Chapter Iii Surgery: Integumentary System Cpt Codes 10000-19999 for National Correct Coding Initiative Policy Manual for Medicare Services
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CPT® New Codes 2019: Biopsy, Skin
Billing and Coding Update Alexander Miller, M.D. AAD Representative to the AMA CPT Advisory Committee New Skin Biopsy CPT® Codes It’s all about the Technique! SPEAKER: Alexander Miller, M.D. AAD Representative to the AMA -CPT Advisory Committee Chair AAD Health Care Finance Committee Arriving on January 1, 2019 New and Restructured Biopsy Codes Tangential biopsy Punch Biopsy Incisional Biopsy How Did We Get Here? CMS CY 2016 Biopsy codes (11100, 11101 identified as potentially mis-valued; high expenditure RUC Survey sent to AAD Members Specialty survey results are the only tool available to support code values Challenging survey results Survey revealed bimodal data distribution; CPT Codes 11100, 11101 referred to CPT for respondents were valuing different procedures restructuring Rationale for New Codes 11100; 11101 • Previous skin biopsy codes did not distinguish between the different biopsy techniques that were being used CPT Recommended technique specification in new biopsy codes • Will also provide for reimbursement commensurate with the technique used How Did We Get Here? • CPT Editorial Panel deleted 11100; 11101 February 2017 • 6 New codes created based on technique utilized • Each technique: primary code and add-on code March 2017 • RUC survey sent to AAD members April 2017 • Survey results presented to the RUC Biopsy Codes Effective Jan., 1, 2019 • Integumentary biopsy codes 11755 Biopsy of nail unit (plate, bed, matrix, hyponychium, proximal and lateral nail folds 11100, 11101 have been deleted 30100 Biopsy, intranasal • New -

ANMC Specialty Clinic Services
Cardiology Dermatology Diabetes Endocrinology Ear, Nose and Throat (ENT) Gastroenterology General Medicine General Surgery HIV/Early Intervention Services Infectious Disease Liver Clinic Neurology Neurosurgery/Comprehensive Pain Management Oncology Ophthalmology Orthopedics Orthopedics – Back and Spine Podiatry Pulmonology Rheumatology Urology Cardiology • Cardiology • Adult transthoracic echocardiography • Ambulatory electrocardiology monitor interpretation • Cardioversion, electrical, elective • Central line placement and venous angiography • ECG interpretation, including signal average ECG • Infusion and management of Gp IIb/IIIa agents and thrombolytic agents and antithrombotic agents • Insertion and management of central venous catheters, pulmonary artery catheters, and arterial lines • Insertion and management of automatic implantable cardiac defibrillators • Insertion of permanent pacemaker, including single/dual chamber and biventricular • Interpretation of results of noninvasive testing relevant to arrhythmia diagnoses and treatment • Hemodynamic monitoring with balloon flotation devices • Non-invasive hemodynamic monitoring • Perform history and physical exam • Pericardiocentesis • Placement of temporary transvenous pacemaker • Pacemaker programming/reprogramming and interrogation • Stress echocardiography (exercise and pharmacologic stress) • Tilt table testing • Transcutaneous external pacemaker placement • Transthoracic 2D echocardiography, Doppler, and color flow Dermatology • Chemical face peels • Cryosurgery • Diagnosis -

