Cardiac Disease in Pregnancy D
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Early Diastolic Clicks After the Fontan Procedure for Double
304 Br Heart J 1990;63:304-7 Early diastolic clicks after the Fontan procedure for double inlet left ventricle: anatomical and physiological correlates Br Heart J: first published as 10.1136/hrt.63.5.304 on 1 May 1990. Downloaded from Andrew N Redlngton, Kit-Yee Chan, Julene S Carvalho, Elliot A Shinebourne Abstract inlet ventricle with two atrioventricular M mode echocardiograms and simultan- valves. All had previously undergone a Fontan eous phonocardiograms were recorded type procedure with direct atriopulmonary in four patients with early diastolic anastomosis. In two patients a valved clicks on auscultation. All had double homograft was interposed between the right inlet left ventricle and had undergone atrium and pulmonary artery. Each patient the Fontan procedure with closure of the had the right atrioventricular valve closed by right atrioventricular valve orifice by an either a single or double layer of Dacron cloth artifical patch. The phonocardiogram sewn into the floor of the right atrium. The confirmed a high frequency sound main pulmonary artery was tied off in all. occurring 60-90 ms after aortic valve Cross sectional, M mode, and pulsed wave closure and coinciding with the time of Doppler echocardiograms with simultaneous maximal excursion of the atrioven- electrocardiogram and phonocardiogram were tricular valve patch towards the ven- recorded on a Hewlett-Packard 77020A tricular mass. One patient had coexist- ultrasound system. The phonocardiogram was ing congenital complete heart block. recorded over the point on the chest where the The M mode echocardiogram showed diastolic click was best heart on auscultation, i'reversed") motion of the patch towards usually in the fourth left intercostal space the right atrium during atrial contrac- close to the sternum. -
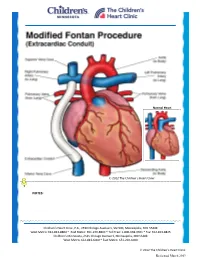
Modified Fontan Procedure: Extracardiac Conduit
Normal Heart © 2012 The Children’s Heart Clinic NOTES: Children’s Heart Clinic, P.A., 2530 Chicago Avenue S, Ste 500, Minneapolis, MN 55404 West Metro: 612-813-8800 * East Metro: 651-220-8800 * Toll Free: 1-800-938-0301 * Fax: 612-813-8825 Children’s Minnesota, 2525 Chicago Avenue S, Minneapolis, MN 55404 West Metro: 612-813-6000 * East Metro: 651-220-6000 © 2012 The Children’s Heart Clinic Reviewed March 2019 Modified Fontan Procedure: Extracardiac Conduit The Fontan procedure is usually the third procedure done in a series of surgeries to complete palliation of single ventricle patients. This procedure separates the “blue,” deoxygenated blood from the “red,” oxygenated blood circuit. Once the Fontan is done, deoxygenated blood drains passively to the pulmonary arteries, then to the lungs. Blood receives oxygen from the lungs and returns to the heart, where it is actively pumped out to the body. This procedure is usually done between 2-4 years of age. During surgery, the chest is opened through the previous incision, using a median sternotomy. The operation may or may not involve the use of cardiopulmonary bypass (heart-lung machine), depending on the surgical plan. A Gore-tex® tube graft (Gore) is cut to the appropriate length. An incision is made on the pulmonary artery near the area of the existing bidirectional Glenn shunt (cavopulmonary anastomosis) and the tube graft is sutured to the artery. Once that is complete, the inferior vena cava is divided from the atrium. The lower end of the Gore-tex® tube graft (Gore) is then sutured to the inferior vena cava. -

