Evidence Based Interventional Pain Practice: According to Clinical Diagnoses
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
My Tooth Hurts: Your Guide to Feeling Better Fast by Dr
Copyright © 2017 by Dr. Scott Shamblott All rights reserved. No part of this book may be reproduced, stored in a retrieval system, or transmitted in any form or by any means—including electronic, mechanical, photocopying, recording, or otherwise—without the prior written permission of Dental Education Press, except for brief quotations or critical reviews. For more information, call 952-935-5599. Dental Education Press, Shamblott Family Dentistry, and Dr. Shamblott do not have control over or assume responsibility for third-party websites and their content. At the time of this book’s publication, all facts and figures cited are the most current available, as are all costs and cost estimates. Keep in mind that these costs and cost estimates may vary depending on your dentist, your location, and your dental insurance coverage. All stories are those of real people and are shared with permission, although some names have been changed to protect patient privacy. All telephone numbers, addresses, and website addresses are accurate and active; all publications, organizations, websites, and other resources exist as described in the book. While the information in this book is accurate and up to date, it is general in nature and should not be considered as medical or dental advice or as a replacement for advice from a dental professional. Please consult a dental professional before deciding on a course of action. Printed in the United States of America. Dental Education Press, LLC 33 10th Avenue South, Suite 250 Hopkins, MN 55343 952-935-5599 Help! My Tooth Hurts: Your Guide to Feeling Better Fast by Dr. -

Opioid Withdrawal ��������������������������������������������������������������������������������������������������� 15 Mark S
Magdalena Anitescu Honorio T. Benzon Mark S. Wallace Editors Challenging Cases and Complication Management in Pain Medicine 123 Challenging Cases and Complication Management in Pain Medicine Magdalena Anitescu Honorio T. Benzon • Mark S. Wallace Editors Challenging Cases and Complication Management in Pain Medicine Editors Magdalena Anitescu Honorio T. Benzon Department of Anesthesia and Critical Care Department of Anesthesiology University of Chicago Medicine Northwestern University Chicago, IL Feinberg School of Medicine USA Chicago, IL USA Mark S. Wallace Division of Pain Medicine Department of Anesthesiology University of California San Diego School of Medicine La Jolla, CL USA ISBN 978-3-319-60070-3 ISBN 978-3-319-60072-7 (eBook) https://doi.org/10.1007/978-3-319-60072-7 Library of Congress Control Number: 2017960332 © Springer International Publishing AG 2018 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifically the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfilms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a specific statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. The publisher, the authors and the editors are safe to assume that the advice and information in this book are believed to be true and accurate at the date of publication. -

Covering the Receiver
PERCUTANEOUS RADIOFREQUENCY THERMAL LUMBAR SYMPATHECTOMY AND ITS CLINICAL USE PERCUTANEOUS RADIOFREQUENCY THERMAL LUMBAR SYMPATHECTOMY AND ITS CLINICAL USE Thermische Iurn bale sympathectomie door mid del van· percutane radiofrequency en zijn klinische toepassing PROEFSCHRIFT ter verkrijging van de graad van doctor aan de Erasmus Universiteit Rotterdam op gezag van de rector magnificus Prof. Dr. A.H.G. Rinnooy Kan en volgens besluit van het College van Dekanen. De openbare verdediging zal plaatsvinden op vrijdag 23 september 1988 om 15.00 uur door JANINA PERNAK geboren te Polen Eburon Delft 1988 PROMOTIECOMMISSIE: Promotor: Prof. Dr. W. Erdmann Overige !eden: Prof. Dr. P. Scherpereel (Lille) Prof. Dr. O.T. Terpstra Prof. Dr. B.D.· Bangma CONTENTS ABBREVIATIONS I INTRODUCTION 1 II AIMS OF STUDY 2 PART ONE: LITERATURE REVIEW Chapter 1 DIFFERENT THERAPIES IN THE REFLEX SYMPATHETIC DYSTROPHY 5 I Introduction 5 II Reflex Sympathetic Dystrophy and its treatment 7 1 Physical therapy 9 2 Pharmacological intervention 9 3 Transcutaneous electrostimulation 10 4 Dorsal spinal cord stimulation 11 5 Acupuncture 13 6 Laser 13 7 Cryoanalgesia 15 8 Percutaneous facet joints denervation 17 9 Epidural blocks 17 10 Sympathetic blocks 19 11 Intravenous sympathetic blocks 20 12 Sympathectorp.y 20 Chapter 2 SYMPATHECTOMY 21 I Historical Review 21 II Lumbar sympathectomy: 21 a. surgical - technique 21 b. chemical - technique 23 III Comparison between surgical and chemical sympathectomy 25 IV Summary and conclusions 25 PART TWO : OWN INVESTIGATION AND FINDINGS -