A Clinical and Histological Study of Radiofrequency-Assisted Liposuction (RFAL) Mediated Skin Tightening and Cellulite Improvement ——RFAL for Skin Tightening
Journal of Cosmetics, Dermatological Sciences and Applications, 2011, 1, 36-42 doi:10.4236/jcdsa.2011.12006 Published Online June 2011 (http://www.SciRP.org/journal/jcdsa) A Clinical and Histological Study of Radiofrequency-Assisted Liposuction (RFAL) Mediated Skin Tightening and Cellulite Improvement ——RFAL for Skin Tightening Marc Divaris1, Sylvie Boisnic2, Marie-Christine Branchet2, Malcolm D. Paul3 1Plastic and Maxillo-Facial Surgery, University of Pitie Salpetiere, Paris, France; 2Institution GREDECO, Paris, France; 3Department of Surgery, Aesthetic and PlasticSurgery Institute, University of California, Irvine, USA. Email: [email protected] Received May 1st, 2011; revised May 27th, 2011; accepted June 6th, 2011. ABSTRACT Background: A novel Radiofrequency-Assisted Liposuction (RFAL) technology was evaluated clinically. Parallel origi- nal histological studies were conducted to substantiate the technology’s efficacy in skin tightening, and cellulite im- provement. Methods: BodyTiteTM system, utilizing the RFAL technology, was used for treating patients on abdomen, hips, flanks and arms. Clinical results were measured on 53 patients up to 6 months follow-up. Histological and bio- chemical studies were conducted on 10 donors by using a unique GREDECO model of skin fragments cultured under survival conditions. Fragments from RFAL treated and control areas were examined immediately and after 10 days in culture, representing long-term results. Skin fragments from patients with cellulite were also examined. Results: Grad- ual improvement in circumference reduction (3.9 - 4.9 cm) and linear contraction (8% - 38%) was observed until the third month. These results stabilized at 6 months. No adverse events were recorded. Results were graded as excellent by most patients, including the satisfaction from minimal pain, bleeding, and downtime. -

Co™™I™™Ee Opinion
The American College of Obstetricians and Gynecologists WOMEN’S HEALTH CARE PHYSICIANS COMMITTEE OPINION Number 673 • September 2016 (Replaces Committee Opinion No. 345, October 2006) Committee on Gynecologic Practice This Committee Opinion was developed by the American College of Obstetricians and Gynecologists’ Committee on Gynecologic Practice and the American Society for Colposcopy and Cervical Pathology (ASCCP) in collaboration with committee member Ngozi Wexler, MD, MPH, and ASCCP members and experts Hope K. Haefner, MD, Herschel W. Lawson, MD, and Colleen K. Stockdale, MD, MS. This document reflects emerging clinical and scientific advances as of the date issued and is subject to change. The information should not be construed as dictating an exclusive course of treatment or procedure to be followed. Persistent Vulvar Pain ABSTRACT: Persistent vulvar pain is a complex disorder that frequently is frustrating to the patient and the clinician. It can be difficult to treat and rapid resolution is unusual, even with appropriate therapy. Vulvar pain can be caused by a specific disorder or it can be idiopathic. Idiopathic vulvar pain is classified as vulvodynia. Although optimal treatment remains unclear, consider an individualized, multidisciplinary approach to address all physical and emotional aspects possibly attributable to vulvodynia. Specialists who may need to be involved include sexual counselors, clinical psychologists, physical therapists, and pain specialists. Patients may perceive this approach to mean the practitioner does not believe their pain is “real”; thus, it is important to begin any treatment approach with a detailed discussion, including an explanation of the diagnosis and determination of realistic treatment goals. Future research should aim at evaluating a multimodal approach in the treatment of vulvodynia, along with more research on the etiologies of vulvodynia. -

Slide Courtesy of Jeff North, MD
3/17/2017 Basic Dermatology Procedures Basic Dermatology Procedures for the Non‐dermatologist • Liquid Nitrogen • Skin Biopsies Lindy P. Fox, MD • Electrocautery Associate Professor Director, Hospital Consultation Service Department of Dermatology University of California, San Francisco [email protected] I have no conflicts of interest to disclose 1 Liquid Nitrogen Cryosurgery 1 3/17/2017 Liquid Nitrogen Cryosurgery Liquid Nitrogen Cryosurgery Principles • Indications • ‐ 196°C (−320.8°F) – Benign, premalignant, in situ malignant lesions • Temperatures of −25°C to −50°C (−13°F to −58°F) within 30 seconds with spray or probe • Objective – Selective tissue necrosis • Benign lesions: −20°C to −30°C (−4°F to −22°F) • Reactions predictable • Malignant lesions: −40°C to −50°C. – Crust, bulla, exudate, edema, sloughing • Post procedure hypopigmentation • Rapid cooling intracellular ice crystals • Slow thawing tissue damage – Melanocytes are more sensitive to freezing than • Duration of THAW (not freeze) time is most keratinocytes important factor in determining success Am Fam Physician. 2004 May 15;69(10):2365‐2372 Liquid Nitrogen Cryosurgery • Fast freeze, slow thaw cycles – Times vary per condition (longer for deeper lesion) – One cycle for benign, premalignant – Two cycles for warts, malignant (not commonly done) • Lateral spread of freeze (indicates depth of freeze) – Benign lesions 1‐2mm beyond margins – Actinic keratoses‐ 2‐3mm beyond margins – Malignant‐ 3‐5+mm beyond margins (not commonly done) From: Bolognia, Jorizzo, and Schaffer. -

