Persistent Lactic Acidosis - Think Beyond Sepsis Emily Pallister1* and Thogulava Kannan2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diabetic Ketoacidosis and Hyperosmolar BMJ: First Published As 10.1136/Bmj.L1114 on 29 May 2019
STATE OF THE ART REVIEW Diabetic ketoacidosis and hyperosmolar BMJ: first published as 10.1136/bmj.l1114 on 29 May 2019. Downloaded from hyperglycemic syndrome: review of acute decompensated diabetes in adult patients Esra Karslioglu French,1 Amy C Donihi,2 Mary T Korytkowski1 1Division of Endocrinology and Metabolism, Department of ABSTRACT Medicine, University of Pittsburgh, Pittsburgh, PA, USA Diabetic ketoacidosis and hyperosmolar hyperglycemic syndrome (HHS) are life threatening 2University of Pittsburgh School of complications that occur in patients with diabetes. In addition to timely identification of the Pharmacy, Pittsburgh, PA, USA Correspondence to: M Korytkowski precipitating cause, the first step in acute management of these disorders includes aggressive [email protected] administration of intravenous fluids with appropriate replacement of electrolytes (primarily Cite this as: BMJ 2019;365:l1114 doi: 10.1136/bmj.l1114 potassium). In patients with diabetic ketoacidosis, this is always followed by administration Series explanation: State of the of insulin, usually via an intravenous insulin infusion that is continued until resolution of Art Reviews are commissioned on the basis of their relevance to ketonemia, but potentially via the subcutaneous route in mild cases. Careful monitoring academics and specialists in the US and internationally. For this reason by experienced physicians is needed during treatment for diabetic ketoacidosis and HHS. they are written predominantly by Common pitfalls in management include premature termination of intravenous insulin US authors therapy and insufficient timing or dosing of subcutaneous insulin before discontinuation of intravenous insulin. This review covers recommendations for acute management of diabetic ketoacidosis and HHS, the complications associated with these disorders, and methods for http://www.bmj.com/ preventing recurrence. -

Cardiac Dysfunction and Lactic Acidosis During Hyperdynamic and Hypovolemic Shock
è - \-o(J THESIS FOR TIIE DEGREE OF DOCTOR OF MEDICINE CARDIAC DYSFUNCTION AND LACTIC ACIDOSIS DURING HYPERDYNAMIC AND HYPOVOLEMIC SHOCK DAVID JAMES COOPER DEPARTMENT OF ANAESTIIESIA AND INTENSIVE CARE FACULTY OF MEDICINE UNIVERSITY OF ADELAIDE Submitted: October,1995 Submitted in revised form: November, 1996 2 J TABLE OF CONTENTS Page 5 CH 1(1.1) Abstract (1.2) Signed statement (1.3) Authors contribution to each publication (1.4) Acknowledgments (1.5) Publications arising 9 CH2Introduction (2.1) Shock and lactic acidosis (2.2) Cardiac dysfunction and therapies during lactic acidosis (2.3) Cardiac dysfunction during hyperdynamic shock (2.4) Cardiac dysfunction during hypovolemic shock (2.5) Cardiac dysfunction during ionised hypocalcaemia l7 CH3 Methods (3. 1) Left ventricular function assessment - introduction (3.2) Left ventricular function assessment in an animal model 3.2.I Introduction 3.2.2 Anaesthesia 3.2.3 Instrumentation 3.2.4 Systolic left ventricular contractility 3.2.5 Left ventricular diastolic mechanics 3.2.6 Yentricular function curves 3.2.1 Limitations of the animal model (3.3) Left ventricular function assessment in human volunteers 3.3.7 Left ventricular end-systolic pressure measurement 3.3.2 Left ventricular dimension measurement 3.3.3 Rate corrected velocity of circumferential fibre shortening (v"¡.) 3.3.4. Left ventricular end-systolic meridional wall stress (o"r) 4 33 CH 4 Cardiac dysfunction during lactic acidosis (4.1) Introduction 4.7.1 Case report (4.2) Human studies 4.2.1 Bicarbonate in critically ill patients -
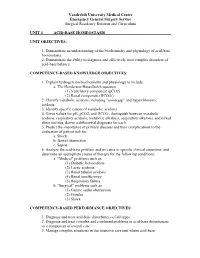
Unit 4 Acid-Base Homeostasis
Vanderbilt University Medical Center Emergency General Surgery Service Surgical Residency Rotation and Curriculum UNIT 4 ACID-BASE HOMEOSTASIS UNIT OBJECTIVES: 1. Demonstrate an understanding of the biochemistry and physiology of acid-base homeostasis. 2. Demonstrate the ability to diagnose and effectively treat complex disorders of acid-base balance. COMPETENCY-BASED KNOWLEDGE OBJECTIVES: 1. Explain hydrogen ion biochemistry and physiology to include: a. The Henderson-Hasselbalch equation (1) Ventilatory component (pCO2) (2) Renal component (HCO3-) 2. Classify metabolic acidosis, including "anion gap" and hyperchloremic acidosis. 3. Identify specific causes of metabolic acidosis. 4. Given values for pH, pCO2, and HCO3-, distinguish between metabolic acidosis, respiratory acidosis, metabolic alkalosis, respiratory alkalosis, and mixed abnormalities; derive a differential diagnosis for each. 5. Predict the importance of primary diseases and their complications to the evaluation of patient risk for: a. Shock b. Bowel obstruction c. Sepsis 6. Analyze the acid-base problem and its cause in specific clinical situations, and determine an appropriate course of therapy for the following conditions: a. "Medical" problems such as: (1) Diabetic ketoacidosis (2) Lactic acidosis (3) Renal tubular acidosis (4) Renal insufficiency (5) Respiratory failure b. "Surgical" problems such as: (1) Gastric outlet obstruction (2) Fistulas (3) Shock COMPETENCY-BASED PERFORMANCE OBJECTIVES: 1. Diagnose and treat acid-base disturbances of all types. 2. Diagnose and treat complex and combined problems in acid-base disturbances as a component of overall care. 3. Manage complex situations in the intensive care unit where acid-base Vanderbilt University Medical Center Emergency General Surgery Service Surgical Residency Rotation and Curriculum abnormalities coexist with other metabolic derangements, including: a. -