Third Molar (Wisdom) Teeth
Third molar (wisdom) teeth This information leaflet is for patients who may need to have their third molar (wisdom) teeth removed. It explains why they may need to be removed, what is involved and any risks or complications that there may be. Please take the opportunity to read this leaflet before seeing the surgeon for consultation. The surgeon will explain what treatment is required for you and how these issues may affect you. They will also answer any of your questions. What are wisdom teeth? Third molar (wisdom) teeth are the last teeth to erupt into the mouth. People will normally develop four wisdom teeth: two on each side of the mouth, one on the bottom jaw and one on the top jaw. These would normally erupt between the ages of 18-24 years. Some people can develop less than four wisdom teeth and, occasionally, others can develop more than four. A wisdom tooth can fail to erupt properly into the mouth and can become stuck, either under the gum, or as it pushes through the gum – this is referred to as an impacted wisdom tooth. Sometimes the wisdom tooth will not become impacted and will erupt and function normally. Both impacted and non-impacted wisdom teeth can cause problems for people. Some of these problems can cause symptoms such as pain & swelling, however other wisdom teeth may have no symptoms at all but will still cause problems in the mouth. People often develop problems soon after their wisdom teeth erupt but others may not cause problems until later on in life. -

Would You Go to Your PCP for a Toothache? He Or She Is Trained in All Aspects of the Human Body and Has a Good Understanding of the Teeth and Gums
WOULD YOU GO TO YOUR PCP FOR A TOOTHACHE? I pose the question, "Would you go to your PCP for a toothache? He or she is trained in all aspects of the human body and has a good understanding of the teeth and gums. He or she knows that healthy teeth play an important part in overall health, so certainly one would think that going to him or her might be a good option. But you don't. Why not? Well, because we all know that a dentist has more specific training, knowledge and experience with teeth and related matters. In fact, even if you did go to your PCP, I bet 99.99% or more would send you to your dentist, and you would thank them and do so without hesitation. This Photo by Unknown Author is licensed under CC BY-NC-ND So, who should you see if you are having musculoskeletal problems? To this day about 86% of people would select their primary physician or equivalent medical practice for these issues. Is that any smarter than seeing him or her for your teeth? Studies in 2004, 2006 and 2007 found that not only were the areas of spinal dysfunction and mechanical back pain not understood by the medical doctors, but most had little if any training in the area and almost no experience treating it. The typical response to treating low back pain is still to provide pain medication, muscle relaxants, order an x-ray and possibly refer to physical therapy. This is the routine in spite of the 1994 U.S. -