SKIN GRAFTS and SKIN SUBSTITUTES James F Thornton MD
SKIN GRAFTS AND SKIN SUBSTITUTES James F Thornton MD HISTORY OF SKIN GRAFTS ANATOMY Ratner1 and Hauben and colleagues2 give excel- The character of the skin varies greatly among lent overviews of the history of skin grafting. The individuals, and within each person it varies with following highlights are excerpted from these two age, sun exposure, and area of the body. For the sources. first decade of life the skin is quite thin, but from Grafting of skin originated among the tilemaker age 10 to 35 it thickens progressively. At some caste in India approximately 3000 years ago.1 A point during the fourth decade the thickening stops common practice then was to punish a thief or and the skin once again begins to decrease in sub- adulterer by amputating the nose, and surgeons of stance. From that time until the person dies there is their day took free grafts from the gluteal area to gradual thinning of dermis, decreased skin elastic- repair the deformity. From this modest beginning, ity, and progressive loss of sebaceous gland con- skin grafting evolved into one of the basic clinical tent. tools in plastic surgery. The skin also varies greatly with body area. Skin In 1804 an Italian surgeon named Boronio suc- from the eyelid, postauricular and supraclavicular cessfully autografted a full-thickness skin graft on a areas, medial thigh, and upper extremity is thin, sheep. Sir Astley Cooper grafted a full-thickness whereas skin from the back, buttocks, palms of the piece of skin from a man’s amputated thumb onto hands and soles of the feet is much thicker. -
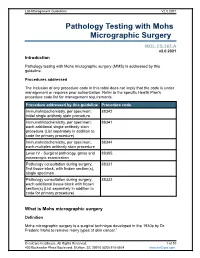
Pathology Testing with Mohs Micrographic Surgery
Lab Management Guidelines V2.0.2021 Pathology Testing with Mohs Micrographic Surgery MOL.CS.363.A v2.0.2021 Introduction Pathology testing with Mohs micrographic surgery (MMS) is addressed by this guideline. Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedure addressed by this guideline Procedure code Immunohistochemistry, per specimen; 88342 initial single antibody stain procedure Immunohistochemistry, per specimen; 88341 each additional single antibody stain procedure (List separately in addition to code for primary procedure) Immunohistochemistry, per specimen; 88344 each multiplex antibody stain procedure Level IV - Surgical pathology, gross and 88305 microscopic examination Pathology consultation during surgery; 88331 first tissue block, with frozen section(s), single specimen Pathology consultation during surgery; 88332 each additional tissue block with frozen section(s) (List separately in addition to code for primary procedure) What is Mohs micrographic surgery Definition Mohs micrographic surgery is a surgical technique developed in the 1930s by Dr. Frederic Mohs to remove many types of skin cancer.1 © eviCore healthcare. All Rights Reserved. 1 of 10 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines V2.0.2021 It is performed by dermatologists, many of whom have completed a one or two year fellowship in Mohs surgery.2 One of the defining, and unique, features of this technique is that the Mohs surgeon also serves the role of the pathologist, examining frozen sections of excised tissue at the time of surgery. -

Erosive Lichen Planus Affecting the Vulva
EROSIVE LICHEN PLANUS AFFECTING THE VULVA: Defining the disease, developing outcome measures and designing a randomised controlled trial Rosalind C Simpson BMedSci, BMBS, MRCP(UK) Thesis submitted to the University of Nottingham for the degree of Doctor of Philosophy December 2014 Abstract Erosive lichen planus (ELP) is a chronic, inflammatory, scarring skin condition that occurs predominantly on the mucosal surfaces of the mouth and genital region. It is believed to be an autoimmune condition although the exact pathogenesis remains unclear. This thesis focuses on ELP affecting the vulvovaginal region (ELPV). This is a rare condition with unknown incidence and prevalence. It causes painful raw areas at the vaginal entrance and subsequent scarring leads to anatomical changes with narrowing of the vaginal canal. Symptoms lead to difficulty in normal daily activities such as walking/sitting, washing, going to the toilet and can prevent normal sexual function. There is risk of cancerous change in affected skin of 1-3%. A Cochrane Systematic Review of interventions for mucosal erosive lichen planus, published in 2012, found no randomised controlled trials (RCT) on which to base treatment for ELPV. Evidence for treatments has historically been based upon retrospective case- series and case reports. Retrospective case series suggest that super-potent topical corticosteroids an effective first-line therapy, although one third of patients fail to respond adequately and require I Abstract escalation of therapy. There is no agreement for which second-line agents should be used and this is where the greatest clinical need for therapeutic guidance exists. The objective of this PhD was to begin to standardise practice for the management of people with ELPV and then develop a pragmatic protocol for those individuals who had failed to adequately respond to first line therapy with super-potent topical corticosteroids. -