Lecture-1 Keto Acidosis, Bovine Ketosis, Ovine Pregnancy Toxemia
Lecture-1 Keto acidosis Ketoacidosis is a metabolic acidosis due to an excessive blood concentration of ketone bodies (acetone, acetoacetate and beta-hydroxybutyrate). Ketone bodies are released into the blood from the liver when hepatic lipid metabolism has changed to a state of increased ketogenesis. The abnormal accumulation of ketones in the body occurs due to excessive breakdown of fats in deficiency or inadequate use of carbohydrates. It is characterized by ketonuria, loss of potassium in the urine, and a fruity odor of acetone on the breath. Untreated, ketosis may progress to ketoacidosis, coma, and death. This condition is seen in starvation, occasionally in pregnancy if the intake of protein and carbohydrates is inadequate, and most frequently in diabetes mellitus. Different Types of Ketoacidosis Diabetes Keto Acidosis (DKA): Due to lack of insulin glucose uptake and metabolism by cells is decrased.Fatty acid catabolism increased in resulting in excess production of ketone bodies. Starvation Ketosis: Starvation leads to hypoglycemia as there is little or no absorption of glucose from intestine and also due to depletion of liver glycogen. In Fatty acid oxidation leads to excess ketone body. Bovine Ketosis Introduction Bovine ketosis occurs in the high producing dairy cows during the early stages of lactation, when the milk production is generally the highest. Abnormally high levels of the ketone bodies, acetone, acetoacetic and beta-hydroxy butyric acid and also iso- propanol appear in blood, urine and in milk. The alterations are accompanied by loss of appetite , weight loss, decrease in milk production and nervous disturbances. Hypoglycemia (starvation) is a common finding in bovine ketosis and in ovine pregnancy toxemia. -

Diabetic Ketoalkalosis in Children and Adults
Original Article Diabetic Ketoalkalosis in Children and Adults Emily A. Huggins, MD, Shawn A. Chillag, MD, Ali A. Rizvi, MD, Robert R. Moran, PhD, and Martin W. Durkin, MD, MPH and DR are calculated because the pH and bicarbonate may be near Objectives: Diabetic ketoacidosis (DKA) with metabolic alkalosis normal or even elevated. In addition to having interesting biochemical (diabetic ketoalkalosis [DKALK]) in adults has been described in the features as a complex acid-base disorder, DKALK can pose diagnostic literature, but not in the pediatric population. The discordance in the and/or therapeutic challenges. change in the anion gap (AG) and the bicarbonate is depicted by an Key Words: delta ratio, diabetic ketoacidosis, diabetic ketoalkalosis, elevated delta ratio (DR; rise in AG/drop in bicarbonate), which is metabolic alkalosis normally approximately 1. The primary aim of this study was to de- termine whether DKALK occurs in the pediatric population, as has been seen previously in the adult population. The secondary aim was iabetic ketoacidosis (DKA), a common and serious dis- to determine the factors that may be associated with DKALK. Dorder that almost always results in hospitalization, is de- Methods: A retrospective analysis of adult and pediatric cases with a fined by the presence of hyperglycemia, reduced pH, metabolic 1 primary or secondary discharge diagnosis of DKA between May 2008 and acidosis, elevated anion gap (AG), and serum or urine ketones. August 2010 at a large urban hospital was performed. DKALK was as- In some situations, a metabolic alkalosis coexists with DKA sumedtobepresentiftheDRwas91.2 or in cases of elevated bicarbonate. -

