Inhaled Nitric Oxide
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Biochemical Rationale for the Discrete Behavior of Nitroxyl and Nitric Oxide in the Cardiovascular System
A biochemical rationale for the discrete behavior of nitroxyl and nitric oxide in the cardiovascular system Katrina M. Miranda*†‡, Nazareno Paolocci§, Tatsuo Katori§, Douglas D. Thomas*, Eleonora Ford¶, Michael D. Bartbergerʈ, Michael G. Espey*, David A. Kass§, Martin Feelisch**, Jon M. Fukuto¶, and David A. Wink*† *Radiation Biology Branch, Building 10, Room B3-B69, National Cancer Institute, National Institutes of Health, Bethesda, MD 20892; §Division of Cardiology, Department of Medicine, The Johns Hopkins Medical Institutions, Baltimore, MD 21287; ¶Department of Molecular and Medical Pharmacology, Center for the Health Sciences, University of California, Los Angeles, CA 90095; ʈDepartment of Chemistry and Biochemistry, University of California, Los Angeles, CA 90095; and **Department of Molecular and Cellular Physiology, Louisiana State University Health Sciences Center, Shreveport, LA 71130 Edited by Louis J. Ignarro, University of California School of Medicine, Los Angeles, CA, and approved May 20, 2003 (received for review February 20, 2003) The redox siblings nitroxyl (HNO) and nitric oxide (NO) have often cellular thiol functions (14, 15). Conversely, NO reacts only indi- been assumed to undergo casual redox reactions in biological sys- rectly with thiols after RNOS formation (17). tems. However, several recent studies have demonstrated distinct Contrasting effects are also apparent in vivo or ex vivo,for pharmacological effects for donors of these two species. Here, infu- example in models of ischemia reperfusion injury. Exposure to NO sion of the HNO donor Angeli’s salt into normal dogs resulted in donors at the onset of reperfusion provides protection against elevated plasma levels of calcitonin gene-related peptide, whereas reperfusion injury in the heart and other organs (18–20). -
Download Product Insert (PDF)
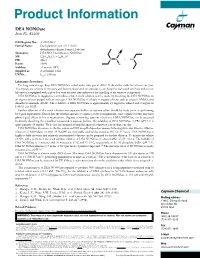
Product Information DEA NONOate Item No. 82100 CAS Registry No.: 372965-00-9 Formal Name: Diethylammonium (Z)-1-(N,N- diethylamino)diazen-1-ium-1,2-diolate O Synonyms: DEA/NO, Diethylamine NONOate N MF: C4H10N3O2 • C4H12N + N N • H N FW: 206.3 2 Purity: ≥98% O- Stability: ≥1 year at -80°C Supplied as: A crystalline solid l UV/Vis.: max: 250 nm Laboratory Procedures For long term storage, keep DEA NONOate sealed under nitrogen at -80°C. It should be stable for at least one year. The crystals are sensitive to moisture and become discolored on exposure to air. Keep the vial sealed until use unless your laboratory is equipped with a glove box with an inert atmosphere for the handling of air sensitive compounds. DEA NONOate is supplied as a crystalline solid. A stock solution may be made by dissolving the DEA NONOate in an organic solvent purged with an inert gas. DEA NONOate is soluble in organic solvents such as ethanol, DMSO, and dimethyl formamide (DMF). The solubility of DEA NONOate is approximately 25 mg/ml in ethanol and 2 mg/ml in DMSO and DMF. Further dilutions of the stock solution into aqueous buffers or isotonic saline should be made prior to performing biological experiments. Ensure that the residual amount of organic solvent is insignificant, since organic solvents may have physiological effects at low concentrations. Organic solvent-free aqueous solutions of DEA NONOate can be prepared by directly dissolving the crystalline compound in aqueous buffers. The solubility of DEA NONOate in PBS (pH 7.2) is approximately 10 mg/ml. -

Current Advances of Nitric Oxide in Cancer and Anticancer Therapeutics
