Variations in the Circumflex Branches of the Profunda Femoris Artery - a Cadaveric Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A STUDY of ANAMOLOUS ORIGIN of GLUTEAL ARTERIES IJCRR Section: Healthcare Sci
Research Article A STUDY OF ANAMOLOUS ORIGIN OF GLUTEAL ARTERIES IJCRR Section: Healthcare Sci. Journal Impact Factor Amudalapalli Siva Narayana1, M. Pramila Padmini2 4.016 1Tutor, Department of Anatomy, Gitam Institute of Medical Sciences Visakhapatnam, Andhrapradesh, India; 2Assistant Professor, Department of Anatomy, Gitam Institute of Medical Sciences, Visakhapatnam, Andhrapradesh, India. ABSTRACT Aim: The present study has been taken up to observe the branching pattern of internal iliac artery and its importance for the clinicians in their respective fields. Methodology: 45 pelvic halves were studied from dissected cadavers. The branches of gluteal arteries were traced carefully by separating the connective tissue surrounding the arteries. Result: In 4 cadavers, inferior gluteal artery was given off in the gluteal region, in 1 case it is given off from posterior division of internal iliac artery. In 1 case superior gluteal arose in common with internal pudendal artery. Conclusion: Vascular variations in the gluteal region are important for surgeons and anatomists. Key Words: Internal iliac artery, Gluteal arteries, Pelvic region, Internal pudendal artery INTRODUCTION The tributaries of internal iliac vein along with the main trunk were discarded to visualize the branches of IIA. Con- Each internal iliac artery is about 4 cm long and begins at the nective tissue surrounding the IIA was cleared. Parietal and common iliac bifurcation level with the intervertebral disc visceral branches were traced. Some of the branches of between L5 and S1 vertebrae and anterior to the sacroiliac IIA were traced till their exit from the pelvic cavity and are joint. As it passes downward across the brim of the pelvis it called parietal branches. -

The Deep Femoral Artery and Branching Variations: a Case Report Arteria Profunda Femoris Ve Dallarının Varyasyonu: Olgu Sunumu
Cumhuriyet Tıp Dergisi Cumhuriyet Tıp Derg 2009; 31: 279-282 Cumhuriyet Medical Journal Cumhuriyet Med J 2009; 31: 279-282 The deep femoral artery and branching variations: a case report Arteria profunda femoris ve dallarının varyasyonu: olgu sunumu Vedat Sabancıoğulları, Mehmet İlkay Koşar, Ekrem Ölçü, Mehmet Çimen Department of Anatomy (Assist. Prof. V. Sabancıoğulları, MD; Assist. Prof. M. İ. Koşar, MD; Prof. M. Çimen, PhD), Cumhuriyet University School of Medicine, TR-58140, Sivas; and Department of Radiology (E. Ölçü, MD, Specialist in Radiology) Afşin State Hospital, TR-46500 Kahramanmaraş Abstract The deep femoral artery is the major branch of the femoral artery. Its branches and branching show various variations. For this reason, an extensive knowledge about the anatomy of the deep femoral artery is indeed important in vascular reconstructive surgery involving the groin. In this investigation, a case with variations of the deep femoral artery origin and branching has been presented. The case was a 45-year old male cadaver and the arterial variation was noted during routine dissection. The right and left origins of the deep femoral artery varied. When the midpoint of the inguinal ligament was taken as a reference, the right artery originated at 5.58 cm and the left artery at 2.22 cm. In the left, the ascending branch and transverse branch of the lateral circumflex femoral artery originated. At a joint root and the descending branch originated directly at the deep femoral artery. Also in the left, it was observed that there were eight perforating arteries. Keywords: Deep femoral artery, anatomic variation, cadaver Özet Arteria profunda femoris, arteria femoralis’in uyluğu besleyen en büyük dalıdır. -

