic model. Diver- sification rates were estimated in Bayesian Analysis of Macroevolutionary Mixtures [BAMM]. Astelioid relationships were inferred as Boryaceae(Blandfordiaceae(Asteliaceae(Hypoxidaceae plus Lanariaceae))). The crown astelioid node was dated to the Late Cretaceous (75.2 million years; 95% highest posterior densities interval 61.0-90.0 million years) with an inferred Eastern Gondwanan origin. However, aste- lioid speciation events have not been shaped by Gondwanan vicariance. Rather long-distance dispersal since the Eocene is inferred to account for current distributions. -

Redalyc.HYPOXIS COLLICULATA (HYPOXIDACEAE)
Acta Botánica Mexicana ISSN: 0187-7151 [email protected] Instituto de Ecología, A.C. México Sánchez-Ken, J. Gabriel HYPOXIS COLLICULATA (HYPOXIDACEAE), A NEW SPECIES FROM MEXICO AND A KEY TO THE AMERICAN SPECIES WITH BLACK SEEDS Acta Botánica Mexicana, núm. 92, 2010, pp. 1-9 Instituto de Ecología, A.C. Pátzcuaro, México Available in: http://www.redalyc.org/articulo.oa?id=57415475001 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative Acta Botanica Mexicana 92: 1-9 (2010) HYPOXIS COLLICULATA (HYPOXIDACEAE), A NEW SPECIES FROM MEXICO AND A KEY TO THE AMERICAN SPECIES WITH BLACK SEEDS J. GABRIEL SÁNCHEZ -KEN Universidad Nacional Autónoma de México, Instituto de Biología, Departamento de Botánica, 04510 México, D.F. México. [email protected] ABSTRACT A new species, Hypoxis colliculata from Oaxaca and Chiapas, México is presented here. It belongs to the group with black seeds and is separated from the other species by the colliculate sculpturing of the seeds. Key words: black seeds, colliculate, Chiapas, Hypoxidaceae, Hypoxis colliculata, Mexico, Oaxaca, ornamentation. RESUMEN Se propone como nueva a Hypoxis colliculata, planta de Oaxaca y Chiapas, México. La especie se separa de las otras del grupo caracterizado por semillas negras en la ornamentación bulada de estas últimas. Palabras clave: bulada, Chiapas, Hypoxidaceae, Hypoxis colliculata, México, Oaxaca, ornamentación, semillas negras. The Hypoxidaceae R. Br. are a small family within the order Asparagales and together with other small families conform the sister group to the Orchidaceae, ba- sed on molecular and morphological data (Dahlgren et al., 1985; Rudall et al., 1998; Anónimo, 2003; Davis et al., 2004). -

Phylogeny, Genome Size, and Chromosome Evolution of Asparagales J
Aliso: A Journal of Systematic and Evolutionary Botany Volume 22 | Issue 1 Article 24 2006 Phylogeny, Genome Size, and Chromosome Evolution of Asparagales J. Chris Pires University of Wisconsin-Madison; University of Missouri Ivan J. Maureira University of Wisconsin-Madison Thomas J. Givnish University of Wisconsin-Madison Kenneth J. Systma University of Wisconsin-Madison Ole Seberg University of Copenhagen; Natural History Musem of Denmark See next page for additional authors Follow this and additional works at: http://scholarship.claremont.edu/aliso Part of the Botany Commons Recommended Citation Pires, J. Chris; Maureira, Ivan J.; Givnish, Thomas J.; Systma, Kenneth J.; Seberg, Ole; Peterson, Gitte; Davis, Jerrold I.; Stevenson, Dennis W.; Rudall, Paula J.; Fay, Michael F.; and Chase, Mark W. (2006) "Phylogeny, Genome Size, and Chromosome Evolution of Asparagales," Aliso: A Journal of Systematic and Evolutionary Botany: Vol. 22: Iss. 1, Article 24. Available at: http://scholarship.claremont.edu/aliso/vol22/iss1/24 Phylogeny, Genome Size, and Chromosome