E001466.Full.Pdf
Editorial BMJ Glob Health: first published as 10.1136/bmjgh-2019-001466 on 11 April 2019. Downloaded from WHO recommendations on uterotonics for postpartum haemorrhage prevention: what works, and which one? Joshua P Vogel, 1,2 Myfanwy Williams,3 Ioannis Gallos,4 Fernando Althabe,1 Olufemi T Oladapo1 To cite: Vogel JP, THE GLOBAL BURDEN OF POSTPARTUM trials of tranexamic acid for PPH treatment Williams M, Gallos I, et al. HAEMORRHAGE and a heat-stable formulation of carbetocin WHO recommendations on 6–12 uterotonics for postpartum Obstetric haemorrhage, especially post- for PPH prevention. The increasing haemorrhage prevention: partum haemorrhage (PPH), was responsible number of PPH prevention and management what works, and which for more than a quarter of the estimated 303 options makes it challenging for providers one?BMJ Glob Health 000 maternal deaths that occurred globally in and health system stakeholders to choose 2019;4:e001466. doi:10.1136/ 2015.1 PPH—commonly defined as a blood where and how to invest limited resources in bmjgh-2019-001466 loss of 500 mL or more within 24 hours after order to optimise health outcomes. birth—affects about 6% of all women giving Multiple uterotonics have been eval- Handling editor Seye Abimbola birth.1 Uterine atony is the most common uated for PPH prevention over the past Received 4 February 2019 cause of PPH, but it can also be caused by four decades, including oxytocin receptor Revised 10 March 2019 genital tract trauma, retained placental tissue agonists (oxytocin and carbetocin), prosta- Accepted 16 March 2019 or maternal bleeding disorders. The majority glandin analogues (misoprostol, sulprostone, of women who experience PPH have no iden- carboprost), ergot alkaloids (such as ergo- tifiable risk factor, meaning that PPH preven- metrine/methylergometrine) and combina- tion programmes rely on universal use of PPH tions of these (oxytocin plus ergometrine, © Author(s) (or their prophylaxis for all women in the immediate or oxytocin plus misoprostol). -

New Zealand Data Sheet
NEW ZEALAND DATA SHEET 1. PRODUCT NAME PROSTIN 15M 250 microgram (µg)/mL Solution for Injection 2. QUALITATIVE AND QUANTITIATIVE COMPOSITION Each 1 mL contains 250 μg carboprost or 332 μg carboprost (as tromethamine). Excipient(s) with known effect Each 1 mL contains 9.45 mg/mL benzyl alcohol (added as preservative). For the full list of excipients, see section 6.1. 3. PHARMACEUTIAL FORM Solution for Injection. PROSTIN 15M is a clear colourless solution. 4. CLINCAL PARTICUALRS 4.1 Therapeutic indications PROSTIN 15M is indicated for the treatment of postpartum haemorrhage due to uterine atony which has not responded to conventional methods of management. Prior treatment should include the use of intravenously administered oxytocin, manipulative techniques such as uterine massage and, unless contraindicated, intramuscular ergot preparations. Studies have shown that in such cases, the use of PROSTIN 15M has resulted in satisfactory control of haemorrhage, although it is unclear whether or not ongoing or delayed effects of previously administered embolic agents have contributed to the outcome. In a high proportion of cases, PROSTIN 15M used in this manner has resulted in the cessation of life threatening bleeding and the avoidance of emergency surgical intervention. 4.2 Dose and method of administration Dose An initial dose of 250 µg (1 mL) is to be given by deep intramuscular injection. In clinical trials, it was found that the majority of successful cases (73%) responded to single injections. In some selected cases, however, multiple dosing at intervals of 15 to 90 minutes was carried out with successful outcome. The need for additional injections and the interval at which these should be given can be determined only by the attending physicians as dictated by the course of clinical events. -

The Physiology of the Fontan Circulation ⁎ Andrew Redington
Progress in Pediatric Cardiology 22 (2006) 179–186 www.elsevier.com/locate/ppedcard The physiology of the Fontan circulation ⁎ Andrew Redington Division of Cardiology, The Department of Pediatrics, The Hospital for Sick Children, University of Toronto School of Medicine, Toronto, Ontario, Canada Available online 8 September 2006 Abstract The Fontan circulation, no matter which of its various iterations, is abnormal in virtually every aspect of its performance. Some of these abnormalities are primarily the result of the procedure itself, and others are secondary to the fundamental disturbances of circulatory performance imposed by the ‘single’ ventricle circulation. The physiology of ventricular, systemic arterial and venopulmonary function will be described in this review. © 2006 Elsevier Ireland Ltd. All rights reserved. Keywords: palliation; Fontan circulation; Cavopulmonary anastomosis; Antriopulmonary anastomosis 1. Introduction has the profound consequences for the systemic ventricle that will discussed below. At the same time as the bidirectional In this personal overview, I will discuss the physiology of the cavopulmonary anastomosis was becoming almost uniformly Fontan circulation. Bob Freedom's contribution to our under- adopted, there was abandonment of the ‘classical’ atriopulmon- standing of complex congenital heart disease has meant that ary anastomosis, in favour of the total cavopulmonary con- many more of these patients are surviving with this physiology nection (TCPC). The ‘lateral wall’ TCPC, popularised by Marc than could have been contemplated 30 years ago. Nonetheless, deLeval [1], was shown experimentally and clinically to be they represent a very difficult group of patients and we continue haemodynamically more efficient [1,2] and set the scene for the to learn more about this unique circulation. -