Reconstructive
RECONSTRUCTIVE Angiosomes of the Foot and Ankle and Clinical Implications for Limb Salvage: Reconstruction, Incisions, and Revascularization Christopher E. Attinger, Background: Ian Taylor introduced the angiosome concept, separating the M.D. body into distinct three-dimensional blocks of tissue fed by source arteries. Karen Kim Evans, M.D. Understanding the angiosomes of the foot and ankle and the interaction among Erwin Bulan, M.D. their source arteries is clinically useful in surgery of the foot and ankle, especially Peter Blume, D.P.M. in the presence of peripheral vascular disease. Paul Cooper, M.D. Methods: In 50 cadaver dissections of the lower extremity, arteries were injected Washington, D.C.; New Haven, with methyl methacrylate in different colors and dissected. Preoperatively, each Conn.; and Millburn, N.J. reconstructive patient’s vascular anatomy was routinely analyzed using a Dopp- ler instrument and the results were evaluated. Results: There are six angiosomes of the foot and ankle originating from the three main arteries and their branches to the foot and ankle. The three branches of the posterior tibial artery each supply distinct portions of the plantar foot. The two branches of the peroneal artery supply the anterolateral portion of the ankle and rear foot. The anterior tibial artery supplies the anterior ankle, and its continuation, the dorsalis pedis artery, supplies the dorsum of the foot. Blood flow to the foot and ankle is redundant, because the three major arteries feeding the foot have multiple arterial-arterial connections. By selectively performing a Doppler examination of these connections, it is possible to quickly map the existing vascular tree and the direction of flow. -

Femoral Artery, Profunda Femoris Artery, Lateral Circumflex Femoral Artery, Medial Circumflex Artery, Femoral Triangle
Basic Sciences of Medicine 2016, 5(1): 5-7 DOI: 10.5923/j.medicine.20160501.02 Anomalous Configuration of Medial and Lateral Circumflex Femoral Arteries Rajani Singh Department of Anatomy AIIMS Rishikesh, Rishikesh, India Abstract Normally profunda femoris artery arises from femoral artery below the inguinal ligament. Profunda femoris artery gives rise to lateral circumflex artery laterally and medial circumflex artery medially. But abnormal configuration of profunda femoris artery and its branches was observed in two cases in present study during dissection of lower limbs for teaching purpose in the department of Anatomy AIIMS Rishikesh, India. In one case, femoral artery trifurcated into medial circumflex, lateral circumflex and profunda femoris arteries. This finding is rare. In another case, common trunk arose from femoral artery which descended for 2.5 cm and gave medial circumflex artery. This common trunk descended further for 1 cm and bifurcated into lateral circumflex and profunda femoris arteries. This finding is new and unique and hence the case is reported. Knowledge of these variations will be of utmost importance to surgeons carrying out surgical procedures around the femoral triangle, to radiologists to avoid misinterpretation of radiographs and to anatomists for new and rare variants. Keywords Femoral artery, Profunda femoris artery, Lateral circumflex femoral artery, Medial circumflex artery, Femoral triangle 1. Introduction 2. Case Report Femoral artery (FA) is continuation of external iliac artery. Femoral triangles of two female cadavers embalmed in Profunda femoris artery (PFA) originates from posterolateral 10% formalin were dissected for teaching undergraduate aspect of femoral artery about 3.5 cm below the inguinal medical students in the department of anatomy AIIMS ligament (IL) in femoral triangle [1]. -

Pdf Manual (964.7Kb)
MD-17 , CONTENTS THE URINARY SYSTEM 4 THE REPRODUCTIVE SYSTEM 5 The Scrotum The Testis The Epididylnis The Ductus Deferens The Ejaculatory Duct The Seminal Vesicle The Spermatic Cord The Penis The Prostate Gland THE INGUINAL CANAL l) HERNIAS FURTIlER READING 10 MODEL KEY 1I Human Male Pelvis This life-size model shows the viscera and structures which form the urogenital system and some of the related anatomy such as the sig moid colon and rectum. The vascular supply to the viscera and support ing tissue is demonstrated, as well as that portion of the vascular system which continues into the lower extremity. The model is divided into right and left portions. The right portion shows a midsagittal section of the pelvic structures. The left represents a similar section, but the dissection is deeper. Two pieces are remov able on the left side; one piece includes the bladder, prostate, and semi nal vesicles, and the other includes the penis, left testicle, and scrotum. When all portions are removed, a deeper view of these structures and a deeper dissection of the pelvis can be seen. THE URINARY SYSTEM The portion of the urinary system shown depicts the ureter from the level of the 5th lumbar vertebra, where it passes the common iliac ar tery near the bifurcation of thi s artery into the external and internal iliac arteries. The ureter then passes toward the posterior portion of the bladder, beneath the vas deferens, and opens through the wall of the blad der at one cranial corner of the trigone on the bladder's interior. -