Evolution of Asparagales Authors J. Chris Pires, Ivan J. Maureira, Thomas J. Givnish, Kenneth J. Systma, Ole Seberg, Gitte Peterson, Jerrold I. Davis, Dennis W. Stevenson, Paula J. Rudall, Michael F. Fay, and Mark W. Chase This article is available in Aliso: A Journal of Systematic and Evolutionary Botany: http://scholarship.claremont.edu/aliso/vol22/iss1/ 24 Asparagales ~£~2COTSgy and Evolution Excluding Poales Aliso 22, pp. 287-304 © 2006, Rancho Santa Ana Botanic Garden PHYLOGENY, GENOME SIZE, AND CHROMOSOME EVOLUTION OF ASPARAGALES 1 7 8 1 3 9 J. CHRIS PIRES, • • IVAN J. MAUREIRA, THOMAS J. GIVNISH, 2 KENNETH J. SYTSMA, 2 OLE SEBERG, · 9 4 6 GITTE PETERSEN, 3· JERROLD I DAVIS, DENNIS W. -

On the Flora of Australia
L'IBRARY'OF THE GRAY HERBARIUM HARVARD UNIVERSITY. BOUGHT. THE FLORA OF AUSTRALIA, ITS ORIGIN, AFFINITIES, AND DISTRIBUTION; BEING AN TO THE FLORA OF TASMANIA. BY JOSEPH DALTON HOOKER, M.D., F.R.S., L.S., & G.S.; LATE BOTANIST TO THE ANTARCTIC EXPEDITION. LONDON : LOVELL REEVE, HENRIETTA STREET, COVENT GARDEN. r^/f'ORElGN&ENGLISH' <^ . 1859. i^\BOOKSELLERS^.- PR 2G 1.912 Gray Herbarium Harvard University ON THE FLORA OF AUSTRALIA ITS ORIGIN, AFFINITIES, AND DISTRIBUTION. I I / ON THE FLORA OF AUSTRALIA, ITS ORIGIN, AFFINITIES, AND DISTRIBUTION; BEIKG AN TO THE FLORA OF TASMANIA. BY JOSEPH DALTON HOOKER, M.D., F.R.S., L.S., & G.S.; LATE BOTANIST TO THE ANTARCTIC EXPEDITION. Reprinted from the JJotany of the Antarctic Expedition, Part III., Flora of Tasmania, Vol. I. LONDON : LOVELL REEVE, HENRIETTA STREET, COVENT GARDEN. 1859. PRINTED BY JOHN EDWARD TAYLOR, LITTLE QUEEN STREET, LINCOLN'S INN FIELDS. CONTENTS OF THE INTRODUCTORY ESSAY. § i. Preliminary Remarks. PAGE Sources of Information, published and unpublished, materials, collections, etc i Object of arranging them to discuss the Origin, Peculiarities, and Distribution of the Vegetation of Australia, and to regard them in relation to the views of Darwin and others, on the Creation of Species .... iii^ § 2. On the General Phenomena of Variation in the Vegetable Kingdom. All plants more or less variable ; rate, extent, and nature of variability ; differences of amount and degree in different natural groups of plants v Parallelism of features of variability in different groups of individuals (varieties, species, genera, etc.), and in wild and cultivated plants vii Variation a centrifugal force ; the tendency in the progeny of varieties being to depart further from their original types, not to revert to them viii Effects of cross-impregnation and hybridization ultimately favourable to permanence of specific character x Darwin's Theory of Natural Selection ; — its effects on variable organisms under varying conditions is to give a temporary stability to races, species, genera, etc xi § 3. -
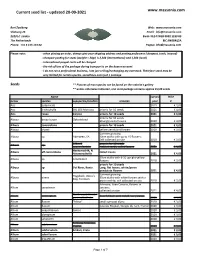
Current Seed List - Updated 20-09-2021
Current seed list - updated 20-09-2021 www.massonia.com Bert Zaalberg Web: www.massonia.com Vlietweg 26 Email: [email protected] 2323 LC Leiden Bank: NL14 INGB 0002 1233 89 The Netherlands BIC: INGBNL2A Phone: +31 6 155 133 64 Paypal: [email protected] Please note: - when placing an order, always give your shipping address and posting preference (cheapest, track, insured) - cheapest posting for seeds (weight < 20gr) is 2,50€ (international) and 1,50€ (local) - International paypal costs will be charged - the risk of loss of the package during transport is on the buyers account - I do not run a professional business, I am just selling/exchanging my overstock. Therefore stock may be very limited for certain species, sometimes even just 1 package Seeds ** Pictures of most species can be found on the website's gallery ** unless otherwise indicated, one seed-package contains approx 15/20 seeds Name harvest Price Genus species supspecies/location remarks year € Acis autumnalis 2019 € 3,00 Acis trichophylla SBL 603 Morocco price is for 10 seeds 2021 € 4,00 Acis rosea Corsica price is for 10 seeds 2021 € 4,00 Albuca bruce-bayeri Ockertskraal price is for 10 seeds Strongly coiled leaves 2020 € 4,00 Albuca concordiana price is for 10 seeds 2021 € 4,00 Albuca shawii yellow pendulant flowers 2019 € 3,00 Summer growing Albuca sp. Aberdeen, SA 20cm stalks with up to 15 flowers; Self collected on site 2020 € 3,00 27km S price is for 10 seeds Albuca sp. Loeriesfontein Habitat seeds, coiled leaves 2021 € 4,00 Albuca aff concordiana Hantamsdrift, N coiled leaves Nieuwoudtville 2021 € 4,00 30cm stalks with 6-10 upright yellow Albuca sp. -

Phylogenetic Relationships of Monocots Based on the Highly Informative Plastid Gene Ndhf Thomas J
Aliso: A Journal of Systematic and Evolutionary Botany Volume 22 | Issue 1 Article 4 2006 Phylogenetic Relationships of Monocots Based on the Highly Informative Plastid Gene ndhF Thomas J. Givnish University of Wisconsin-Madison J. Chris Pires University of Wisconsin-Madison; University of Missouri Sean W. Graham University of British Columbia Marc A. McPherson University of Alberta; Duke University Linda M. Prince Rancho Santa Ana Botanic Gardens See next page for additional authors Follow this and additional works at: http://scholarship.claremont.edu/aliso Part of the Botany Commons Recommended Citation Givnish, Thomas J.; Pires, J. Chris; Graham, Sean W.; McPherson, Marc A.; Prince, Linda M.; Patterson, Thomas B.; Rai, Hardeep S.; Roalson, Eric H.; Evans, Timothy M.; Hahn, William J.; Millam, Kendra C.; Meerow, Alan W.; Molvray, Mia; Kores, Paul J.; O'Brien, Heath W.; Hall, Jocelyn C.; Kress, W. John; and Sytsma, Kenneth J. (2006) "Phylogenetic Relationships of Monocots Based on the Highly Informative Plastid Gene ndhF," Aliso: A Journal of Systematic and Evolutionary Botany: Vol. 22: Iss. 1, Article 4. Available at: http://scholarship.claremont.edu/aliso/vol22/iss1/4 Phylogenetic Relationships of Monocots Based on the Highly Informative Plastid Gene ndhF Authors Thomas J. Givnish, J. Chris Pires, Sean W. Graham, Marc A. McPherson, Linda M. Prince, Thomas B. Patterson, Hardeep S. Rai, Eric H. Roalson, Timothy M. Evans, William J. Hahn, Kendra C. Millam, Alan W. Meerow, Mia Molvray, Paul J. Kores, Heath W. O'Brien, Jocelyn C. Hall, W. John Kress, and Kenneth J. Sytsma This article is available in Aliso: A Journal of Systematic and Evolutionary Botany: http://scholarship.claremont.edu/aliso/vol22/iss1/ 4 Aliso 22, pp. -

Including Hypoxidaceae)
Flora Malesiana ser. I, Vol. 11 (2) (1993) 353-373 Amaryllidaceae (including Hypoxidaceae) D.J.L. Geerinck Brussels, Belgium) Perennial herbs with bulbs, tubers or rhizomes. Leaves simple, with parallel nerves. In- terminal in umbels florescences or axillary, cymes, spikes or (in Amaryllidoideae), or flowers solitary, bracteateand often with one or few spathes (in Amaryllidoideae). Flowers sometimes in 2 free bisexual, actinomorphic or zygomorphic, marcescent. Tepals whorls, sometimes with Stamens free or united into a tube, a conspicuous corona. 