Review Current Advances of Nitric Oxide in Cancer and Anticancer Therapeutics Joel Mintz 1,†, Anastasia Vedenko 2,†, Omar Rosete 3 , Khushi Shah 4, Gabriella Goldstein 5 , Joshua M. Hare 2,6,7 , Ranjith Ramasamy 3,6,* and Himanshu Arora 2,3,6,* 1 Dr. Kiran C. Patel College of Allopathic Medicine, Nova Southeastern University, Davie, FL 33328, USA; [email protected] 2 John P Hussman Institute for Human Genomics, Miller School of Medicine, University of Miami, Miami, FL 33136, USA; [email protected] (A.V.); [email protected] (J.M.H.) 3 Department of Urology, Miller School of Medicine, University of Miami, Miami, FL 33136, USA; [email protected] 4 College of Arts and Sciences, University of Miami, Miami, FL 33146, USA; [email protected] 5 College of Health Professions and Sciences, University of Central Florida, Orlando, FL 32816, USA; [email protected] 6 The Interdisciplinary Stem Cell Institute, Miller School of Medicine, University of Miami, Miami, FL 33136, USA 7 Department of Medicine, Cardiology Division, Miller School of Medicine, University of Miami, Miami, FL 33136, USA * Correspondence: [email protected] (R.R.); [email protected] (H.A.) † These authors contributed equally to this work. Abstract: Nitric oxide (NO) is a short-lived, ubiquitous signaling molecule that affects numerous critical functions in the body. There are markedly conflicting findings in the literature regarding the bimodal effects of NO in carcinogenesis and tumor progression, which has important consequences for treatment. Several preclinical and clinical studies have suggested that both pro- and antitumori- Citation: Mintz, J.; Vedenko, A.; genic effects of NO depend on multiple aspects, including, but not limited to, tissue of generation, the Rosete, O.; Shah, K.; Goldstein, G.; level of production, the oxidative/reductive (redox) environment in which this radical is generated, Hare, J.M; Ramasamy, R.; Arora, H. -

Nitric Oxide Attenuates Hypoxia-Induced 5-FU Resistance
Sasabe et al. Int J Cancer Clin Res 2015, 2:2 DOI: 10.23937/2378-3419/2/2/1014 International Journal of Cancer and Clinical Research ISSN: 2378-3419 Original Article: Open Access Nitric Oxide Attenuates Hypoxia-Induced 5-FU Resistance of Oral Squamous Cell Carcinoma Cells Eri Sasabe*, Ayumi Tomomura, Mayuko Hamada, Naoya Kitamura, Tomohiro Yamada and Tetsuya Yamamoto Department of Oral and Maxillofacial Surgery, Kochi Medical School, Kochi University Kohasu, Japan *Corresponding author: Eri Sasabe, Department of Oral and Maxillofacial Surgery, Kochi Medical School, Kochi University Kohasu, Oko-cho, Nankoku, Kochi 783-8505, Japan, Tel: +81-88-880-2423, Fax: +81-88-880-2424, E-mail: [email protected] to development and progression of malignancies, and resistance Abstract to cancer therapy. The heterodimeric transcription factor Hypoxia Hypoxic environments in tumors induce expression of hypoxia- inducible factor (HIF) is a master regulator that can adapt tumor cells inducible factor (HIF). HIF contributes to the development of the to hypoxic conditions [1]. Overexpression of HIF has been observed malignant progression through the induction of various target genes. in many different cancers, including head and neck squamous cell We previously reported that treatment with chemotherapeutic drugs and γ-rays enhances expression and nuclear translocation carcinomas, and is associated with increased patient mortality [2-4]. of HIF-1α under normoxic conditions; susceptibility of oral HIF consists of an oxygen-regulated α-subunit and a constitutively squamous cell carcinoma (OSCC) cells to the drugs and γ-rays expressed β-subunit, also known as aryl hydrocarbon receptor is negatively correlated with expression of HIF-1α protein. -

Oxidative Stress and the Guanosine Nucleotide Triphosphate Pool: Implications for a Biomarker and Mechanism of Impaired Cell Function