Vascular Anatomy of the Lower Limbs Anatomy Team 434
Vascular Anatomy of the Lower Limbs Anatomy Team 434 Color Index: If you have any complaint or ▪ Important Points suggestion please don’t ▪ Helping notes hesitate to contact us on: [email protected] ▪ Explanation OBJECTIVES ● List the main arteries of the lower limb. ● Describe their origin, course distribution & branches ● List the main arterial anastomosis ● List the sites where you feel the arterial pulse. ● Differentiate the veins of LL into superficial & deep ● Describe their origin, course & termination and tributaries ORIGIN FEMORAL ARTERY It is the main Arterial supply of the lower limb it is the LOCATION continuation of the external Behind the inguinal ligament in the midway iliac artery between Superior anterior iliac spine and the pubic symphysis . It ends at the opening of adductor magnus as the popliteal artery. It descends vertically towards the adductor RELATIONS tubercle -It terminates by passing through the adductor hiatus (in adductor magnus) and entering the popliteal space as the Popliteal artery. - In the front of hip joint→femoral artery - artery and vien inside the femoral sheath but the nerve outside the sheath - In the back of hip joint→siatic nearve - artery , vien and nerve inside femoral triangle . FEMORAL VEIN & ARTETY : ( See Figure 1 ) 1- At the inguinal ligament : it is located medially to the femoral artery 2- At the apex of the femoral triangle : it is located posteriorly to the femoral artery 3- At the opening of the adductor magnus : it is located laterally to the femoral artery 1 BRANCHES OF THE FEMORAL ARTERY(1) : ( See Figure 2 ) 2 3 1- Superficial Epigastric 2- Superficial Circumflex iliac 3- Superficial external pudendal 4- Deep external pudendal Figure Figure 1 5- Profunda femoris —(Deep artery of thigh) 2 Cannulation of Femoral Artery : It is used for left cardiac angiography. -

Part Innervation Blood Supply Venous Drainage
sheet PART INNERVATION BLOOD SUPPLY VENOUS DRAINAGE LYMPH DRAINAGE Roof: greater palatine & nasopalatine Mouth nerves (maxillary N.) Floor: lingual nerve (mandibular N.) Taste {ant 1/3}: chorda tympani nerve (facial nerve) Cheeks: buccal nerve (mandibular N.) Buccinator muscle: Buccal Nerve 1 (facial Nerve) Orbicularis oris muscle: facial nerve Tip: Submental LNs Tongue lingual artery (ECA) sides of ant 2/3: Ant 1/3: Lingual nerve (sensory) & tonsillar branch of facial artery lingual veins correspond to submandibular & chorda tympani (Taste) (ECA) the arteries and drain into IJV deep cervical LNs Post 2/3: glossopharyngeal N. (both) ascending pharyngeal artery post 1/3: Deep (ECA) cervical LNs greater palatine vein greater palatine artrey Palate Hard Palate: greater palatine and (→maxillary V.) (maxillary A.) nasopalatine nerves ascending palatine vein Deep cervical lymph ascending palatine artrey Soft Palate: lesser palatine and (→facial V.) nodes (facial A.) glossopharyngeal nerves ascending pharyngeal ascending pharyngeal artery vein PANS (secreto-motor) & Sensory: 2 Parotid gland Auriculotemporal nerve {Inferior salivary Nucleus → tympanic branch of glossopharyngeal N.→ Lesser petrosal nerve parasympathetic preganglionic fibres → otic ganglia → auriculotemporal nerve parasympathetic postganglionic fibres} sheet PART INNERVATION BLOOD SUPPLY VENOUS DRAINAGE LYMPH DRAINAGE PANS (secreto-motor): facial nerve Submandibular Sensory: lingual nerve gland {Superior salivary Nucleus → Chorda tympani branch from facial -

