Я-Hydroxybutyrate Ketosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Limited Role of Glucagon for Ketogenesis During Fasting Or in Response to SGLT2 Inhibition
882 Diabetes Volume 69, May 2020 The Limited Role of Glucagon for Ketogenesis During Fasting or in Response to SGLT2 Inhibition Megan E. Capozzi,1 Reilly W. Coch,1,2 Jepchumba Koech,1 Inna I. Astapova,1,2 Jacob B. Wait,1 Sara E. Encisco,1 Jonathan D. Douros,1 Kimberly El,1 Brian Finan,3 Kyle W. Sloop,4 Mark A. Herman,1,2,5 David A. D’Alessio,1,2 and Jonathan E. Campbell1,2,5 Diabetes 2020;69:882–892 | https://doi.org/10.2337/db19-1216 Glucagon is classically described as a counterregula- the oxidation of fatty acids, a shift in fuel utilization that tory hormone that plays an essential role in the pro- coordinates energy needs and glucose production (2). The tection against hypoglycemia. In addition to its role in actions of glucagon to increase lipid oxidation, including the regulation of glucose metabolism, glucagon has the production of ketone bodies that is a downstream end been described to promote ketosis in the fasted state. point of this process, have been defined by numerous – Sodium glucose cotransporter 2 inhibitors (SGLT2i) are experiments with cultured hepatocytes (3–5). Moreover, a new class of glucose-lowering drugs that act primarily the classic studies of Gerich et al. (6), using somatostatin to in the kidney, but some reports have described direct reduce circulating glucagon and mitigate diabetic ketoaci- effects of SGLT2i on a-cells to stimulate glucagon se- dosis (DKA), add to the now ingrained belief that glucagon cretion. Interestingly, SGLT2 inhibition also results in increased endogenous glucose production and ketone has both glucogenic and ketogenic activities. -

Diabetic Ketoacidosis and Hyperosmolar BMJ: First Published As 10.1136/Bmj.L1114 on 29 May 2019
STATE OF THE ART REVIEW Diabetic ketoacidosis and hyperosmolar BMJ: first published as 10.1136/bmj.l1114 on 29 May 2019. Downloaded from hyperglycemic syndrome: review of acute decompensated diabetes in adult patients Esra Karslioglu French,1 Amy C Donihi,2 Mary T Korytkowski1 1Division of Endocrinology and Metabolism, Department of ABSTRACT Medicine, University of Pittsburgh, Pittsburgh, PA, USA Diabetic ketoacidosis and hyperosmolar hyperglycemic syndrome (HHS) are life threatening 2University of Pittsburgh School of complications that occur in patients with diabetes. In addition to timely identification of the Pharmacy, Pittsburgh, PA, USA Correspondence to: M Korytkowski precipitating cause, the first step in acute management of these disorders includes aggressive [email protected] administration of intravenous fluids with appropriate replacement of electrolytes (primarily Cite this as: BMJ 2019;365:l1114 doi: 10.1136/bmj.l1114 potassium). In patients with diabetic ketoacidosis, this is always followed by administration Series explanation: State of the of insulin, usually via an intravenous insulin infusion that is continued until resolution of Art Reviews are commissioned on the basis of their relevance to ketonemia, but potentially via the subcutaneous route in mild cases. Careful monitoring academics and specialists in the US and internationally. For this reason by experienced physicians is needed during treatment for diabetic ketoacidosis and HHS. they are written predominantly by Common pitfalls in management include premature termination of intravenous insulin US authors therapy and insufficient timing or dosing of subcutaneous insulin before discontinuation of intravenous insulin. This review covers recommendations for acute management of diabetic ketoacidosis and HHS, the complications associated with these disorders, and methods for http://www.bmj.com/ preventing recurrence. -

