Observations Compensatory Hypochloraemic Alkalosis In
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diabetic Ketoacidosis and Hyperosmolar BMJ: First Published As 10.1136/Bmj.L1114 on 29 May 2019
STATE OF THE ART REVIEW Diabetic ketoacidosis and hyperosmolar BMJ: first published as 10.1136/bmj.l1114 on 29 May 2019. Downloaded from hyperglycemic syndrome: review of acute decompensated diabetes in adult patients Esra Karslioglu French,1 Amy C Donihi,2 Mary T Korytkowski1 1Division of Endocrinology and Metabolism, Department of ABSTRACT Medicine, University of Pittsburgh, Pittsburgh, PA, USA Diabetic ketoacidosis and hyperosmolar hyperglycemic syndrome (HHS) are life threatening 2University of Pittsburgh School of complications that occur in patients with diabetes. In addition to timely identification of the Pharmacy, Pittsburgh, PA, USA Correspondence to: M Korytkowski precipitating cause, the first step in acute management of these disorders includes aggressive [email protected] administration of intravenous fluids with appropriate replacement of electrolytes (primarily Cite this as: BMJ 2019;365:l1114 doi: 10.1136/bmj.l1114 potassium). In patients with diabetic ketoacidosis, this is always followed by administration Series explanation: State of the of insulin, usually via an intravenous insulin infusion that is continued until resolution of Art Reviews are commissioned on the basis of their relevance to ketonemia, but potentially via the subcutaneous route in mild cases. Careful monitoring academics and specialists in the US and internationally. For this reason by experienced physicians is needed during treatment for diabetic ketoacidosis and HHS. they are written predominantly by Common pitfalls in management include premature termination of intravenous insulin US authors therapy and insufficient timing or dosing of subcutaneous insulin before discontinuation of intravenous insulin. This review covers recommendations for acute management of diabetic ketoacidosis and HHS, the complications associated with these disorders, and methods for http://www.bmj.com/ preventing recurrence. -

Acid-Base Abnormalities in Dogs with Diabetic Ketoacidosis: a Prospective Study of 60 Cases
325 Acid-base abnormalities in dogs with diabetic ketoacidosis: a prospective study of 60 cases Distúrbios ácido-base em cães com cetoacidose diabética: estudo prospectivo de 60 casos Ricardo DUARTE1; Denise Maria Nunes SIMÕES1; Khadine Kazue KANAYAMA1; Márcia Mery KOGIKA1 1School of Veterinary Medicine and Animal Science, University of São Paulo, São Paulo-SP, Brazil Abstract Diabetic ketoacidosis (DKA) is considered a typical high anion gap metabolic acidosis due to the retention of ketoanions. The objective of this study was to describe the acid-base disturbances of dogs with DKA and further characterize them, according to their frequency, adequacy of the secondary physiologic response, and occurrence of mixed disturbances. Sixty dogs with DKA were enrolled in the study. Arterial blood pH and gas tensions, plasma electrolytes, serum b-hydroxybutyrate (b-OHB), glucose, albumin and urea concentrations were determined for all dogs included in the study. All dogs were evaluated individually and systematically by the traditional approach to the diagnosis of acid- base disorders. Most of the dogs had a high anion gap acidosis, with appropriated respiratory response (n = 18; 30%) or concurrent respiratory alkalosis (n = 14; 23%). Hyperchloremic acidosis with moderated to marked increases in b-OHB was observed in 18 dogs (30%) and 7 of these patients had concurrent respiratory alkalosis. Hyperchloremic acidosis with mild increase in b-OHB was observed in 6 dogs (10%). Four dogs (7%) had a high anion gap acidosis with mild increase in b-OHB and respiratory alkalosis. Most of dogs with DKA had a high anion gap acidosis, but mixed acid-base disorders were common, chiefly high anion gap acidosis and concurrent respiratory alkalosis, and hyperchloremic acidosis with moderated to marked increases in serum b-OHB. -