Eicosanoids & Platelet Activating Factor
Eicosanoids & Platelet Activating Factor Prof. Sanjay Khattri Dept. of Pharmacology & Therapeutics King George’s Medical University, Lucknow 1 Autacoid These are the substances produced by wide variety of cells that act locally at the site of production. (local hormones) 2 Mediators of Inflammation and Immune reaction 1. Vasoactive amines (Histamine and Serotonin) 2.Eicosanoids 3.Platlet Activating Factor 4.Bradykinins 4.Nitric Oxide 5.Neuropeptides 6.Cytokinines 3 EICOSANOIDS PGs, TXs and LTs are all derived from eicosa (referring to 20 C atoms) tri/tetra/ penta enoic acids. Therefore, they can be collectively called eicosanoids. Major source: 5,8,11,14 eicosa tetraenoic acid (arachidonic acid). Other eicosanoids of increasing interest are: lipoxins and resolvins. The term prostanoid encompasses both prostaglandins and thromboxanes. 4 EICOSANOIDS Contd…. In most instances, the initial and rate-limiting step in eicosanoid synthesis is the liberation of intracellular arachidonate, usually in a one-step process catalyzed by the enzyme phospholipase A2 (PLA2). PLA2 generates not only arachidonic acid but also lysoglyceryl - phosphorylcholine (lyso-PAF), the precursor of platelet activating factor (PAF). 5 EICOSANOIDS Contd…. Corticosteroids inhibit the enzyme PLA2 by inducing the production of lipocortins (annexins). The free arachidonic acid is metabolised separately (or sometimes jointly) by several pathways, including the following: Cyclo-oxygenase (COX)- Two main isoforms exist, COX-1 and COX-2 Lipoxygenases- Several subtypes, which -

Product Monograph
PRODUCT MONOGRAPH HEMABATE® STERILE SOLUTION (carboprost tromethamine injection USP) 250 µg/mL Prostaglandin Pfizer Canada Inc. Date of Revision: 17,300 Trans-Canada Highway February 21, 2014 Kirkland, Quebec H9J 2M5 Control No. 170114 ® Pfizer Enterprises SARL Pfizer Canada Inc, Licensee © Pfizer Canada Inc. 2014 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION ..........................................................3 SUMMARY OF PRODUCT INFORMATION ..................................................................3 INDICATIONS AND CLINICAL USE ..............................................................................3 CONTRAINDICATIONS ...................................................................................................4 WARNINGS AND PRECAUTIONS ..................................................................................4 ADVERSE REACTIONS ....................................................................................................7 DRUG INTERACTIONS ..................................................................................................10 DOSAGE AND ADMINISTRATION ..............................................................................11 OVERDOSAGE ................................................................................................................11 ACTION AND CLINICAL PHARMACOLOGY ............................................................12 STORAGE AND STABILITY ..........................................................................................12 DOSAGE -