Persistent Lactic Acidosis - Think Beyond Sepsis Emily Pallister1* and Thogulava Kannan2
ISSN: 2377-4630 Pallister and Kannan. Int J Anesthetic Anesthesiol 2019, 6:094 DOI: 10.23937/2377-4630/1410094 Volume 6 | Issue 3 International Journal of Open Access Anesthetics and Anesthesiology CASE REPORT Persistent Lactic Acidosis - Think beyond Sepsis Emily Pallister1* and Thogulava Kannan2 1 Check for ST5 Anaesthetics, University Hospitals of Coventry and Warwickshire, UK updates 2Consultant Anaesthetist, George Eliot Hospital, Nuneaton, UK *Corresponding author: Emily Pallister, ST5 Anaesthetics, University Hospitals of Coventry and Warwickshire, Coventry, UK Introduction • Differential diagnoses for hyperlactatemia beyond sepsis. A 79-year-old patient with type 2 diabetes mellitus was admitted to the Intensive Care Unit for manage- • Remember to check ketones in patients taking ment of Acute Kidney Injury refractory to fluid resusci- Metformin who present with renal impairment. tation. She had felt unwell for three days with poor oral • Recovery can be protracted despite haemofiltration. intake. Admission bloods showed severe lactic acidosis and Acute Kidney Injury (AKI). • Suspect digoxin toxicity in patients on warfarin with acute kidney injury, who develop cardiac manifes- The patient was initially managed with fluid resus- tations. citation in A&E, but there was no improvement in her acid/base balance or AKI. The Intensive Care team were Case Description asked to review the patient and she was subsequently The patient presented to the Emergency Depart- admitted to ICU for planned haemofiltration. ment with a 3 day history of feeling unwell with poor This case presented multiple complex concurrent oral intake. On examination, her heart rate was 48 with issues. Despite haemofiltration, acidosis persisted for blood pressure 139/32. -
Unit 4 Acid-Base Homeostasis
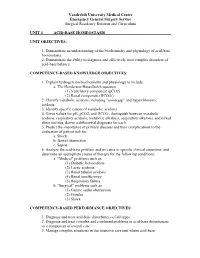
Vanderbilt University Medical Center Emergency General Surgery Service Surgical Residency Rotation and Curriculum UNIT 4 ACID-BASE HOMEOSTASIS UNIT OBJECTIVES: 1. Demonstrate an understanding of the biochemistry and physiology of acid-base homeostasis. 2. Demonstrate the ability to diagnose and effectively treat complex disorders of acid-base balance. COMPETENCY-BASED KNOWLEDGE OBJECTIVES: 1. Explain hydrogen ion biochemistry and physiology to include: a. The Henderson-Hasselbalch equation (1) Ventilatory component (pCO2) (2) Renal component (HCO3-) 2. Classify metabolic acidosis, including "anion gap" and hyperchloremic acidosis. 3. Identify specific causes of metabolic acidosis. 4. Given values for pH, pCO2, and HCO3-, distinguish between metabolic acidosis, respiratory acidosis, metabolic alkalosis, respiratory alkalosis, and mixed abnormalities; derive a differential diagnosis for each. 5. Predict the importance of primary diseases and their complications to the evaluation of patient risk for: a. Shock b. Bowel obstruction c. Sepsis 6. Analyze the acid-base problem and its cause in specific clinical situations, and determine an appropriate course of therapy for the following conditions: a. "Medical" problems such as: (1) Diabetic ketoacidosis (2) Lactic acidosis (3) Renal tubular acidosis (4) Renal insufficiency (5) Respiratory failure b. "Surgical" problems such as: (1) Gastric outlet obstruction (2) Fistulas (3) Shock COMPETENCY-BASED PERFORMANCE OBJECTIVES: 1. Diagnose and treat acid-base disturbances of all types. 2. Diagnose and treat complex and combined problems in acid-base disturbances as a component of overall care. 3. Manage complex situations in the intensive care unit where acid-base Vanderbilt University Medical Center Emergency General Surgery Service Surgical Residency Rotation and Curriculum abnormalities coexist with other metabolic derangements, including: a. -