08. Serdar Erdine.Indd
AĞRI 2009;21(4):133-140 REVIEW - DERLEME Neurolytic blocks: When, How, Why Nörolitik bloklar: Ne zaman, Nasıl, Niçin Serdar ERDİNE1 Summary Interventional techniques are divided into two categories: neuroablative and neuromodulatory procedures. Neuroablation is the physical interruption of pain pathways either surgically, chemically or thermally. Neuromodulation is the dynamic and functional inhibition of pain pathways either by administration of opioids and other drugs intraspinally or intraventricularly or by stimulation. Neuroablative techniques for cancer pain treatment have been used for more than a century. With the de- velopment of imaging facilities such as fl uoroscopy, neuroablative techniques can be performed more precisely and effi ciently. Key words: Neuroablative techniques; neurolytic blocks; radiofrequency thermocoagulation. Özet Girişimsel teknikler nöroablatif ve nöromodülatör işlemler olarak iki gruba ayrılırlar. Nöroablasyon, cerrahi, kimyasal veya ısı uy- gulamalarıyla ağrı yolaklarında fi ziksel iletinin kesilmesidir. Nöromodülasyon, stimülasyon uygulamasıyla veya intraventriküler ya da intraspinal uygulanan opioidler ve diğer ajanlarla ağrı yolaklarının dinamik ve fonksiyonel inhibisyonudur. Nöroablatif teknik- ler kanser tedavisinde yüzyıldan fazla zamandır kullanılmaktadır. Fluroskopi gibi görüntüleme araçlarındaki gelişmelerle nöroabla- tif uygulamalar daha doğru ve etkili bir şekilde gerçekleştirilmektedir. Anahtar sözcükler: Nöroablatif teknikler; nörolitik bloklar; radyofrekans termokoagulasyon. 1Department of -

Transcutaneous Electrical Nerve Stimulation for Acute Pain (Review)
Transcutaneous electrical nerve stimulation for acute pain (Review) Walsh DM, Howe TE, Johnson MI, Moran F, Sluka KA This is a reprint of a Cochrane review, prepared and maintained by The Cochrane Collaboration and published in The Cochrane Library 2011, Issue 8 http://www.thecochranelibrary.com Transcutaneous electrical nerve stimulation for acute pain (Review) Copyright © 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd. TABLE OF CONTENTS HEADER....................................... 1 ABSTRACT ...................................... 1 PLAINLANGUAGESUMMARY . 2 BACKGROUND .................................... 2 OBJECTIVES ..................................... 3 METHODS ...................................... 3 RESULTS....................................... 6 Figure1. ..................................... 9 Figure2. ..................................... 10 DISCUSSION ..................................... 13 AUTHORS’CONCLUSIONS . 14 ACKNOWLEDGEMENTS . 14 REFERENCES ..................................... 15 CHARACTERISTICSOFSTUDIES . 19 DATAANDANALYSES. 49 Analysis 1.1. Comparison 1 TENS versus placebo TENS, Outcome 1 VAS >50% pain relief post treatment. 50 Analysis 1.2. Comparison 1 TENS versus placebo TENS, Outcome 2 Pain rating index >50% pain relief post treatment. 51 Analysis 1.3. Comparison 1 TENS versus placebo TENS, Outcome 3 VAS for pain intensity after two days of treatment. 51 Analysis 1.4. Comparison 1 TENS versus placebo TENS, Outcome 4 Numerical rating scale for pain intensity during procedure................................... -

Clinical Diagnosis of Herpes Zoster Presenting As Odontogenic Pain
대한치과보존학회지: Vol. 33, No. 5, 2008 Clinical Diagnosis of Herpes Zoster Presenting as Odontogenic Pain Seong-Hak Yang, Dong-Ho Jung, Hae-Doo Lee, Yoon Lee, Hoon-Sang Chang, Kyung-San Min* Department of Conservative Dentistry, College of Dentistry, Wonkwang University ABSTRACT Herpes zoster, an acute viral infection produced by the varicella zoster virus, may affect any of the trigeminal branches. This case report presents a patient with symptoms mimicking odontogenic pain. No obvious cause of the symptoms could be found based on clinical and radiographic examinations. After a dermatologist made a diagnosis of herpes zoster involving the third trigeminal branch, the patient was given antiviral therapy. Two months later, the facial lesions and pain had almost disap- peared, and residual pigmented scars were present. During the diagnostic process, clinicians should keep in mind the possibility that orofacial pain might be related to herpes zoster. [J Kor Acad Cons Dent 33(5):452-456, 2008] Key words : Herpes zoster, Trigeminal nerve, Odontogenic pain - Received 2008.7.2., revised 2008.8.4., accepted 2008.8.25- Ⅰ. INTRODUCTION affected by the reactivation of the latent herpes zoster virus the most. The first division of the Diagnostic assessment in patients with orofacial trigeminal nerve is commonly affected, whereas pain may be challenging due to the close proximi- the second and third divisions are rarely ty between the teeth and other orofacial tissues, involved4). If the third division of the trigeminal and symptoms associated with neurological disor- nerve is affected, it may be characterized by pul- ders. Herpes zoster (shingles) is caused by the pitis in the mandibular molars and vesicular skin reactivation of the latent varicella-zoster virus eruptions in the affected sensory nerve area. -