Pathophysiology of Acid Base Balance: the Theory Practice Relationship
Intensive and Critical Care Nursing (2008) 24, 28—40 ORIGINAL ARTICLE Pathophysiology of acid base balance: The theory practice relationship Sharon L. Edwards ∗ Buckinghamshire Chilterns University College, Chalfont Campus, Newland Park, Gorelands Lane, Chalfont St. Giles, Buckinghamshire HP8 4AD, United Kingdom Accepted 13 May 2007 KEYWORDS Summary There are many disorders/diseases that lead to changes in acid base Acid base balance; balance. These conditions are not rare or uncommon in clinical practice, but every- Arterial blood gases; day occurrences on the ward or in critical care. Conditions such as asthma, chronic Acidosis; obstructive pulmonary disease (bronchitis or emphasaemia), diabetic ketoacidosis, Alkalosis renal disease or failure, any type of shock (sepsis, anaphylaxsis, neurogenic, cardio- genic, hypovolaemia), stress or anxiety which can lead to hyperventilation, and some drugs (sedatives, opoids) leading to reduced ventilation. In addition, some symptoms of disease can cause vomiting and diarrhoea, which effects acid base balance. It is imperative that critical care nurses are aware of changes that occur in relation to altered physiology, leading to an understanding of the changes in patients’ condition that are observed, and why the administration of some immediate therapies such as oxygen is imperative. © 2007 Elsevier Ltd. All rights reserved. Introduction the essential concepts of acid base physiology is necessary so that quick and correct diagnosis can The implications for practice with regards to be determined and appropriate treatment imple- acid base physiology are separated into respi- mented. ratory acidosis and alkalosis, metabolic acidosis The homeostatic imbalances of acid base are and alkalosis, observed in patients with differing examined as the body attempts to maintain pH bal- aetiologies. -

Persistent Lactic Acidosis - Think Beyond Sepsis Emily Pallister1* and Thogulava Kannan2
ISSN: 2377-4630 Pallister and Kannan. Int J Anesthetic Anesthesiol 2019, 6:094 DOI: 10.23937/2377-4630/1410094 Volume 6 | Issue 3 International Journal of Open Access Anesthetics and Anesthesiology CASE REPORT Persistent Lactic Acidosis - Think beyond Sepsis Emily Pallister1* and Thogulava Kannan2 1 Check for ST5 Anaesthetics, University Hospitals of Coventry and Warwickshire, UK updates 2Consultant Anaesthetist, George Eliot Hospital, Nuneaton, UK *Corresponding author: Emily Pallister, ST5 Anaesthetics, University Hospitals of Coventry and Warwickshire, Coventry, UK Introduction • Differential diagnoses for hyperlactatemia beyond sepsis. A 79-year-old patient with type 2 diabetes mellitus was admitted to the Intensive Care Unit for manage- • Remember to check ketones in patients taking ment of Acute Kidney Injury refractory to fluid resusci- Metformin who present with renal impairment. tation. She had felt unwell for three days with poor oral • Recovery can be protracted despite haemofiltration. intake. Admission bloods showed severe lactic acidosis and Acute Kidney Injury (AKI). • Suspect digoxin toxicity in patients on warfarin with acute kidney injury, who develop cardiac manifes- The patient was initially managed with fluid resus- tations. citation in A&E, but there was no improvement in her acid/base balance or AKI. The Intensive Care team were Case Description asked to review the patient and she was subsequently The patient presented to the Emergency Depart- admitted to ICU for planned haemofiltration. ment with a 3 day history of feeling unwell with poor This case presented multiple complex concurrent oral intake. On examination, her heart rate was 48 with issues. Despite haemofiltration, acidosis persisted for blood pressure 139/32. -

Evaluation and Treatment of Alkalosis in Children
Review Article 51 Evaluation and Treatment of Alkalosis in Children Matjaž Kopač1 1 Division of Pediatrics, Department of Nephrology, University Address for correspondence Matjaž Kopač, MD, DSc, Division of Medical Centre Ljubljana, Ljubljana, Slovenia Pediatrics, Department of Nephrology, University Medical Centre Ljubljana, Bohoričeva 20, 1000 Ljubljana, Slovenia J Pediatr Intensive Care 2019;8:51–56. (e-mail: [email protected]). Abstract Alkalosisisadisorderofacid–base balance defined by elevated pH of the arterial blood. Metabolic alkalosis is characterized by primary elevation of the serum bicarbonate. Due to several mechanisms, it is often associated with hypochloremia and hypokalemia and can only persist in the presence of factors causing and maintaining alkalosis. Keywords Respiratory alkalosis is a consequence of dysfunction of respiratory system’s control ► alkalosis center. There are no pathognomonic symptoms. History is important in the evaluation ► children of alkalosis and usually reveals the cause. It is important to evaluate volemia during ► chloride physical examination. Treatment must be causal and prognosis depends on a cause. Introduction hydrogen ion concentration and an alkalosis is a pathologic Alkalosis is a disorder of acid–base balance defined by process that causes a decrease in the hydrogen ion concentra- elevated pH of the arterial blood. According to the origin, it tion. Therefore, acidemia and alkalemia indicate the pH can be metabolic or respiratory. Metabolic alkalosis is char- abnormality while acidosis and alkalosis indicate the patho- acterized by primary elevation of the serum bicarbonate that logic process that is taking place.3 can result from several mechanisms. It is the most common Regulation of hydrogen ion balance is basically similar to form of acid–base balance disorders. -