Acid-Base Physiology & Anesthesia
ACID-BASE PHYSIOLOGY & ANESTHESIA Lyon Lee DVM PhD DACVA Introductions • Abnormal acid-base changes are a result of a disease process. They are not the disease. • Abnormal acid base disorder predicts the outcome of the case but often is not a direct cause of the mortality, but rather is an epiphenomenon. • Disorders of acid base balance result from disorders of primary regulating organs (lungs or kidneys etc), exogenous drugs or fluids that change the ability to maintain normal acid base balance. • An acid is a hydrogen ion or proton donor, and a substance which causes a rise in H+ concentration on being added to water. • A base is a hydrogen ion or proton acceptor, and a substance which causes a rise in OH- concentration when added to water. • Strength of acids or bases refers to their ability to donate and accept H+ ions respectively. • When hydrochloric acid is dissolved in water all or almost all of the H in the acid is released as H+. • When lactic acid is dissolved in water a considerable quantity remains as lactic acid molecules. • Lactic acid is, therefore, said to be a weaker acid than hydrochloric acid, but the lactate ion possess a stronger conjugate base than hydrochlorate. • The stronger the acid, the weaker its conjugate base, that is, the less ability of the base to accept H+, therefore termed, ‘strong acid’ • Carbonic acid ionizes less than lactic acid and so is weaker than lactic acid, therefore termed, ‘weak acid’. • Thus lactic acid might be referred to as weak when considered in relation to hydrochloric acid but strong when compared to carbonic acid. -

Diabetic Ketoacidosis: Evaluation and Treatment DYANNE P
Diabetic Ketoacidosis: Evaluation and Treatment DYANNE P. WESTERBERG, DO, Cooper Medical School of Rowan University, Camden, New Jersey Diabetic ketoacidosis is characterized by a serum glucose level greater than 250 mg per dL, a pH less than 7.3, a serum bicarbonate level less than 18 mEq per L, an elevated serum ketone level, and dehydration. Insulin deficiency is the main precipitating factor. Diabetic ketoacidosis can occur in persons of all ages, with 14 percent of cases occurring in persons older than 70 years, 23 percent in persons 51 to 70 years of age, 27 percent in persons 30 to 50 years of age, and 36 percent in persons younger than 30 years. The case fatality rate is 1 to 5 percent. About one-third of all cases are in persons without a history of diabetes mellitus. Common symptoms include polyuria with polydipsia (98 percent), weight loss (81 percent), fatigue (62 percent), dyspnea (57 percent), vomiting (46 percent), preceding febrile illness (40 percent), abdominal pain (32 percent), and polyphagia (23 percent). Measurement of A1C, blood urea nitro- gen, creatinine, serum glucose, electrolytes, pH, and serum ketones; complete blood count; urinalysis; electrocar- diography; and calculation of anion gap and osmolar gap can differentiate diabetic ketoacidosis from hyperosmolar hyperglycemic state, gastroenteritis, starvation ketosis, and other metabolic syndromes, and can assist in diagnosing comorbid conditions. Appropriate treatment includes administering intravenous fluids and insulin, and monitoring glucose and electrolyte levels. Cerebral edema is a rare but severe complication that occurs predominantly in chil- dren. Physicians should recognize the signs of diabetic ketoacidosis for prompt diagnosis, and identify early symp- toms to prevent it. -