Lecture-1 Keto Acidosis, Bovine Ketosis, Ovine Pregnancy Toxemia
Lecture-1 Keto acidosis Ketoacidosis is a metabolic acidosis due to an excessive blood concentration of ketone bodies (acetone, acetoacetate and beta-hydroxybutyrate). Ketone bodies are released into the blood from the liver when hepatic lipid metabolism has changed to a state of increased ketogenesis. The abnormal accumulation of ketones in the body occurs due to excessive breakdown of fats in deficiency or inadequate use of carbohydrates. It is characterized by ketonuria, loss of potassium in the urine, and a fruity odor of acetone on the breath. Untreated, ketosis may progress to ketoacidosis, coma, and death. This condition is seen in starvation, occasionally in pregnancy if the intake of protein and carbohydrates is inadequate, and most frequently in diabetes mellitus. Different Types of Ketoacidosis Diabetes Keto Acidosis (DKA): Due to lack of insulin glucose uptake and metabolism by cells is decrased.Fatty acid catabolism increased in resulting in excess production of ketone bodies. Starvation Ketosis: Starvation leads to hypoglycemia as there is little or no absorption of glucose from intestine and also due to depletion of liver glycogen. In Fatty acid oxidation leads to excess ketone body. Bovine Ketosis Introduction Bovine ketosis occurs in the high producing dairy cows during the early stages of lactation, when the milk production is generally the highest. Abnormally high levels of the ketone bodies, acetone, acetoacetic and beta-hydroxy butyric acid and also iso- propanol appear in blood, urine and in milk. The alterations are accompanied by loss of appetite , weight loss, decrease in milk production and nervous disturbances. Hypoglycemia (starvation) is a common finding in bovine ketosis and in ovine pregnancy toxemia. -

Diabetic Ketoalkalosis in Children and Adults
Original Article Diabetic Ketoalkalosis in Children and Adults Emily A. Huggins, MD, Shawn A. Chillag, MD, Ali A. Rizvi, MD, Robert R. Moran, PhD, and Martin W. Durkin, MD, MPH and DR are calculated because the pH and bicarbonate may be near Objectives: Diabetic ketoacidosis (DKA) with metabolic alkalosis normal or even elevated. In addition to having interesting biochemical (diabetic ketoalkalosis [DKALK]) in adults has been described in the features as a complex acid-base disorder, DKALK can pose diagnostic literature, but not in the pediatric population. The discordance in the and/or therapeutic challenges. change in the anion gap (AG) and the bicarbonate is depicted by an Key Words: delta ratio, diabetic ketoacidosis, diabetic ketoalkalosis, elevated delta ratio (DR; rise in AG/drop in bicarbonate), which is metabolic alkalosis normally approximately 1. The primary aim of this study was to de- termine whether DKALK occurs in the pediatric population, as has been seen previously in the adult population. The secondary aim was iabetic ketoacidosis (DKA), a common and serious dis- to determine the factors that may be associated with DKALK. Dorder that almost always results in hospitalization, is de- Methods: A retrospective analysis of adult and pediatric cases with a fined by the presence of hyperglycemia, reduced pH, metabolic 1 primary or secondary discharge diagnosis of DKA between May 2008 and acidosis, elevated anion gap (AG), and serum or urine ketones. August 2010 at a large urban hospital was performed. DKALK was as- In some situations, a metabolic alkalosis coexists with DKA sumedtobepresentiftheDRwas91.2 or in cases of elevated bicarbonate. -

Diabetic Ketoacidosis: Evaluation and Treatment DYANNE P
Diabetic Ketoacidosis: Evaluation and Treatment DYANNE P. WESTERBERG, DO, Cooper Medical School of Rowan University, Camden, New Jersey Diabetic ketoacidosis is characterized by a serum glucose level greater than 250 mg per dL, a pH less than 7.3, a serum bicarbonate level less than 18 mEq per L, an elevated serum ketone level, and dehydration. Insulin deficiency is the main precipitating factor. Diabetic ketoacidosis can occur in persons of all ages, with 14 percent of cases occurring in persons older than 70 years, 23 percent in persons 51 to 70 years of age, 27 percent in persons 30 to 50 years of age, and 36 percent in persons younger than 30 years. The case fatality rate is 1 to 5 percent. About one-third of all cases are in persons without a history of diabetes mellitus. Common symptoms include polyuria with polydipsia (98 percent), weight loss (81 percent), fatigue (62 percent), dyspnea (57 percent), vomiting (46 percent), preceding febrile illness (40 percent), abdominal pain (32 percent), and polyphagia (23 percent). Measurement of A1C, blood urea nitro- gen, creatinine, serum glucose, electrolytes, pH, and serum ketones; complete blood count; urinalysis; electrocar- diography; and calculation of anion gap and osmolar gap can differentiate diabetic ketoacidosis from hyperosmolar hyperglycemic state, gastroenteritis, starvation ketosis, and other metabolic syndromes, and can assist in diagnosing comorbid conditions. Appropriate treatment includes administering intravenous fluids and insulin, and monitoring glucose and electrolyte levels. Cerebral edema is a rare but severe complication that occurs predominantly in chil- dren. Physicians should recognize the signs of diabetic ketoacidosis for prompt diagnosis, and identify early symp- toms to prevent it. -