Oral Rehydration of Adult Cattle Using Isotonic Solution of Sugar, Sodium Chloride and Potassium Chloride
Haryana Vet. (Dec., 2019) 58(2), 166-169 Research Article ABSTRACT Fig 2: Transmission electron photomicrograph of monocyte of dog Present study comprised of 72 crossbred cows (group I= 60 endometritic and group II=12 healthy) at 30±2days postpartum. The showing heterochromatin (a), euchromatin (b), cytoplasmic process (c), polymorphonuclear neutrophils (PMN) cell coun Vacuole and nuclear membrane. Uranyl acetate and lead citrate × 25500 Figure 1: Cyclic conditions for PCR profiling for detection of Salmonella genes ASSOCIATION OF SEMEN TRAITS IN CONSECUTIVE EJACULATES WITH FSH-β GENE POLYMORPHISM IN HOLSTEIN-FRIESIAN CROSSBRED BULLS FROM INDIA VIJAY KADAM, ABH trus synchronizathod that synchronizes ovulations is Corresponding author: [email protected] Fig. 1. Histogram depicting frequency distribution of animal named briefly as “Ovsynch” (Pursley et al., 1995). The right score of respondents Clinical Article study was aimed to evaluate the efficacy of different methods of estrus sync Fig. 1. Semilogarithmic plot of plasma concentration time profile of amoxicillin and cloxacillin following single dose (10 mg/kg) i.v. and i.m. administration in sheep (n=4) Haryana Vet. (Dec., 2019) 58(2), 166-169 Research Article 2003) which might lead to increased chances of urolith the time for the urinary tract to restore patency (Parrah, Haryana Vet. (March, 2020) 59(SI), 93-95 Short Communication Research Article formation. The increased hospital incidence can also be 2009) in conjugation with supportive treatments like COMPARATIVE EFFICACY OF SYNCHRONIZATION PROTOCOLS FOR IMPROVING attributed to the proximity of the clinic as well. According to peritoneal lavage, urinary acidifiers and urinary ORAL REHYDRATION OF ADULT CATTLE USING ISOTONIC SOLUTION OF SUGAR, FERTILITY IN POSTPARTUM CROSSBRED DAIRY COWS data published by Department ff Soil Science, Haryana, antiseptics. -