6, or some- times united into a false corona, often inserted at the mouth of the perigone-tube; anthers often versatile. 3-celled with basifixed, dorsifixed or medifixed, Ovary inferior, axillary placentas; ovules 1 to numerous per cell. Fruit capsular, dehiscing either loculicidally or irregularly, or fruit a berry. Seeds globose or flattened, sometimes winged. Distribution— Cosmopolitan, with c. 80 genera and around 1000 species. In Malesia only 6 genera are indigenous or naturalized, but many others are cultivatedin botanic and private gardens (see the list on p. 371). Taxonomy — The family is treated here in a broad sense, comprising the genera with an inferior ovary, i.e. excluding the Allioideae(= Alliaceae), which are characterized by a superior ovary. In Malesia there are no indigenous species of the latter family, which is treated elsewhere in this instalment (p. 375). The Agavoideae (partly with an inferiorovary and partly with a superior one) are also excluded. The family Agavaceae has one indigenous genus in Malesia (Dracaena, includ- ing Pleomele). In the Amaryllidaceae two subfamilies are hererecognized which are often considered to be distinctfamilies: the Amaryllidoideae (= Amaryllidaceae s. -

Systematic Studies in the Family Liliaceae from Bangladesh
Bangladesh J. Plant Taxon. 15(2): 115-128, 2008 (December) © 2008 Bangladesh Association of Plant Taxonomists SYSTEMATIC STUDIES IN THE FAMILY LILIACEAE FROM BANGLADESH 1 SUMONA AFROZ AND MD. ABUL HASSAN Department of Botany, University of Dhaka, Dhaka 1000, Bangladesh Keywords: Liliaceae, Systematic studies, Bangladesh Abstract The family Liliaceae A.L. de Jussieu has been revised for Bangladesh and a total of 34 species with one variant under 16 genera have been recorded. Artificial dichotomous keys to the genera and species have been given. Descriptions have been provided for each taxon, and local names, flowering and fruiting periods have been added wherever available. Out of 34 species, 16 species are native/naturalized and 18 species, including 1 variant, are exotic. Four genera, ten species and one variant have been documented for the first time in Bangladesh. Introduction Liliaceae A.L. de Jussieu, the Lily family, is a moderately large family consisting of about 280 genera and nearly 4000 species, widespread throughout the world, but most abundant and varied in fairly dry, temperate to subtropical regions. The family is characterized by the following diagnostic characters: i) Perennial or annual herbs, rarely shrubs, with starchy rhizome, bulb or corm; ii) Leaves simple, alternate or less often opposite or whorled, often all basal; iii) Flowers in a raceme, spike, panicle or involucrate cymose umbel, sometimes solitary or paired in the axils of the leaves; iv) Tepals 6-8, usually in 2 similar petaloid cycles, stamens usually as many as the tepals; v) Carpels 3 (rarely 2 or 4), united, ovary superior or inferior with axile or basal placentation; vi) Fruit a loculicidal or septicidal capsule, less often a berry, seeds often flat (Cronquist 1981). -

BULLETIN of the AMERICAN ROCK GARDEN SOCIETY