Diabetic Ketoacidosis Diabetic Ketoacidosis (DKA) Is a Serious Problem That Can Happen in People with Diabetes
Diabetic Ketoacidosis Diabetic ketoacidosis (DKA) is a serious problem that can happen in people with diabetes. DKA should be treated as a medical emergency. This is because it can lead to coma or death. If you have the symptoms of DKA, get medical help right away. DKA happens more often in people with type 1 diabetes. But it can happen in people with type 2 diabetes. It can also happen in women with diabetes during pregnancy (gestational diabetes). DKA happens when insulin levels are too low. Without enough insulin, sugar (glucose) can’t get to the cells of your body. The glucose stays in the blood. The liver then puts out even more glucose into the blood. This causes high blood glucose (hyperglycemia). Without glucose, your body breaks down stored fat for energy. When this happens, acids called ketones are released into the blood. This is called ketosis. High levels of ketones (ketoacidosis) can be harmful to you. Hyperglycemia and ketoacidosis can also cause serious problems in the blood and your body, such as: • Low levels of potassium (hypokalemia) and phosphate • Damage to kidneys or other organs • Coma What causes diabetic ketoacidosis? In people with diabetes, DKA is most often caused by too little insulin in the body. It is also caused by: • Poor management of diabetes • Infections such as a urinary tract infection or pneumonia • Serious health problems, such as a heart attack • Reactions to certain prescribed medicines including SGLT2 inhibitors for treating type 2 diabetes • Reactions to illegal drugs including cocaine • Disruption of insulin delivery from an insulin pump Symptoms of diabetic ketoacidosis DKA most often happens slowly over time. -

Ketosis Diagnosis and Monitoring in High-Producing Dairy Cows
Review Invited Review: Ketosis Diagnosis and Monitoring in High-Producing Dairy Cows Mariana Alves Caipira Lei 1 and João Simões 2,* 1 Department of Zootechnics, School of Agricultural and Veterinary Sciences, University of Trás-os-Montes e Alto Douro (UTAD), 5000-801 Vila Real, Portugal; [email protected] 2 Department of Veterinary Sciences, School of Agricultural and Veterinary Sciences, University of Trás-os-Montes e Alto Douro (UTAD), 5000-801 Vila Real, Portugal * Correspondence: [email protected]; Tel.: +351-259-350-666 Abstract: This work reviews the current impact and manifestation of ketosis (hyperketonemia) in dairy cattle, emphasizing the practical use of laboratory methods, field tests, and milk data to monitoring this disease. Ketosis is a major issue in high-producing cows, easily reaching a prevalence of 20% during early postpartum when the negative energy balance is well established. Its economic losses, mainly related to decreasing milk yield, fertility, and treatment costs, have been estimated up to €250 per case of ketosis/year, which can double if associated diseases are considered. A deep relationship between subclinical or clinical ketosis and negative energy balance and related production diseases can be observed mainly in the first two months postpartum. Fourier transform infrared spectrometry methods gradually take place in laboratory routine to evaluates body ketones (e.g., beta-hydroxybutyrate) and probably will accurately substitute cowside blood and milk tests at a farm in avenir. Fat to protein ratio and urea in milk are largely evaluated each month in dairy farms indicating animals at risk of hyperketonemia. At preventive levels, other than periodical evaluation of body condition score and controlling modifiable or identifying non-modifiable risk Citation: Lei, M.A.C.; Simões, J. -

Therapeutics of Corticosteroids in the Bovine Animal and Problems Surrounding Their Use W
Therapeutics of Corticosteroids in the Bovine Animal and Problems Surrounding Their Use W. D. Black, D. V.M.· Department of Biomedical Sciences Ontario Veterinary College · University of Guelph Guelph, Ontario The corticosteroids have been used extensively in Anti- Gluco- Sodium veterinary practice for the last 15 to 20 years. They inflammatory corticoid Retaining have offered the practitioners of veterinary medicine Compound Potency Potency Potency a tool useful for blocking a portion of the pathological 1-Jydrocortisone 1.01 1.02 1.01 changes seen in infectious and metabolic disease. Un Prednisolone 4.01 5.52 0.81 Cortisone 0.81 0.82 0.81 fortunately they have done little to advance the cause Triamcinolone 5.01 ~25.03 0.01 of specific disease therapy. I shall discuss the use of Betamethasone 102 - 25.01 ~25.03 0.01 corticosteroids by veterinarians in some conditions in Dexamethasone 102 - 25.01 ~25.03 0.01 Flumethasone ~75 -1004 ~75 - 1004 0.0 which they are widely employed and attempt to Predef (Fluoro- clarify their usefulness in some cases and their abuse prednisolone) 14.02 50.02 in others. Figure 2. Relative Potencies of Corticosteroids. First let us consider what the pharmacological properties of these agents are and which ones are most likely to be of therapeutic value (Figure 1). The titioner should select one that does not cause sodium ability of these agents to reduce an elevated retention in order to avoid the problems of edema for mation and fluid build-up that can be harmful to the 0 temperature, to reduce inflammatory and allergic "'O animal. -