Preparation and Chiral HPLC Separation of the Enantiomeric Forms of Natural Prostaglandins
Article Preparation and Chiral HPLC Separation of the Enantiomeric Forms of Natural Prostaglandins Márton Enesei 1,2,László Takács 2, Enik˝oTormási 3, Adrienn Tóthné Rácz 3, Zita Róka 3, Mihály Kádár 3 and Zsuzsanna Kardos 2,* 1 Department of Organic Chemistry and Technology, Budapest University of Technology and Economics, M˝uegyetemrakpart 3, 1111 Budapest, Hungary; [email protected] 2 CHINOIN, a member of Sanofi Group, PG Development, Tó utca 1-5, 1045 Budapest, Hungary; laszlo.takacs@sanofi.com 3 CHINOIN, a member of Sanofi Group, PG Analytics, Tó utca 1-5, 1045 Budapest, Hungary; robertne.tormasi@sanofi.com (E.T.); adrienn.tothneracz@sanofi.com (A.T.R.); zita.roka@sanofi.com (Z.R.); mihaly.kadar@sanofi.com (M.K.) * Correspondence: zsuzsanna.kardos@sanofi.com Received: 15 June 2020; Accepted: 10 August 2020; Published: 18 August 2020 Abstract: Four enantiomeric forms of natural prostaglandins, ent-PGF α (( )-1), ent-PGE ((+)-2) 2 − 2 ent-PGF α (( )-3), and ent-PGE ((+)-4) have been synthetized in gram scale by Corey synthesis used 1 − 1 in the prostaglandin plants of CHINOIN, Budapest. Chiral HPLC methods have been developed to separate the enantiomeric pairs. Enantiomers of natural prostaglandins can be used as analytical standards to verify the enantiopurity of synthetic prostaglandins, or as biomarkers to study oxidation processes in vivo. Keywords: preparation; ent-PGF2α; ent-PGF1α; ent-PGE2; ent-PGE1; chiral HPLC; enantiomeric separation; mirror images; enantiopurity 1. Introduction Interest in the field of prostaglandins has been steadily growing since the basic work of Bergström Samuelsson, and Vane [1–3]. Their discoveries revealed the structure, the enzyme-controlled biochemical synthesis from arachidonic acid, and the main physiological effects of prostaglandins as well as their related substances. -

Arterial Switch Operation Surgery Surgical Solutions to Complex Problems
Pediatric Cardiovascular Arterial Switch Operation Surgery Surgical Solutions to Complex Problems Tom R. Karl, MS, MD The arterial switch operation is appropriate treatment for most forms of transposition of Andrew Cochrane, FRACS the great arteries. In this review we analyze indications, techniques, and outcome for Christian P.R. Brizard, MD various subsets of patients with transposition of the great arteries, including those with an intact septum beyond 21 days of age, intramural coronary arteries, aortic arch ob- struction, the Taussig-Bing anomaly, discordant (corrected) transposition, transposition of the great arteries with left ventricular outflow tract obstruction, and univentricular hearts with transposition of the great arteries and subaortic stenosis. (Tex Heart Inst J 1997;24:322-33) T ransposition of the great arteries (TGA) is a prototypical lesion for pediat- ric cardiac surgeons, a lethal malformation that can often be converted (with a single operation) to a nearly normal heart. The arterial switch operation (ASO) has evolved to become the treatment of choice for most forms of TGA, and success with this operation has become a standard by which pediatric cardiac surgical units are judged. This is appropriate, because without expertise in neonatal anesthetic management, perfusion, intensive care, cardiology, and surgery, consistently good results are impossible to achieve. Surgical Anatomy of TGA In the broad sense, the term "TGA" describes any heart with a discordant ven- triculoatrial (VA) connection (aorta from right ventricle, pulmonary artery from left ventricle). The anatomic diagnosis is further defined by the intracardiac fea- tures. Most frequently, TGA is used to describe the solitus/concordant/discordant heart. -

Norwood/Batista Operation for a Newborn with Dilated Myopathy of the Left Ventricle
612 Brief communications The Journal of Thoracic and Cardiovascular Surgery September 2000 NORWOOD/BATISTA OPERATION FOR A NEWBORN WITH DILATED MYOPATHY OF THE LEFT VENTRICLE Richard D. Mainwaring, MD, Regina M. Healy, BS, John D. Murphy, MD, and William I. Norwood, MD, PhD, Wilmington, Del Partial left ventriculectomy for dilated cardiomyopathy was contractile function. The variable results that have been first reported by Batista and associates1 in 1996. The rationale reported in the adult literature may reflect patient selection for this procedure is the increase in left ventricular cavity size according to the reversibility or recoverability of the underly- in the absence of compensatory left ventricular wall thickness ing disease process. that is observed in dilated cardiomyopathy. This combination Despite the substantial worldwide experience with the of factors results in an increase in wall stress per unit muscle Batista procedure in adult patients, there is limited experience mass, as predicted by the LaPlace equation. As wall stress with this procedure in children. The current case report increases, mechanical load eventually becomes nonsustain- describes the treatment of a patient in whom the diagnosis of able and contributes to further dilation of the ventricle. Partial dilated cardiomyopathy was made in utero. left ventriculectomy has been advocated as a method of Clinical summary. A female infant was recognized in restoring the balance between cavity size and wall thickness. utero as having a dilated, poorly functioning left ventricle. Fundamental to this concept is the assumption that the left Labor was induced at 36 weeks’ gestation, and she was deliv- ventricular muscle is intrinsically normal or has recoverable ered by normal, spontaneous, vaginal delivery. -