Provider Type 72 Nurse Anesthetist Reimbursement Rates
Provider Type 72 Nurse Anesthetist Reimbursement Rates Updated: May 1, 2015 The information contained in the schedule is made available to provide information and is not a guarantee by the State or the Department or its employees as to the present accuracy of the information contained herein. For example, coverage as well as an actual rate may have been revised or updated and may no longer be the same as posted on the website. Note: Procedure codes with a rate of $0.00 are reimbursed at 62% of Usual and Customary charges unless noted otherwise in Nevada Medicaid policy. CPT codes, descriptions and other data only are copyright © 2008 American Medical Association. All rights reserved. Applicable FARS/DFARS apply. CPT is a registered trademark ® of the American Medical Association. Modifier List Anesthesiology Unit Values Proc Code Description Mod Rate 01953 ANESTH BURN EACH 9 PERCENT 21.12 01996 HOSP MANAGE CONT DRUG ADMIN 63.36 10021 FNA W/O IMAGE TC 12.96 10021 FNA W/O IMAGE 26 48.11 10021 FNA W/O IMAGE 61.32 10022 FNA W/IMAGE TC 17.20 10022 FNA W/IMAGE 26 45.87 10022 FNA W/IMAGE 63.07 10040 ACNE SURGERY 45.12 10060 DRAINAGE OF SKIN ABSCESS 49.86 10061 DRAINAGE OF SKIN ABSCESS 103.70 10080 DRAINAGE OF PILONIDAL CYST 51.35 10081 DRAINAGE OF PILONIDAL CYST 108.69 10120 REMOVE FOREIGN BODY 42.87 10121 REMOVE FOREIGN BODY 122.40 10140 DRAINAGE OF HEMATOMA/FLUID 66.06 10160 PUNCTURE DRAINAGE OF LESION 44.62 10180 COMPLEX DRAINAGE WOUND 98.47 11000 DEBRIDE INFECTED SKIN 22.68 11001 DEBRIDE INFECTED SKIN ADD-ON 10.96 11010 DEBRIDE SKIN AT FX -

Shave and Punch Biopsy for Skin Lesions
Shave and Punch Biopsy for Skin Lesions HEATHER PICKETT, DO, Nellis Air Force Base Family Medicine Residency, Mike O’Callaghan Federal Hospital, Nellis Air Force Base, Nevada Shave and punch biopsies are essential procedures for physicians who manage skin conditions. These office-based procedures can diagnose questionable dermatologic lesions, including possible malignancies. Approaches include the superficial shave biopsy, sau- cerization excision, punch biopsy, and elliptical excision. A super- ficial shave biopsy can be used for raised lesions. A saucerization biopsy may be performed for flat or pigmented lesions. Punch biop- sies yield full-thickness samples and can be used for lesions that require dermal or subcutaneous tissue for diagnosis. Indications for biopsy of suspected melanoma remain controversial. Sufficient tissue may be obtained with the quicker, less costly saucerization biopsy or the more time-consuming, invasive elliptical excisional biopsy. (Am Fam Physician. 2011;84(9):995-1002. Copyright © 2011 American Academy of Family Physicians.) kin biopsies are simple office pro- lesion for diagnostic purposes (e.g., fusiform cedures that can provide useful ellipse, punch for 1- to 4-mm lesions, saucer- information about undiagnosed ization [also called deep scoop shave]).1 lesions such as neoplasms, bullous This article reviews conditions that warrant S disorders, keratoses, or dysplastic nevi. A office-based biopsy; the types of biopsies com- diagnostic biopsy can also be the definitive monly performed in the office setting; and treatment for some malignant, irritated, or indications (Table 12-4), contraindications, and precancerous lesions. The primary types of proper techniques. Superficial shave, sauceriza- skin biopsies are incisional and excisional. tion, and punch biopsies are emphasized. -