Variation in the Origin of Obturator Artery
Indian Journal of Clinical Anatomy and Physiology 2019;6(4):401–404 Content available at: iponlinejournal.com Indian Journal of Clinical Anatomy and Physiology Journal homepage: www.innovativepublication.com Original Research Article Variation in the origin of obturator artery Karishma Sharma1, Prashant Prasad1, Mathew Joseph1, Mukesh Singla1, K S Ravi1, Brijendra Singh1,* 1Dept. of Anatomy, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India ARTICLEINFO ABSTRACT Article history: Introduction: An ideal method of exploring the surgical anatomy and the variations and anomalies is Received 09-11-2019 the human cadaver. The anatomical region of pelvic cavity consists of a large number of organs and Accepted 14-11-2019 structures. The clear knowledge of vascular pattern and its variations is significant. The laparoscopic Available online 31-12-2019 surgical procedures for herniorrhaphy and hernio plasty makes the study of the pelvic vascular structures very important. The obturator artery which is normally a branch of anterior division of internal iliac artery has high frequency of variations which brings attention of many anatomists and surgeons to its origin and Keywords: course. Anterior trunk Materials and Methods: The present study was conducted on 24 hemi pelvises of 12 adult cadavers, Posterior trunk independent of age and sex dissected in the department of Anatomy, AIIMS, Rishikesh, India. During the Internal Iliac Artery dissection, origin and course of the obturator artery were traced. The handy instruction booklet of Anatomy Obturator artery by Cunningham was referred as the standard for all the dissections. Pelvic vasculature Observation and Result: In 22 specimens out of the 24 pelvic halves, the obturator artery originated from Variations the anterior division of the internal iliac artery (IIA). -

Vascular Anatomy of the Lower Limb
Vascular anatomy of the lower limb Musculoskeletal block- Anatomy-lecture 17 Editing file Objectives Color guide : Only in boys slides in Green Only in girls slides in Purple ✓ List the main arteries of the lower limb. important in Red ✓ Describe their origin, course distribution & branches. Doctor note in Blue Extra information in Grey ✓ List the main arterial anastomosis ✓ List the sites where you feel the arterial pulse. ✓ Differentiate the veins of the lower limb into superficial & deep. ✓ Describe their origin, course & termination and tributaries. For best understand check this:https://youtu.be/JNczJx2ju3I ➢ Is the main arterial supply to the lower limb Femoral artery ➢ It is the continuation of the external iliac artery Beginning Relations Terminations Branches It enters the thigh In the femoral triangle the Terminates by passing The femoral artery supplies: lower behind the inguinal artery is superficial covered through the adductor canal abdominal wall, thigh & external ligament point only by skin & fascia. (deep to sartorius) genitalia through the following (midway between the Posterior: Hip joint, It exits the canal by passing branches: anterior superior iliac separated from it by psoas through the adductor hiatus 1- superficial epigastric spine & the symphysis muscle and becomes the popliteal 2- superficial circumflex iliac pubis Medial: femoral vein. artery 3- superficial external pudendal Lateral: femoral nerve & its 4- deep external pudendal branches 5- profunda femoris (deep artery of thigh) Inguinal ligament Cannulation of FA: because of the superficial position of the femoral artery, it is used for left cardiac angiography. A long catheter is inserted percutaneously into the artery and passed up the external iliac artery, common iliac artery , aorta to the left ventricle. -
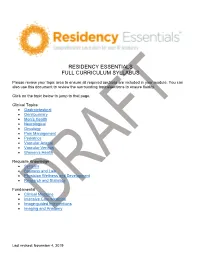
Residency Essentials Full Curriculum Syllabus
RESIDENCY ESSENTIALS FULL CURRICULUM SYLLABUS Please review your topic area to ensure all required sections are included in your module. You can also use this document to review the surrounding topics/sections to ensure fluidity. Click on the topic below to jump to that page. Clinical Topics • Gastrointestinal • Genitourinary • Men’s Health • Neurological • Oncology • Pain Management • Pediatrics • Vascular Arterial • Vascular Venous • Women’s Health Requisite Knowledge • Systems • Business and Law • Physician Wellness and Development • Research and Statistics Fundamental • Clinical Medicine • Intensive Care Medicine • Image-guided Interventions • Imaging and Anatomy Last revised: November 4, 2019 Gastrointestinal 1. Portal hypertension a) Pathophysiology (1) definition and normal pressures and gradients, MELD score (2) Prehepatic (a) Portal, SMV or Splenic (i) thrombosis (ii) stenosis (b) Isolated mesenteric venous hypertension (c) Arterioportal fistula (3) Sinusoidal (intrahepatic) (a) Cirrhosis (i) ETOH (ii) Non-alcoholic fatty liver disease (iii) Autoimmune (iv) Viral Hepatitis (v) Hemochromatosis (vi) Wilson's disease (b) Primary sclerosing cholangitis (c) Primary biliary cirrhosis (d) Schistosomiasis (e) Infiltrative liver disease (f) Drug/Toxin/Chemotherapy induced chronic liver disease (4) Post hepatic (a) Budd Chiari (Primary secondary) (b) IVC or cardiac etiology (5) Ectopic perianastomotic and stomal varices (6) Splenorenal shunt (7) Congenital portosystemic shunt (Abernethy malformation) b) Measuring portal pressure (1) Direct -