University of Montana ScholarWorks at University of Montana Graduate Student Theses, Dissertations, & Professional Papers Graduate School 2008 OXIDATIVE STRESS AND THE GUANOSINE NUCLEOTIDE TRIPHOSPHATE POOL: IMPLICATIONS FOR A BIOMARKER AND MECHANISM OF IMPAIRED CELL FUNCTION Celeste Maree Bolin The University of Montana Follow this and additional works at: https://scholarworks.umt.edu/etd Let us know how access to this document benefits ou.y Recommended Citation Bolin, Celeste Maree, "OXIDATIVE STRESS AND THE GUANOSINE NUCLEOTIDE TRIPHOSPHATE POOL: IMPLICATIONS FOR A BIOMARKER AND MECHANISM OF IMPAIRED CELL FUNCTION" (2008). Graduate Student Theses, Dissertations, & Professional Papers. 728. https://scholarworks.umt.edu/etd/728 This Dissertation is brought to you for free and open access by the Graduate School at ScholarWorks at University of Montana. It has been accepted for inclusion in Graduate Student Theses, Dissertations, & Professional Papers by an authorized administrator of ScholarWorks at University of Montana. For more information, please contact [email protected]. OXIDATIVE STRESS AND THE GUANOSINE NUCLEOTIDE TRIPHOSPHATE POOL: IMPLICATIONS FOR A BIOMARKER AND MECHANISM OF IMPAIRED CELL FUNCTION By Celeste Maree Bolin B.A. Chemistry, Whitman College, Walla Walla, WA 2001 Dissertation presented in partial fulfillment of the requirements for the degree of Doctor of Philosophy in Toxicology The University of Montana Missoula, Montana Spring 2008 Approved by: Dr. David A. Strobel, Dean Graduate School Dr. Fernando Cardozo-Pelaez, -

Sustained Formation of Nitroglycerin-Derived Nitric Oxide
Supplemental material to this article can be found at: http://molpharm.aspetjournals.org/content/suppl/2018/01/22/mol.117.110783.DC1 1521-0111/93/4/335–343$35.00 https://doi.org/10.1124/mol.117.110783 MOLECULAR PHARMACOLOGY Mol Pharmacol 93:335–343, April 2018 Copyright ª 2018 The Author(s). This is an open access article distributed under the CC BY Attribution 4.0 International license. Sustained Formation of Nitroglycerin-Derived Nitric Oxide by Aldehyde Dehydrogenase-2 in Vascular Smooth Muscle without Added Reductants: Implications for the Development of Nitrate Tolerance s Marissa Opelt, Gerald Wölkart, Emrah Eroglu, Markus Waldeck-Weiermair, Roland Malli, Wolfgang F. Graier, Alexander Kollau, John T. Fassett, Astrid Schrammel, Bernd Mayer, and Antonius C. F. Gorren Downloaded from Institute of Pharmaceutical Sciences, Department of Pharmacology and Toxicology, Karl-Franzens University (M.O., G.W., A.K., J.T.F., A.S., B.M., A.C.F.G.), and Institute of Molecular Biology and Biochemistry, Center of Molecular Medicine, Medical University Graz (E.E., M.W.-W., R.M., W.F.G.), Graz, Austria Received October 4, 2017; accepted January 18, 2018 molpharm.aspetjournals.org ABSTRACT According to current views, oxidation of aldehyde dehydrogenase-2 ALDH2, thiol-refractive inactivation was observed, particularly under (ALDH2) during glyceryltrinitrate (GTN) biotransformation is essen- high-turnover conditions. Organ bath experiments with rat aortas tially involved in vascular nitrate tolerance and explains the de- showed that relaxation by GTN lasted longer than that caused by the pendence of this reaction on added thiols. Using a novel fluorescent NO donor diethylamine/NONOate, in line with the long-lasting intracellular nitric oxide (NO) probe expressed in vascular smooth nanomolar NO generation from GTN observed in VSMCs. -

New Insights Into the Role of Soluble Guanylate Cyclase in Blood Pressure Regulation