TITLE: Acid-Base Disorders PRESENTER: Brenda Suh-Lailam
TITLE: Acid-Base Disorders PRESENTER: Brenda Suh-Lailam Slide 1: Hello, my name is Brenda Suh-Lailam. I am an Assistant Director of Clinical Chemistry and Mass Spectrometry at Ann & Robert H. Lurie Children’s Hospital of Chicago, and an Assistant Professor of Pathology at Northwestern Feinberg School of Medicine. Welcome to this Pearl of Laboratory Medicine on “Acid-Base Disorders.” Slide 2: During metabolism, the body produces hydrogen ions which affect metabolic processes if concentration is not regulated. To maintain pH within physiologic limits, there are several buffer systems that help regulate hydrogen ion concentration. For example, bicarbonate, plasma proteins, and hemoglobin buffer systems. The bicarbonate buffer system is the major buffer system in the blood. Slide 3: In the bicarbonate buffer system, bicarbonate, which is the metabolic component, is controlled by the kidneys. Carbon dioxide is the respiratory component and is controlled by the lungs. Changes in the respiratory and metabolic components, as depicted here, can lead to a decrease in pH termed acidosis, or an increase in pH termed alkalosis. Slide 4: Because the bicarbonate buffer system is the major buffer system of blood, estimation of pH using the Henderson-Hasselbalch equation is usually performed, expressed as a ratio of bicarbonate and carbon dioxide. Where pKa is the pH at which the concentration of protonated and unprotonated species are equal, and 0.0307 is the solubility coefficient of carbon dioxide. Four variables are present in this equation; knowing three variables allows for calculation of the fourth. Since pKa is a constant, and pH and carbon dioxide are measured during blood gas analysis, bicarbonate can, therefore, be determined using this equation. -
Unit 4 Acid-Base Homeostasis
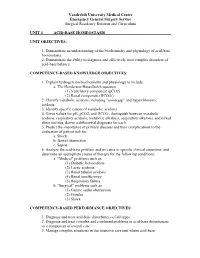
Vanderbilt University Medical Center Emergency General Surgery Service Surgical Residency Rotation and Curriculum UNIT 4 ACID-BASE HOMEOSTASIS UNIT OBJECTIVES: 1. Demonstrate an understanding of the biochemistry and physiology of acid-base homeostasis. 2. Demonstrate the ability to diagnose and effectively treat complex disorders of acid-base balance. COMPETENCY-BASED KNOWLEDGE OBJECTIVES: 1. Explain hydrogen ion biochemistry and physiology to include: a. The Henderson-Hasselbalch equation (1) Ventilatory component (pCO2) (2) Renal component (HCO3-) 2. Classify metabolic acidosis, including "anion gap" and hyperchloremic acidosis. 3. Identify specific causes of metabolic acidosis. 4. Given values for pH, pCO2, and HCO3-, distinguish between metabolic acidosis, respiratory acidosis, metabolic alkalosis, respiratory alkalosis, and mixed abnormalities; derive a differential diagnosis for each. 5. Predict the importance of primary diseases and their complications to the evaluation of patient risk for: a. Shock b. Bowel obstruction c. Sepsis 6. Analyze the acid-base problem and its cause in specific clinical situations, and determine an appropriate course of therapy for the following conditions: a. "Medical" problems such as: (1) Diabetic ketoacidosis (2) Lactic acidosis (3) Renal tubular acidosis (4) Renal insufficiency (5) Respiratory failure b. "Surgical" problems such as: (1) Gastric outlet obstruction (2) Fistulas (3) Shock COMPETENCY-BASED PERFORMANCE OBJECTIVES: 1. Diagnose and treat acid-base disturbances of all types. 2. Diagnose and treat complex and combined problems in acid-base disturbances as a component of overall care. 3. Manage complex situations in the intensive care unit where acid-base Vanderbilt University Medical Center Emergency General Surgery Service Surgical Residency Rotation and Curriculum abnormalities coexist with other metabolic derangements, including: a. -

Lecture-1 Keto Acidosis, Bovine Ketosis, Ovine Pregnancy Toxemia
Lecture-1 Keto acidosis Ketoacidosis is a metabolic acidosis due to an excessive blood concentration of ketone bodies (acetone, acetoacetate and beta-hydroxybutyrate). Ketone bodies are released into the blood from the liver when hepatic lipid metabolism has changed to a state of increased ketogenesis. The abnormal accumulation of ketones in the body occurs due to excessive breakdown of fats in deficiency or inadequate use of carbohydrates. It is characterized by ketonuria, loss of potassium in the urine, and a fruity odor of acetone on the breath. Untreated, ketosis may progress to ketoacidosis, coma, and death. This condition is seen in starvation, occasionally in pregnancy if the intake of protein and carbohydrates is inadequate, and most frequently in diabetes mellitus. Different Types of Ketoacidosis Diabetes Keto Acidosis (DKA): Due to lack of insulin glucose uptake and metabolism by cells is decrased.Fatty acid catabolism increased in resulting in excess production of ketone bodies. Starvation Ketosis: Starvation leads to hypoglycemia as there is little or no absorption of glucose from intestine and also due to depletion of liver glycogen. In Fatty acid oxidation leads to excess ketone body. Bovine Ketosis Introduction Bovine ketosis occurs in the high producing dairy cows during the early stages of lactation, when the milk production is generally the highest. Abnormally high levels of the ketone bodies, acetone, acetoacetic and beta-hydroxy butyric acid and also iso- propanol appear in blood, urine and in milk. The alterations are accompanied by loss of appetite , weight loss, decrease in milk production and nervous disturbances. Hypoglycemia (starvation) is a common finding in bovine ketosis and in ovine pregnancy toxemia. -