Diabetic Ketoacidosis Diabetic Ketoacidosis (DKA) Is a Serious Problem That Can Happen in People with Diabetes
Diabetic Ketoacidosis Diabetic ketoacidosis (DKA) is a serious problem that can happen in people with diabetes. DKA should be treated as a medical emergency. This is because it can lead to coma or death. If you have the symptoms of DKA, get medical help right away. DKA happens more often in people with type 1 diabetes. But it can happen in people with type 2 diabetes. It can also happen in women with diabetes during pregnancy (gestational diabetes). DKA happens when insulin levels are too low. Without enough insulin, sugar (glucose) can’t get to the cells of your body. The glucose stays in the blood. The liver then puts out even more glucose into the blood. This causes high blood glucose (hyperglycemia). Without glucose, your body breaks down stored fat for energy. When this happens, acids called ketones are released into the blood. This is called ketosis. High levels of ketones (ketoacidosis) can be harmful to you. Hyperglycemia and ketoacidosis can also cause serious problems in the blood and your body, such as: • Low levels of potassium (hypokalemia) and phosphate • Damage to kidneys or other organs • Coma What causes diabetic ketoacidosis? In people with diabetes, DKA is most often caused by too little insulin in the body. It is also caused by: • Poor management of diabetes • Infections such as a urinary tract infection or pneumonia • Serious health problems, such as a heart attack • Reactions to certain prescribed medicines including SGLT2 inhibitors for treating type 2 diabetes • Reactions to illegal drugs including cocaine • Disruption of insulin delivery from an insulin pump Symptoms of diabetic ketoacidosis DKA most often happens slowly over time. -

Internationaljournalo Fnutrition
Freely Available Online INTERNATIONAL JOURNAL OF NUTRITION ISSN NO: 2379-7835 Review DOI: 10.14302/issn.2379-7835.ijn-20-3159 Pyruvate Research and Clinical Application Outlooks A Revolutionary Medical Advance Zhou Fang-Qiang1,* 1Shanghai Sandai Pharmaceutical R&D Co. Ltd., Shanghai, 200127 China Abstract Pyruvate holds superior biomedical properties in increase of hypoxia tolerance, correction of severe acidosis, exertion of anti-oxidative stress and protection of mitochondria against apoptosis, so that it improves multi-organ function in various pathogenic insults. Particularly, pyruvate preserves key enzyme: pyruvate dehydrogenase (PDH) activity through direct inhibition of pyruvate dehydrogenase kinas (PDK), as a PDH activator, in hypoxia. Therefore, pyruvate is robustly beneficial for cell/organ function over citrate, acetate, lactate, bicarbonate and chloride as anions in current medical fluids. Pyruvate-enriched oral rehydration salt/solution (Pyr-ORS) and pyruvate-based intravenous (IV) fluids would be more beneficial than WHO-ORS and current IV fluids in both crystalloids and colloids, respectively. Pyruvate-containing fluids as the new generation would be not only a volume expander, but also a therapeutic agent simultaneously in fluid resuscitation in critical care patients. Pyruvate may be also beneficial in prevent and treatment of diabetes, aging and even cancer. Pyruvate clinical applications indicates a new revolutionary medical advance, following the WHO-ORS prevalence, this century. Corresponding author: Zhou FQ, Shanghai Sandai Pharmaceutical R&D Co., Ltd., Shanghai, 200127 China; current address: 200 W. Sahara Ave, Unit 604, Las Vegas, NV 89102 USA; Tel: 1-708-785-3568. Running title: Pyruvate in medical advance Keywords: Aging, Cancer, Diabetes, Fluid Therapy, Hypoxic Lactic Acidosis, Oral Rehydration Salt, Pyruvate, Resuscitation Received: Jan 01, 2020 Accepted: Jan 07, 2020 Published: Jan 14, 2020 Editor: Godwin Ajayi, Prenatal Diagnosis and Therapy Centre, College of Medicine, University of Lagos, Nigeria. -

The Role of Bicarbonate and Base Precursors in Treatment of Acute Gastroenteritis
Arch Dis Child: first published as 10.1136/adc.62.1.91 on 1 January 1987. Downloaded from Archives of Disease in Childhood, 1987, 62, 91-95 Current topic The role of bicarbonate and base precursors in treatment of acute gastroenteritis E J ELLIOTT, J A WALKER-SMITH, AND M J G FARTHING Departments of Child Health and Gastroenterology, St Bartholomew's Hospital, London Widespread use of oral glucose-electrolyte rehydra- tion as to whether rehydration with base was tion solutions (ORS) has resulted in a dramatic superior to rehydration with saline alone. decrease in the morbidity and mortality associated The use of parenteral bicarbonate was not without with childhood gastroenteritis, regardless of its its problems. In the 1940s Rapoport et al recom- aetiology. Nevertheless, diarrhoeal disease remains mended vigorous rehydration with saline containing the most common cause of death of children in sodium bicarbonate but without potassium and developing countries, and current research efforts reported a 'post-acidotic state' in children whose are directed towards optimising the efficacy of ORS, diarrhoea had improved and in whom recovery aiming for both simplicity and economy. Con- seemed imminent. The clinical syndrome he de- troversy regarding the 'ideal' sodium and glucose scribed of lethargy, irritability, abnormal cardiac concentration continues to the extent that different function, intracranial haemorrhage, generalised copyright. formulations are now recommended in the develop- oedema, and tetany can be attributed to the ing and industrialised world. The inclusion of alkalosis and electrolyte disturbance (hypoka- bicarbonate or a base precursor (citrate, acetate, or laemia, hypocalcaemia, hypophosphataemia, and lactate) in ORS is generally assumed to be neces- hypernatraemia) after excessive rapid administra- sary, both for promotion of water and sodium tion of sodium and alkali. -