Effects of Ketone Bodies on Brain Metabolism and Function In
International Journal of Molecular Sciences Review Effects of Ketone Bodies on Brain Metabolism and Function in Neurodegenerative Diseases Nicole Jacqueline Jensen 1,* , Helena Zander Wodschow 1, Malin Nilsson 1 and Jørgen Rungby 1,2 1 Department of Endocrinology, Bispebjerg University Hospital, 2400 Copenhagen, Denmark; [email protected] (H.Z.W.); malin.sofi[email protected] (M.N.); [email protected] (J.R.) 2 Copenhagen Center for Translational Research, Copenhagen University Hospital, Bispebjerg and Frederiksberg, 2400 Copenhagen, Denmark * Correspondence: [email protected] Received: 4 November 2020; Accepted: 18 November 2020; Published: 20 November 2020 Abstract: Under normal physiological conditions the brain primarily utilizes glucose for ATP generation. However, in situations where glucose is sparse, e.g., during prolonged fasting, ketone bodies become an important energy source for the brain. The brain’s utilization of ketones seems to depend mainly on the concentration in the blood, thus many dietary approaches such as ketogenic diets, ingestion of ketogenic medium-chain fatty acids or exogenous ketones, facilitate significant changes in the brain’s metabolism. Therefore, these approaches may ameliorate the energy crisis in neurodegenerative diseases, which are characterized by a deterioration of the brain’s glucose metabolism, providing a therapeutic advantage in these diseases. Most clinical studies examining the neuroprotective role of ketone bodies have been conducted in patients with Alzheimer’s disease, where brain imaging studies support the notion of enhancing brain energy metabolism with ketones. Likewise, a few studies show modest functional improvements in patients with Parkinson’s disease and cognitive benefits in patients with—or at risk of—Alzheimer’s disease after ketogenic interventions. -

Observations Compensatory Hypochloraemic Alkalosis In
Letters 871 tended to the DQ-LTR13 integration, where we also find a con- 2. Pascual M, Martin J, Nieto A et al. (2001) Distribution of tribution of DQ-LTR13 to RA susceptibility in DQ8-positive HERV-LTR elements in the 5′-flanking region of HLA- individuals. Furthermore we recently published that patients DQB1 and association with autoimmunity. Immunogenetics with Addison’s disease—another HLA DQ8-associated autoim- 53:114–118 mune disease of the adrenals which may occur in combination 3. Donner H, Tonjes RR, Bontrop RE et al. (1999) Intronic se- with Type 1 diabetes as part of the autoimmune pluriglandular quence motifs of HLA-DQB1 are shared between humans, syndrome Type 2—have more often the DQ8-DQ-LTR13 com- apes and Old World monkeys, but a retroviral LTR element bination in contrast to the DQ-LTR3 insertion. Although both (DQLTR3) is human specific. Tissue Antigens 53:551–558 DQ-LTR3 and DQ-LTR13 are linked to DQ8, DQ-LTR13 en- 4. Donner H, Tonjes RR, Van der Auwera B et al. (1999) The hances the risk for Addison’s disease [7]. presence or absence of a retroviral long terminal repeat Whether DQ-LTR13 has a functional significance or not is influences the genetic risk for type 1 diabetes conferred by currently under investigation. Preliminary data indicate that human leukocyte antigen DQ haplotypes. J Clin Endocrinol DQ-LTR13 harbours regulatory capacity and shows functional Metab 84:1404–1408 activity of an upstream element as revealed by analyses of nu- 5. Seidl C, Donner H, Petershofen E et al.