Acute Low Back Pain
Acute low back pain Key reviewers: Mr Chris Hoffman, Orthopaedic Surgeon, Mana Orthopaedics, Wellington Dr John MacVicar, Medical Director, Southern Rehab, Christchurch Key concepts: ■ Acute low back pain is common and most patients will recover fully within three months ■ Serious causes are rare and can be excluded with careful history and examination ■ Radiological studies are not required for acute low back pain in the absence of red flags ■ An exact diagnosis is often not possible, nor needed for management ■ Patients’ beliefs and attitudes warrant as much attention as the anatomical and pathological aspects of their condition ■ Fear about pain is a major determinant of disability and possible chronicity ■ Management should include reassurance, education and helping the patient stay active ■ Adequate analgesia is important to allow the patient www.bpac.org.nz keyword: lowbackpain to stay active 6 | BPJ | Issue 21 Acute low back pain is common and often relapsing Red Flags: ▪ Trauma Low back pain is discomfort, muscle tension or stiffness ▪ Unrelenting pain, or pain worse at night localised to the area around the lumbar spine. Back pain (supine) may radiate to the groin, buttocks or legs as referred somatic pain and may be associated with lumbar radicular ▪ Age <20 years, or new back pain age >50 pain such as sciatica. years ▪ History of cancer In any given year approximately one third of adults will ▪ Systemic symptoms suffer from low back pain and one third of these will seek help from a health practitioner.1 Most people with low ▪ IV drug use back pain self-treat with over-the-counter medications and ▪ Immunosuppression or steroids lifestyle changes.2 ▪ Widespread or progressive neurological deficit Low back pain is described as acute if present for less than six weeks, sub-acute between six weeks and three Serious causes of acute low back pain are rare months, and chronic if it continues for longer than three and include:6 months. -

Simultaneous Occurrence of Chicken Pox and Herpes Zoster with Facial Nerve Palsy in Immunocompetentpatient- a Case Report
Case Report J Cardiol & Cardiovasc Ther Volume 11 Issue 4 - August 2018 Copyright © All rights are reserved by Basumatary LJ DOI: 10.19080/JOCCT.2018.11.555816 Simultaneous Occurrence of Chicken Pox and Herpes Zoster with Facial Nerve Palsy in ImmunocompetentPatient- A Case Report Basumatary LJ1* and Lalit MB2 1Consultant Neurologist, Downtown Hospitals, India 2Department of Neurology, Downtown Hospitals, India Submission: May 10, 2018; Published: August 06, 2018 *Corresponding author: Basumatary LJ, Consultant Neurologist, Downtown Hospitals, India, Email: Abstract Herpes zoster is caused by reactivation of the latent varicella zoster virus which is present due to an earlier varicella infection. The prodromal stage, the only presenting symptom may be odontalgia, which may prove to be a diagnostic challenge, since many diseases can cause simultaneous occurrence of herpes zoster and varicella zoster in the same patient is sufficiently uncommon to warrant notice. During the division of right trigeminal nerve masquerading as odontalgia with simultaneous occurrence of varicella zoster and right facial nerve palsy. or facial pain, and the diagnosis must be properly established before final treatment. Here we present a case of herpes zoster involving the second Keywords: Herpes zoster; Chicken-pox; Varicella zoster virus; Simultaneous occurrence of chicken pox and herpes zoster; Odontalgia Introduction Herpes Zoster (HZ) occurs as a reactivation of Varicella Zoster Case Report Virus (VZV) that remains latent in dorsal sensory nerve root 48 year old male non diabetic non hypertensive developed ganglion after primary varicella infection (chicken-pox). Bokay papulo-vesicular rashes over right side of face, toothache and fever. He approached to a local dentist and was advised to take co- & HZ. -