2020 National Physician Fee Schedule Relative Value File January Release CPT Codes and Descriptions Only Are Copyright 2018 American Medical Association
2020 National Physician Fee Schedule Relative Value File January Release CPT codes and descriptions only are copyright 2018 American Medical Association. All Rights Reserved. Applicable FARS/DFARS Apply. Dental codes (D codes) are copyright 2019/20 American Dental Association. All Rights Reserved. RELEASED 11/08/2019 NON-FACILITY HCPCS MOD DESCRIPTION TOTAL MULTIPLIER TOTAL 1000F Tobacco use assessed 0.00 $70.00 $0.00 10004 Fna bx w/o img gdn ea addl 1.48 $70.00 $103.60 10005 Fna bx w/us gdn 1st les 3.67 $70.00 $256.90 10006 Fna bx w/us gdn ea addl 1.70 $70.00 $119.00 10007 Fna bx w/fluor gdn 1st les 8.43 $70.00 $590.10 10008 Fna bx w/fluor gdn ea addl 4.79 $70.00 $335.30 10009 Fna bx w/ct gdn 1st les 13.32 $70.00 $932.40 10010 Fna bx w/ct gdn ea addl 8.02 $70.00 $561.40 10011 Fna bx w/mr gdn 1st les 0.00 $70.00 $0.00 10012 Fna bx w/mr gdn ea addl 0.00 $70.00 $0.00 1002F Assess anginal symptom/level 0.00 $70.00 $0.00 10021 Fna bx w/o img gdn 1st les 2.80 $70.00 $196.00 1003F Level of activity assess 0.00 $70.00 $0.00 10030 Guide cathet fluid drainage 17.53 $70.00 $1,227.10 10035 Perq dev soft tiss 1st imag 12.84 $70.00 $898.80 10036 Perq dev soft tiss add imag 10.92 $70.00 $764.40 1004F Clin symp vol ovrld assess 0.00 $70.00 $0.00 10040 Acne surgery 3.11 $70.00 $217.70 1005F Asthma symptoms evaluate 0.00 $70.00 $0.00 1006F Osteoarthritis assess 0.00 $70.00 $0.00 10060 Drainage of skin abscess 3.44 $70.00 $240.80 10061 Drainage of skin abscess 5.97 $70.00 $417.90 1007F Anti-inflm/anlgsc otc assess 0.00 $70.00 $0.00 1008F Gi/renal risk assess -

34. Surgery of the Skin & Soft Tissues
785 THE DIFFERENTIAL DIAGNOSIS may be difficult 34 Surgery of the skin early on. & soft tissues Suggesting a hypertrophic scar (34-1C): abnormal uniform growth starting within weeks of injury, growth restricted to the confines of the original scar, darker than surrounding skin, spontaneous regression in 34.1 Hypertrophic scars & keloids 6months to 3yrs to become broad, soft, thin, and level with the surrounding skin, anywhere in the body, very common in burns scars, itching commonly which may be severe. A surgical scar, especially if it is on the face, should be nearly invisible if made along Langer’s lines (34.1). Suggesting a keloid (34-1D): onset delayed for Sometimes a scar becomes very visible indeed as the result months/yrs, invasion of the surrounding skin, growth stops of hypertrophy and keloid formation. Both these processes in due course but there is no regression, localized can follow surgery, tattooing, infection or almost any commonly on the earlobes, chin, neck, presternal area, and breach of the skin surface. Both cause large scars, and are the midline, not uncommon in young black patients, identical histologically, but they behave differently. uncommon in burn scars, very uncommon below the groin Keloids are difficult to treat. If you excise one through and where vascularization is poor. normal skin and graft the gap, it is likely to recur round the edges of the graft, or in any gaps or splits within the graft. If diagnosis is difficult, remember that a keloid becomes Both a hypertrophic and a keloid response are more likely increasingly raised, and extends beyond the confines of the if a wound is infected, contaminated by foreign material original scar.