Anatomy of the Visceral Branches of the Iliac Arteries in Newborns
MOJ Anatomy & Physiology Research Article Open Access Anatomy of the visceral branches of the iliac arteries in newborns Abstract Volume 6 Issue 2 - 2019 The arising of the branches of the internal iliac artery is very variable and exceeds in this 1 2 feature the arterial system of any other area of the human body. In the literature, there is Valchkevich Dzmitry, Valchkevich Aksana enough information about the anatomy of the branches of the iliac arteries in adults, but 1Department of normal anatomy, Grodno State Medical only a few research studies on children’s material. The material of our investigation was University, Belarus 23 cadavers of newborns without pathology of vascular system. Significant variability of 2Department of clinical laboratory diagnostic, Grodno State iliac arteries of newborns was established; the presence of asymmetry in their structure was Medical University, Belarus shown. The dependence of the anatomy of the iliac arteries of newborns on the sex was revealed. Compared with adults, the iliac arteries of newborns and children have different Correspondence: Valchkevich Dzmitry, Department structure, which should be taken into account during surgical operations. of anatomy, Grodno State Medical University, Belarus, Tel +375297814545, Email Keywords: variant anatomy, arteries of the pelvis, sex differences, correlation, newborn Received: March 31, 2019 | Published: April 26, 2019 Introduction morgue. Two halves of each cadaver’s pelvis was involved in research, so 46 specimens were used in total: 18 halves were taken from boy’s Diseases of the cardiovascular system are one of the leading cadavers (9 left and 9 right) and 27 ones from the girls cadavers (14 problems of modern medicine. -

Product Information
G30 Latin VASA CAPITIS et CERVICIS ORGANA INTERNA 1 V. frontalis 49 Pulmo sinister 2 V. temporalis superficialis 50 Atrium dextrum 3 A. temporalis superficialis 51 Atrium sinistrum 3 a A. maxillaris 52 Ventriculus dexter 4 A. occipitalis 53 Ventriculus sinister 5 A. supratrochlearis 54 Valva aortae 6 A. et V. angularis 55 Valva trunci pulmonalis 7 A. et V. facialis 56 Septum interventriculare 7 a A. lingualis 57 Diaphragma 9 V. retromandibularis 58 Hepar 10 V. jugularis interna 11 A. thyroidea superior VASA ORGANORUM INTERNORUM 12 A. vertebralis 59 Vv. hepaticae 13 Truncus thyrocervicalis 60 V. gastrica dextra et sinistra 14 Truncus costocervicalis 61 A. hepatica communis 15 A. suprascapularis 61 a Truncus coeliacus 16 A. et V. subclavia dextra 62 V. mesenterica superior 17 V. cava superior 63 V. cava inferior 18 A. carotis communis 64 A. et V. renalis 18 a A. carotis externa 65 A. mesenterica superior 19 Arcus aortae 66 A. et V. lienalis 20 Pars descendens aortae 67 A. gastrica sinistra 68 Pars abdominalis® aortae VASA MEMBRII SUPERIORIS 69 A. mesenterica inferior 21 A. et V. axillaris 22 V. cephalica VASA REGIONIS PELVINAE 22 a A. circumflexa humeri anterior 72 A. et V. iliaca communis 22 b A. circumflexa humeri posterior 73 A. et V. iliaca externa 23 A. thoracodorsalis 74 A. sacralis mediana 24 A. et V. brachialis 75 A. et V. iliaca interna 25 A. thoracoacromialis 26 A. subclavia sinistra VASA MEMBRI INFERIORIS 27 V. basilica 76 Ramus ascendens a. circumflexae femoris 28 A. collateralis ulnaris superior lateralis 29 A. ulnaris 77 Ramus descendens a.