The Clinical Spectrum of Fontan-Associated Liver Disease: Results from a Prospective Multimodality Screening Cohort
Edinburgh Research Explorer The clinical spectrum of Fontan-associated liver disease: results from a prospective multimodality screening cohort Citation for published version: Munsterman, ID, Duijnhouwer, AL, Kendall, TJ, Bronkhorst, CM, Ronot, M, van Wettere, M, van Dijk, APJ, Drenth, JPH & Tjwa, ETTL 2019, 'The clinical spectrum of Fontan-associated liver disease: results from a prospective multimodality screening cohort', European Heart Journal, vol. 40, no. 13, pp. 1057–1068. https://doi.org/10.1093/eurheartj/ehy620 Digital Object Identifier (DOI): 10.1093/eurheartj/ehy620 Link: Link to publication record in Edinburgh Research Explorer Document Version: Peer reviewed version Published In: European Heart Journal General rights Copyright for the publications made accessible via the Edinburgh Research Explorer is retained by the author(s) and / or other copyright owners and it is a condition of accessing these publications that users recognise and abide by the legal requirements associated with these rights. Take down policy The University of Edinburgh has made every reasonable effort to ensure that Edinburgh Research Explorer content complies with UK legislation. If you believe that the public display of this file breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. Download date: 25. Sep. 2021 Title: The clinical spectrum of Fontan-Associated Liver Disease: results from a prospective multimodality screening cohort. Authors: I.D. Munsterman1, A.L. Duijnhouwer2, T.J. Kendall3, C.M. Bronkhorst4, M. Ronot5, M. van Wettere5, A.P.J. van Dijk2, J.P.H. Drenth1, E.T.T.L. Tjwa1 On behalf of the Nijmegen Fontan Initiative (A.P.J. -

ICD-10 Coordination and Maintenance Committee Agenda
DEPARTMENT OF HEALTH & HUMAN SERVICES Centers for Medicare & Medicaid Services 7500 Security Boulevard Baltimore, Maryland 21244-1850 Agenda ICD-10 Coordination and Maintenance Committee Department of Health and Human Services Centers for Medicare & Medicaid Services CMS Auditorium 7500 Security Boulevard Baltimore, MD 21244-1850 ICD-10-PCS Topics March 7, 2017 Pat Brooks, CMS – Co -Chairperson Webcast and Dial-In Information The meeting will begin promptly at 9am ET and will be webcast. Toll-free dial-in access is available for participants who cannot join the webcast: Phone: 1-844-396-8222; Meeting ID: 909 233 082. We encourage you to join early, as the number of phone lines is limited. If participating via the webcast or dialing in you do NOT need to register on-line for the meeting. This meeting is being webcast via CMS at http://www.cms.gov/live/. By your attendance, you are giving consent to the use and distribution of your name, likeness and voice during the meeting. You are also giving consent to the use and distribution of any personally identifiable information that you or others may disclose about you during the meeting. Please do not disclose personal health information. Note: Proposals for diagnosis code topics are scheduled for March 8, 2017 and will be led by the Centers for Disease Control (CDC). Please visit CDCs website for the Diagnosis agenda located at the following address: http://www.cdc.gov/nchs/icd/icd9cm_maintenance.htm 1 Introductions and Overview Pat Brooks ICD-10-PCS Topics: 1. Cerebral Embolic Protection During Michelle Joshua Transcatheter Aortic Valve Replacement Alexandra Lansky, MD Pages 10-11 Professor of Medicine, Section of Cardiology Yale School of Medicine 2.