New insights into the role of soluble guanylate cyclase in blood pressure regulation The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters Citation Buys, Emmanuel, and Patrick Sips. 2014. New Insights into the Role of Soluble Guanylate Cyclase in Blood Pressure Regulation. Current Opinion in Nephrology and Hypertension 23, no. 2: 135–142. doi:10.1097/01.mnh.0000441048.91041.3a. Published Version doi:10.1097/01.mnh.0000441048.91041.3a Citable link http://nrs.harvard.edu/urn-3:HUL.InstRepos:29731915 Terms of Use This article was downloaded from Harvard University’s DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http:// nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-of- use#LAA NIH Public Access Author Manuscript Curr Opin Nephrol Hypertens. Author manuscript; available in PMC 2015 March 01. NIH-PA Author ManuscriptPublished NIH-PA Author Manuscript in final edited NIH-PA Author Manuscript form as: Curr Opin Nephrol Hypertens. 2014 March ; 23(2): 135–142. doi:10.1097/01.mnh.0000441048.91041.3a. New Insights into the Role of Soluble Guanylate Cyclase in Blood Pressure Regulation Emmanuel Buys1 and Patrick Sips2 1Anesthesia Center for Critical Care Research, Department of Anesthesia, Critical Care and Pain Medicine, Massachusetts General Hospital, Harvard Medical School, Boston, MA, USA 2Division of Cardiovascular Medicine, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA Abstract Purpose of review—Nitric oxide (NO) – soluble guanylate cyclase (sGC)-dependent signaling mechanisms have a profound effect on the regulation of blood pressure. -

Nitric Oxide Lacks Direct Effect on TRPC5 Channels but Suppresses Endogenous TRPC5-Containing Channels in Endothelial Cells
Pflugers Arch - Eur J Physiol (2010) 460:121–130 DOI 10.1007/s00424-010-0823-3 ION CHANNELS, RECEPTORS AND TRANSPORTERS Nitric oxide lacks direct effect on TRPC5 channels but suppresses endogenous TRPC5-containing channels in endothelial cells Ching-On Wong & Piruthivi Sukumar & David J. Beech & Xiaoqiang Yao Received: 25 November 2009 /Revised: 7 March 2010 /Accepted: 9 March 2010 /Published online: 14 April 2010 # Springer-Verlag 2010 Abstract TRPC5 is a member of the canonical transient (SNAP) and diethylamine NONOate (DEA-NONOate) receptor potential (TRPC) family of proteins that forms failed to stimulate or inhibit TRPC5 at concentrations that cationic channels either through homomultimeric assembly generated nitric oxide, caused vasorelaxation, or suppressed or heteromultimeric coordination with other TRPC proteins. activity of TRPC6 via protein kinase G. At high concen- It is expressed in a variety of cells including central neurones trations, SNAP (but not DEA-NONOate) occasionally and endothelial cells and has susceptibility to stimulation by stimulated TRPC5 but the effect was confounded by multiple factors. Here we investigated if TRPC5 is sensitive background TRPC5-independent Ca2+ signals. Endogenous to nitric oxide. Mouse TRPC5 or human TRPC5 was over- Ca2+-entry in bovine aortic endothelial cells (BAECs) was expressed in HEK293 cells, and TRPC5 activity was suppressed by SNAP; TRPC5 blocking antibody or determined by measuring the cytosolic Ca2+ concentration dominant-negative mutant TRPC5 suppressed this Ca2+ with an indicator dye or by recording membrane current entry and occluded the effect of SNAP. The data suggest under voltage clamp. TRPC5 activity could be evoked by that nitric oxide is not a direct modulator of homomeric carbachol acting at muscarinic receptors, lanthanum, or a TRPC5 channels but may inhibit endogenous BAEC reducing agent. -

Nitric Oxide/Cyclic Guanosine Monophosphate Pathway in the Peripheral and Central Auditory System of the Rat