BULLETIN of the AMERICAN ROCK GARDEN SOCIETY Vol. 22 January, 1964 No. 1 MARY BYMAN AND HER GARDEN — Olgcc Johnson 1 LEWISIAS OF THE SISKIYOUS — Marcel Le Piniec ........ 4 THREE ACQUISITIONS FROM THE NORTH CAROLINA PINE BARRENS — Leonard /. Uttal .... 6 FLOWERS ON BARE-FACED ROCKS — Leonard Wiley 7 BOOK REVIEW — Florence Free 9 HYPOXIS HIRSUTA — Elizabeth L. Freeman 10 FLOWERLESS SEPTEMBER IN THE HIGH SIERRA Shirley Backman 12 INTERCHANGE OVERFLOW 14 SOME SHADE-LOVING NATIVE ROCK GARDEN PLANTS PART II —.Robert H. Gaede 16 ERIGERON AUREUS—AM.S 18 NOTES FROM THE NORTHWEST — Sallie D. Allen 20 WELCOME! NEW MEMBERS 23 THE TRAIL OF THE WHITE IRIS — Mrs. Raleigh Harold .... 23 A FLORAL EMBLEM 25 NOTES ON COLD FRAME SASHES — Richard Langfelder .. 26 INTERCHANGE 27 OMNIUM-GATHERUM 29 DIRECTORATE BULLETIN Editor Emeritus DR. EDGAR T. WHERRY, University of Pennsylvania, Philadelphia 4, Pa. Editor ALBERT M. SUTTON 9608 26th Ave. N. W., Seattle, Washington 98107 AMERICAN ROCK GARDEN SOCIETY President HAROLD EPSTEIN, Larchmont, N. Y. Secretary E. L. TOTTEN, Hendersonville, N. C. Treasurer - ALEX D. REID, Mountain Lakes, N. J. Vice-Presidents LEONARD J. BUCK MRS. HARRY HAYWARD MRS. COULTER STEWART FREDERICK E. LANDMANN BRIAN O. MULLIGAN Directors— Term Expires 1964 MRS. DOROTHY E. HANSELL MISS ALIDA LIVINGSTON MRS. MORTIMER FOX Terra Expires 1965 DR. E. T. WHERRY MR. KURT W. BAASCH MR. BERNARD HARKNESS Term Expires 1966 Miss ALYS SUTCLIFFE MR. H. LINCOLN FOSTER DR. A. R. KRUCKEBERG Director of Seed Exchange BERNARD HARKNESS 5 Castle Park, Rochester 20, N. Y. REGIONAL CHAIRMEN Northwestern SCOTT A. MCCLANAHAN, 2643 38th Ave., W. -

Diversity and Evolution of Monocots
Lilioids - petaloid monocots 4 main groups: Diversity and Evolution • Acorales - sister to all monocots • Alismatids of Monocots – inc. Aroids - jack in the pulpit • Lilioids (lilies, orchids, yams) – grade, non-monophyletic . petaloid monocots . – petaloid • Commelinids – Arecales – palms – Commelinales – spiderwort – Zingiberales –banana – Poales – pineapple – grasses & sedges Lilioids - petaloid monocots Lilioids - petaloid monocots The lilioid monocots represent five The lilioid monocots represent five orders and contain most of the orders and contain most of the showy monocots such as lilies, showy monocots such as lilies, tulips, blue flags, and orchids tulips, blue flags, and orchids Majority are defined by 6 features: Majority are defined by 6 features: 1. Terrestrial/epiphytes: plants 2. Geophytes: herbaceous above typically not aquatic ground with below ground modified perennial stems: bulbs, corms, rhizomes, tubers 1 Lilioids - petaloid monocots Lilioids - petaloid monocots The lilioid monocots represent five orders and contain most of the showy monocots such as lilies, tulips, blue flags, and orchids Majority are defined by 6 features: 3. Leaves without petiole: leaf . thus common in two biomes blade typically broader and • temperate forest understory attached directly to stem without (low light, over-winter) petiole • Mediterranean (arid summer, cool wet winter) Lilioids - petaloid monocots Lilioids - petaloid monocots The lilioid monocots represent five The lilioid monocots represent five orders and contain most of the orders and contain most of the showy monocots such as lilies, showy monocots such as lilies, tulips, blue flags, and orchids tulips, blue flags, and orchids Majority are defined by 6 features: Majority are defined by 6 features: 4. Tepals: showy perianth in 2 5. -

Hypoxis (Hypoxidaceae) in Southern Africa: Taxonomic Notes ⁎ Y