Common Emergencies
ADVICE SHEET WHAT TO DO IF YOU HAVE TOOTHACHE PAIN SYMPTOMS: ✅ Comes on when eating or drinking ✅ Lasts seconds or minutes ✅ Not disturbing sleep ✅ Can be relieved by painkillers ✅ Difficult to localise to one specific tooth [email protected] 0141 779 9274 8 Station Road, Muirhead www.hannigandentalcare.co.uk Glasgow, G69 9EE Page 1 of 6 ADVICE: WHAT TO DO IF YOU HAVE TOOTHACHE Sensitivity/Reversible Toothache PAIN SYMPTOMS: ✅ Comes on when eating or drinking ✅ Lasts seconds or minutes ✅ Not disturbing sleep ✅ Can be relieved by painkillers ✅ Difficult to localise to one specific tooth If this sounds like the type of pain you are experiencing then it is likely you are suffering from sensitivity. This is usually relieved with the use of a desensitising toothpaste, e.g. Sensodyne Rapid Relief. You should use a desensitising toothpaste every morning and night; place it on to a dry toothbrush and brush round – do not rinse out with water or mouthwash afterwards and do not have anything to drink for 30 minutes afterwards. Each time you use these toothpastes they form a microscopic layer on the teeth; with each use this barrier layer gets thicker and thus more effective at insulating the tooth from the hot/cold, so it takes about 2 weeks before it’s working at its optimum. If you are going to have e.g. a cold drink you can rub some directly on to the sensitive tooth with your finger for a minute beforehand and this should help to desensitise it. If you stop using these toothpastes the protective layer will eventually get washed away and your sensitivity will return. -
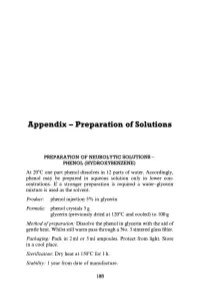
Appendix - Preparation of Solutions
Appendix - Preparation of Solutions PREPARATION OF NEUROLYTIC SOLUTIONS - PHENOL (HYDROXYBENZENE) At 20 0 e one part phenol dissolves in 12 parts of water. Accordingly, phenol may be prepared in aqueous solution only in lower con centrations. If a stronger preparation is required a water-glycerin mixture is used as the solvent. Product: phenol injection 5% in glycerin Formula: phenol crystals 5 g glycerin (previously dried at 120 0 e and cooled) to 100 g Method o/preparation: Dissolve the phenol in glycerin with the aid of gentle heat. Whilst still warm pass through a No.3 sintered glass filter. Packaging: Pack in 2 ml or 5 ml ampoules. Protect from light. Store in a cool place. Sterilization: Dry heat at 1500 e for 1 h. Stability: 1 year from date of manufacture. 185 186 Appendix Product: aqueous phenol 5% phenol injection 7% Formula: phenol crystals 5 g phenol crystals 7 g water for injections glycerin 50% v/v in water for injec to 100ml tions to 100 ml Method of preparation: Pass through sintered glass filter, pack in ampoules and sterilize by autoclaving at U5°e for 30 min. Packaging: 2 ml or 5 ml ampoules. Protect from light. Store in a cool place. Precautions: Avoid prolonged contact with rubber or plastics. Stability: 1 year from date of sterilization. INJECTION ABSOLUTE ALCOHOL Method ofpreparation: In order to avoid absorption of moisture, the infiltration procedure is best carried out under positive pressure, using solvent inert membrane filters. The preparation is then packed in 2 ml or 5 ml ampoules. Sterilization: Autoclave at 155°e for 30 min.