THE JOURNAL OF COMPARATIVE NEUROLOGY 404:52–63 (1999) Nitric Oxide/Cyclic Guanosine Monophosphate Pathway in the Peripheral and Central Auditory System of the Rat JAMES D. FESSENDEN,1 RICHARD A. ALTSCHULER,1 AUDREY F. SEASHOLTZ,2 AND JOCHEN SCHACHT1* 1Kresge Hearing Research Institute, University of Michigan, Ann Arbor, Michigan 48109–0506 2Mental Health Research Institute, University of Michigan, Ann Arbor, Michigan 48109–0720 ABSTRACT The neuronal isoform of nitric oxide synthase (nNOS) and soluble guanylate cyclase (sGC) were localized in the cochlea, the cochlear nucleus (CN), and the superior olivary complex (SOC) of Fisher 344 rats. In the cochlea, nNOS was identified in spiral ganglion cells by using nicotinamide adenine dinucleotide phosphate (NADPH)-diaphorase histochemistry and in situ hybridization. NADPH-diaphorase staining also was detected in blood vessels of the modiolus. By using immunohistochemistry against cyclic guanosine monophosphate, cochlear sGC activity was localized to pericytes in the spiral ligament as well as nerve fibers innervating outer hair cells. In the lower auditory brainstem, nNOS was localized to principal cells of the medial nucleus of the trapezoid body (MNTB) with NADPH-diaphorase histochem- istry and in situ hybridization. NADPH-diaphorase activity also was observed in the lateral and medial superior olive (LSO and MSO, respectively), the superior periolivary nucleus (SPN), the ventral and lateral nuclei of the trapezoid body (VNTB and LNTB, respectively), and the ventral cochlear nucleus (VCN). Transcripts of the -subunit of sGC were localized in rat brainstem by using in situ hybridization. mRNA for sGC was expressed in neurons within the SPN, LSO, MSO, LNTB, MNTB, VNTB, and VCN. -

Sildenafil Reverses O2 Constriction of the Rabbit Ductus Arteriosus by Inhibiting Type 5 Phosphodiesterase and Activating Bkca C
0031-3998/02/5201-0019 PEDIATRIC RESEARCH Vol. 52, No. 1, 2002 Copyright © 2002 International Pediatric Research Foundation, Inc. Printed in U.S.A. Sildenafil Reverses O2 Constriction of the Rabbit Ductus Arteriosus by Inhibiting Type 5 Phosphodiesterase and Activating BKCa Channels BERNARD THÉBAUD, EVANGELOS MICHELAKIS, XI-CHEN WU, GWYNETH HARRY, KYOKO HASHIMOTO, AND STEPHEN L. ARCHER Department of Medicine (Cardiology) and the Vascular Biology Group [B.T., E.M., X.-C.W., G.H., K.H., S.L.A.], Department of Physiology [S.L.A.], University of Alberta, Edmonton, Alberta, T6G 2S2, Canada ABSTRACT Oxygen constriction causes functional closure of the ductus the DA by increasing soluble guanylyl-cyclase–derived cGMP arteriosus (DA) at birth. Although DA closure is crucial for levels and thereby activating calcium-sensitive potassium chan- postnatal adaptation, patency of the DA is critical for survival of nels, causing membrane hyperpolarization. Sildenafil, already newborns with duct-dependent cardiac malformations. In these approved for human usage, might be an alternative or a useful cases, DA patency is achieved by i.v. infusion of prostaglandin adjunct to prostaglandin E1 as a bridge to cardiac surgery. E1, which, though effective, is often associated with complica- (Pediatr Res 52: 19–24, 2002) tions. We hypothesized that sildenafil, a specific phosphodiester- ase type 5 inhibitor, is an effective DA vasodilator. In isolated Abbreviations DA rings from term (d 30) fetal rabbits, sildenafil (10Ϫ6–10Ϫ4 4-AP, 4-aminopyridine Ϫ7 Ϫ5 M) and diethylamine NONOate (10 –10 M) induced dose- BKCa, large conductance calcium-sensitive potassium channels dependent relaxation of oxygen-constricted DA (Ϫ52 Ϯ 4% and cGMP, 3',5'-cyclic GMP Ϫ51 Ϯ 6%, respectively) that was inhibited by the soluble DA, ductus arteriosus guanylyl-cyclase inhibitor, 1H-[1,2,4]oxadiazolo[4,3-a]quinoxa- DASMC, DA smooth muscle cells lin-1-one (5 ϫ 10Ϫ5 M). -

Nitric Oxide Generation Kit