South African Journal of Botany 73 (2007) 360–365 www.elsevier.com/locate/sajb Hypoxis (Hypoxidaceae) in southern Africa: Taxonomic notes ⁎ Y. Singh South African National Biodiversity Institute, KwaZulu-Natal Herbarium, Botanic Gardens Road, Durban 4001, South Africa Received 20 July 2006; received in revised form 31 January 2007; accepted 2 February 2007 Abstract Several Hypoxis species and infraspecific taxa in southern Africa were found to be conspecific with the taxa described earlier. In this paper, thirteen validly published names are reduced to synonyms. Nine currently recognized taxa out of about 30 species in the Flora of southern Africa region are listed together with their new synonyms and important literature, and a brief discussion is given for each change in name status. The nine taxa discussed (with synonyms) are: Hypoxis angustifolia var. buchananii Baker (= H. obliqua var. woodii (Baker) Nel); Hypoxis argentea var. sericea Baker (= H. argentea var. flaccida Baker, H. dinteri Nel); H. colchicifolia Baker (= H. distachya Nel, H. gilgiana Nel); H. floccosa Baker (= H. ecklonii Nel); H. hemerocallidea Fisch., C.A.Mey. & Ave-Lall. (= H. obconica Nel, H. patula Nel, H. rooperi var. forbesii Baker); H. longifolia Baker ex Hook.f. (= H. longifolia var. thunbergii Baker); H. obtusa Ker Gawl. (= H. obtusa var. chrysotricha Nel); H. rigidula var. rigidula Baker (= H. cordata Nel); H. rigidula var. pilosissima Baker (= H. arnottii Baker). © 2007 SAAB. Published by Elsevier B.V. All rights reserved. Keywords: Hypoxis; Hypoxidaceae; Nomenclature; Southern Africa; Synonymy; Taxonomy Hypoxis L. is the largest genus of the Hypoxidaceae, a family inordinate taxonomic significance to two characters, namely of ‘lower’ Asparagales (Nordal, 1998; Fay et al., 2000). -

Sterols and Sterolins in Hypoxis Hemerocallidea (African Potato)
322 South African Journal of Science 104, July/August 2008 Research Letters corm. Furthermore, the term African potato is also, and confus- Sterols and sterolins in ingly, attributed to another plant, Plectrantus esculentus. The name Hypoxis will therefore be used throughout this text when Hypoxis hemerocallidea referring to the AP. Extracts of the corms have been ingested by (African potato) man as a dietary supplement and for a diversity of ailments.1–6 In recent years, the increasing interest in functional foods and the use of phytosterols, their glycosides (sterolins) and steryl esters a b Vipin D.P. Nair and I. Kanfer * (>2 g/day) for reducing serum cholesterol and increasing immunity has resulted in these compounds regaining consider- able attention.1 There are many herbal formulations containing sterols for this reason, most of which have been fortified with Commercially available health supplements and herbal remedies additional amounts of free sterols, stanols and sterolins. Com- containing sterols and sterolins, either from African potato mercially available health supplements and herbal remedies (Hypoxis hemerocallidea) alone, or whether enriched with sterols containing sterols and sterolins as well as Hypoxis, alone or and sterolins, are claimed to be efficacious in the treatment of a enriched with sterols and sterolins, are claimed to be efficacious variety of ailments. Sterols and sterolins in African potato are for a variety of ailments. In particular, purported sterol and purported to be the relevant constituents that are required for sterolin content in products containing Hypoxis is identified to the therapeutic claims of such products. A patent describing the be the important feature for the therapeutic claims of these extraction of sterolins from African potato plant material has products.