Package Insert Template for Oral Rehydration Salt (Ors)
PACKAGE INSERT TEMPLATE FOR ORAL REHYDRATION SALT (ORS) Brand or Product Name [Product name] Powder for Oral Solution [Product name] Liquid in the form of solution/suspension Name and Strength of Active Substance(s) Sodium chloride ………………(12.683% w/v) Glucose, anhydrous…………...(65.854% w/v) Potassium chloride………...…...(7.317% w/v) Trisodium citrate, dihydrate ….(14.146% w/v) Product Description [Visual description of the appearance of the product (eg colour etc)] Eg:A white to off-white colour granules, when dissolved in water, forms an orange colour solution. Pharmacodynamics The reconstituted solution contains a mixture of sodium and potassium salts along with glucose, which facilitates the absorption of sodium and potassium from the intestine. Water is drawn from the bowel by the osmotic effect. As well as “drying up” the stools, the dehydration and loss of electrolytes caused by the diarrhoea is corrected by the water and electrolytes absorbed. Pharmacokinetics Glucose After oral administration glucose is completely absorbed by a sodium dependent uptake mechanism exhibiting saturation kinetics. Blood levels return to normal within two hours of ingestion. Potassium Chloride No specific control mechanisms limit absorption of potassium, which is usually complete. Potassium is excreted largely by the kidneys, though 10% is excreted by the colonic mucosa. Potassium excretion is reduced in patients with renal impairment and in the elderly, so extreme caution should be used in treating such patients with potassium salts. Sodium Bicarbonate Kinetics are determined by the physiological state of the patient at the time. Sodium Chloride Readily absorbed from the gastrointestinal tract. Gut absorption, particularly in the jejunum is enhanced by the addition of glucose. -

Diabetic Ketoalkalosis in Children and Adults
Original Article Diabetic Ketoalkalosis in Children and Adults Emily A. Huggins, MD, Shawn A. Chillag, MD, Ali A. Rizvi, MD, Robert R. Moran, PhD, and Martin W. Durkin, MD, MPH and DR are calculated because the pH and bicarbonate may be near Objectives: Diabetic ketoacidosis (DKA) with metabolic alkalosis normal or even elevated. In addition to having interesting biochemical (diabetic ketoalkalosis [DKALK]) in adults has been described in the features as a complex acid-base disorder, DKALK can pose diagnostic literature, but not in the pediatric population. The discordance in the and/or therapeutic challenges. change in the anion gap (AG) and the bicarbonate is depicted by an Key Words: delta ratio, diabetic ketoacidosis, diabetic ketoalkalosis, elevated delta ratio (DR; rise in AG/drop in bicarbonate), which is metabolic alkalosis normally approximately 1. The primary aim of this study was to de- termine whether DKALK occurs in the pediatric population, as has been seen previously in the adult population. The secondary aim was iabetic ketoacidosis (DKA), a common and serious dis- to determine the factors that may be associated with DKALK. Dorder that almost always results in hospitalization, is de- Methods: A retrospective analysis of adult and pediatric cases with a fined by the presence of hyperglycemia, reduced pH, metabolic 1 primary or secondary discharge diagnosis of DKA between May 2008 and acidosis, elevated anion gap (AG), and serum or urine ketones. August 2010 at a large urban hospital was performed. DKALK was as- In some situations, a metabolic alkalosis coexists with DKA sumedtobepresentiftheDRwas91.2 or in cases of elevated bicarbonate. -

Acid-Base Physiology & Anesthesia
ACID-BASE PHYSIOLOGY & ANESTHESIA Lyon Lee DVM PhD DACVA Introductions • Abnormal acid-base changes are a result of a disease process. They are not the disease. • Abnormal acid base disorder predicts the outcome of the case but often is not a direct cause of the mortality, but rather is an epiphenomenon. • Disorders of acid base balance result from disorders of primary regulating organs (lungs or kidneys etc), exogenous drugs or fluids that change the ability to maintain normal acid base balance. • An acid is a hydrogen ion or proton donor, and a substance which causes a rise in H+ concentration on being added to water. • A base is a hydrogen ion or proton acceptor, and a substance which causes a rise in OH- concentration when added to water. • Strength of acids or bases refers to their ability to donate and accept H+ ions respectively. • When hydrochloric acid is dissolved in water all or almost all of the H in the acid is released as H+. • When lactic acid is dissolved in water a considerable quantity remains as lactic acid molecules. • Lactic acid is, therefore, said to be a weaker acid than hydrochloric acid, but the lactate ion possess a stronger conjugate base than hydrochlorate. • The stronger the acid, the weaker its conjugate base, that is, the less ability of the base to accept H+, therefore termed, ‘strong acid’ • Carbonic acid ionizes less than lactic acid and so is weaker than lactic acid, therefore termed, ‘weak acid’. • Thus lactic acid might be referred to as weak when considered in relation to hydrochloric acid but strong when compared to carbonic acid.