Nitric Oxide Generation Kit This kit contains 10 mg each of the following nitric oxide donors: SIN-1, SNAP, S-nitrosoglutathione, spermine NONOate, and DEA-NONOate Instruct ion Manual Catalog Number PK-CA707-00239 Kit contains 5 x 10 mg (10 mg each of the following nitric oxide donors: Quantity SIN-1, SNAP, S-nitrosoglutathione, spermine NONOate, and DEA-NONOate) Individual Kit Components Product Name SIN-1 Molecular Formula C6H10 N4O Molecular Weight 206.7 Molecular Structure Synonyms Morpholinosydnonimine, hydrochloride Purity 95% as determined by TLC. Formulation White solid. Solubility Soluble in water, methanol or DMSO. Applications SIN-1 releases nitric oxide and forms superoxide spontaneously under physiological conditions and stimulates cyclic GMP production. It has been shown to be a potent vasodilator in vivo and in vitro and to inhibit smooth muscle cell mitogenesis and proliferation. The relationship between NO generated from SIN-1 and intracellular calcium has been studied using fluorescent calcium indictors, which are also available from PromoCell. Storage & Stability Store desiccated at -20°C. References 1) Nature 364, 626(1993); 2) J. Pharmacol. Exp. Ther. 248, 762(1989); 3) Am J Physiol, L9 (1994); 4) Life Sci 54, 1449 (1994); 5) Neuron 12, 1235 (1994). Product Name SNAP Molecular Formula C7H12 N2O4S Molecular Weight 220 Molecular Structure Synonyms S-nitroso-N-acetylpenicillamine Purity 98% as determined by TLC. Formulation Light green solid. Solubility Soluble in water or DMSO. 2 Instruction Manual Applications SNAP releases nitric oxide and forms superoxide spontaneously under physiological conditions and stimulates cyclic GMP production. It has been shown to be a potent vasodilator in vivo and in vitro and to inhibit smooth muscle cell mitogenesis and proliferation. -

A Proatherogenic Role for Cgmp-Dependent Protein Kinase in Vascular Smooth Muscle Cells
A proatherogenic role for cGMP-dependent protein kinase in vascular smooth muscle cells Wiebke Wolfsgruber*, Susanne Feil*, Sabine Brummer, Oliver Kuppinger, Franz Hofmann, and Robert Feil† Institut fu¨r Pharmakologie und Toxikologie, Technische Universita¨t, Biedersteiner Strasse 29, 80802 Munich, Germany Communicated by Joseph A. Beavo, University of Washington School of Medicine, Seattle, WA, September 18, 2003 (received for review May 19, 2003) Nitric oxide (NO) exerts both antiatherogenic and proatherogenic cGKI modulates the properties of aortic SMCs in vitro and in vivo effects, but the cellular and molecular mechanisms that contribute and promotes atherosclerosis. to modulation of atherosclerosis by NO are not understood com- pletely. The cGMP-dependent protein kinase I (cGKI) is a potential Materials and Methods mediator of NO signaling in vascular smooth muscle cells (SMCs). Experimental Animals. The generation of mice carrying a condi- Postnatal ablation of cGKI selectively in the SMCs of mice reduced tional loxP-flanked cGKI allele (L2) or a recombined cGKI-null atherosclerotic lesion area, demonstrating that smooth muscle allele (LϪ) and the detection of the cGKI WT(ϩ), L2, and LϪ cGKI promotes atherogenesis. Cell-fate mapping indicated that alleles by PCR have been described (14). Mice carrying the cGKI is involved in the development of SMC-derived plaque cells. SM-CreERT2 knock-in allele (Cre) were genotyped as described Activation of endogenous cGKI in primary aortic SMCs resulted in (15). Mice carrying the ROSA26 Cre reporter (R26R) (16) or cells with increased levels of proliferation; increased levels of ApoE-null (17) alleles were obtained from The Jackson Labo- vascular cell adhesion molecule-1, peroxisome proliferator-acti- ratory and genotyped according to published protocols (avail- vated receptor ␥, and phosphatidylinositol 3-kinase͞Akt signaling; able at www.jax.org).