Observations Compensatory Hypochloraemic Alkalosis In
Letters 871 tended to the DQ-LTR13 integration, where we also find a con- 2. Pascual M, Martin J, Nieto A et al. (2001) Distribution of tribution of DQ-LTR13 to RA susceptibility in DQ8-positive HERV-LTR elements in the 5′-flanking region of HLA- individuals. Furthermore we recently published that patients DQB1 and association with autoimmunity. Immunogenetics with Addison’s disease—another HLA DQ8-associated autoim- 53:114–118 mune disease of the adrenals which may occur in combination 3. Donner H, Tonjes RR, Bontrop RE et al. (1999) Intronic se- with Type 1 diabetes as part of the autoimmune pluriglandular quence motifs of HLA-DQB1 are shared between humans, syndrome Type 2—have more often the DQ8-DQ-LTR13 com- apes and Old World monkeys, but a retroviral LTR element bination in contrast to the DQ-LTR3 insertion. Although both (DQLTR3) is human specific. Tissue Antigens 53:551–558 DQ-LTR3 and DQ-LTR13 are linked to DQ8, DQ-LTR13 en- 4. Donner H, Tonjes RR, Van der Auwera B et al. (1999) The hances the risk for Addison’s disease [7]. presence or absence of a retroviral long terminal repeat Whether DQ-LTR13 has a functional significance or not is influences the genetic risk for type 1 diabetes conferred by currently under investigation. Preliminary data indicate that human leukocyte antigen DQ haplotypes. J Clin Endocrinol DQ-LTR13 harbours regulatory capacity and shows functional Metab 84:1404–1408 activity of an upstream element as revealed by analyses of nu- 5. Seidl C, Donner H, Petershofen E et al. -

Lactic Acidosis Update for Critical Care Clinicians
J Am Soc Nephrol 12: S15–S19, 2001 Lactic Acidosis Update for Critical Care Clinicians FRIEDRICH C. LUFT Franz Volhard Clinic and Max Delbrück Center for Molecular Medicine, Medical Faculty of the Charité Humboldt University of Berlin, Berlin, Germany. Abstract. Lactic acidosis is a broad-anion gap metabolic aci- involves patients with underlying severe renal and cardiac dosis caused by lactic acid overproduction or underutilization. dysfunction. Drugs used to treat lactic acidosis can aggravate The quantitative dimensions of these two mechanisms com- the condition. NaHCO3 increases lactate production. Treatment monly differ by 1 order of magnitude. Overproduction of lactic of type A lactic acidosis is particularly unsatisfactory. acid, also termed type A lactic acidosis, occurs when the body NaHCO3 is of little value. Carbicarb is a mixture of Na2CO3 must regenerate ATP without oxygen (tissue hypoxia). Circu- and NaHCO3 that buffers similarly to NaHCO3 but without net latory, pulmonary, or hemoglobin transfer disorders are com- generation of CO2. The results from animal studies are prom- monly responsible. Overproduction of lactate also occurs with ising; however, clinical trials are sparse. Dichloroacetate stim- cyanide poisoning or certain malignancies. Underutilization ulates pyruvate dehydrogenase and improves laboratory val- involves removal of lactic acid by oxidation or conversion to ues, but unfortunately not survival rates, among patients with glucose. Liver disease, inhibition of gluconeogenesis, pyruvate lactic acidosis. Hemofiltration has been advocated for the dehydrogenase (thiamine) deficiency, and uncoupling of oxi- treatment of lactic acidosis, on the basis of anecdotal experi- dative phosphorylation are the most common causes. The ences. However, kinetic studies of lactate removal do not kidneys also contribute to lactate removal.