Nitroxyl Gets to the Heart of the Matter
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

A Biochemical Rationale for the Discrete Behavior of Nitroxyl and Nitric Oxide in the Cardiovascular System
A biochemical rationale for the discrete behavior of nitroxyl and nitric oxide in the cardiovascular system Katrina M. Miranda*†‡, Nazareno Paolocci§, Tatsuo Katori§, Douglas D. Thomas*, Eleonora Ford¶, Michael D. Bartbergerʈ, Michael G. Espey*, David A. Kass§, Martin Feelisch**, Jon M. Fukuto¶, and David A. Wink*† *Radiation Biology Branch, Building 10, Room B3-B69, National Cancer Institute, National Institutes of Health, Bethesda, MD 20892; §Division of Cardiology, Department of Medicine, The Johns Hopkins Medical Institutions, Baltimore, MD 21287; ¶Department of Molecular and Medical Pharmacology, Center for the Health Sciences, University of California, Los Angeles, CA 90095; ʈDepartment of Chemistry and Biochemistry, University of California, Los Angeles, CA 90095; and **Department of Molecular and Cellular Physiology, Louisiana State University Health Sciences Center, Shreveport, LA 71130 Edited by Louis J. Ignarro, University of California School of Medicine, Los Angeles, CA, and approved May 20, 2003 (received for review February 20, 2003) The redox siblings nitroxyl (HNO) and nitric oxide (NO) have often cellular thiol functions (14, 15). Conversely, NO reacts only indi- been assumed to undergo casual redox reactions in biological sys- rectly with thiols after RNOS formation (17). tems. However, several recent studies have demonstrated distinct Contrasting effects are also apparent in vivo or ex vivo,for pharmacological effects for donors of these two species. Here, infu- example in models of ischemia reperfusion injury. Exposure to NO sion of the HNO donor Angeli’s salt into normal dogs resulted in donors at the onset of reperfusion provides protection against elevated plasma levels of calcitonin gene-related peptide, whereas reperfusion injury in the heart and other organs (18–20). -
Download Product Insert (PDF)
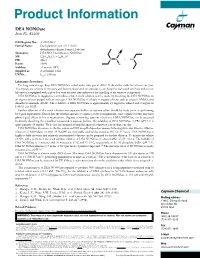
Product Information DEA NONOate Item No. 82100 CAS Registry No.: 372965-00-9 Formal Name: Diethylammonium (Z)-1-(N,N- diethylamino)diazen-1-ium-1,2-diolate O Synonyms: DEA/NO, Diethylamine NONOate N MF: C4H10N3O2 • C4H12N + N N • H N FW: 206.3 2 Purity: ≥98% O- Stability: ≥1 year at -80°C Supplied as: A crystalline solid l UV/Vis.: max: 250 nm Laboratory Procedures For long term storage, keep DEA NONOate sealed under nitrogen at -80°C. It should be stable for at least one year. The crystals are sensitive to moisture and become discolored on exposure to air. Keep the vial sealed until use unless your laboratory is equipped with a glove box with an inert atmosphere for the handling of air sensitive compounds. DEA NONOate is supplied as a crystalline solid. A stock solution may be made by dissolving the DEA NONOate in an organic solvent purged with an inert gas. DEA NONOate is soluble in organic solvents such as ethanol, DMSO, and dimethyl formamide (DMF). The solubility of DEA NONOate is approximately 25 mg/ml in ethanol and 2 mg/ml in DMSO and DMF. Further dilutions of the stock solution into aqueous buffers or isotonic saline should be made prior to performing biological experiments. Ensure that the residual amount of organic solvent is insignificant, since organic solvents may have physiological effects at low concentrations. Organic solvent-free aqueous solutions of DEA NONOate can be prepared by directly dissolving the crystalline compound in aqueous buffers. The solubility of DEA NONOate in PBS (pH 7.2) is approximately 10 mg/ml. -

Hidden Complexities in the Reaction of H2O2 and HNO Revealed by Ab Initio Quantum Chemical Cite This: Phys
PCCP PAPER Hidden complexities in the reaction of H2O2 and HNO revealed by ab initio quantum chemical Cite this: Phys. Chem. Chem. Phys., 2017, 19, 29549 investigations† Daniel Beckett, Marc Edelmann, Jonathan D. Raff and Krishnan Raghavachari* Nitroxyl (HNO) and hydrogen peroxide have both been implicated in a variety of reactions relevant to environmental and physiological processes and may contribute to a unique, unexplored, pathway for the production of nitrous acid (HONO) in soil. To investigate the potential for this reaction, we report an in-depth investigation of the reaction pathway of H2O2 and HNO forming HONO and water. We find the breaking of the peroxide bond and a coupled proton transfer in the first step leads to hydrogen nitryl (HNO2) and an endogenous water, with an extrapolated NEVPT2 (multireference perturbation theory) barrier of 29.3 kcal molÀ1. The first transition state is shown to possess diradical character linking the far peroxide oxygen to the bridging, reacting, peroxide oxygen. The energy of this first step, when calculated using hybrid density functional theory, is shown to depend heavily on the amount of Hartree–Fock exchange in the functional, with higher amounts leading to a higher barrier and more diradical character. Additionally, high amounts of spin contamination cause CCSD(T) to significantly overestimate the TS1 barrier with a value of 36.2 kcal molÀ1 when using the stable UHF wavefunction as the reference wavefunction. However, when using the restricted Hartree–Fock reference wavefunction, the TS1 CCSD(T) energy is lowered to yield a barrier of 31.2 kcal molÀ1, in much better agreement with the Received 29th August 2017, NEVPT2 result. -

Nitroaromatic Antibiotics As Nitrogen Oxide Sources
Review biomolecules Nitroaromatic Antibiotics as Nitrogen Oxide Sources Review Allison M. Rice, Yueming Long and S. Bruce King * Nitroaromatic Antibiotics as Nitrogen Oxide Sources Department of Chemistry and Biochemistry, Wake Forest University, Winston-Salem, NC 27101, USA; Allison M. Rice , Yueming [email protected] and S. Bruce (A.M.R.); King [email protected] * (Y.L.) * Correspondence: [email protected]; Tel.: +1-336-702-1954 Department of Chemistry and Biochemistry, Wake Forest University, Winston-Salem, NC 27101, USA; [email protected]: Nitroaromatic (A.M.R.); [email protected] antibiotics (Y.L.) show activity against anaerobic bacteria and parasites, finding * Correspondence: [email protected]; Tel.: +1-336-702-1954 use in the treatment of Heliobacter pylori infections, tuberculosis, trichomoniasis, human African trypanosomiasis, Chagas disease and leishmaniasis. Despite this activity and a clear need for the Abstract: Nitroaromatic antibiotics show activity against anaerobic bacteria and parasites, finding usedevelopment in the treatment of new of Heliobacter treatments pylori forinfections, these conditio tuberculosis,ns, the trichomoniasis, associated toxicity human Africanand lack of clear trypanosomiasis,mechanisms of action Chagas have disease limited and their leishmaniasis. therapeutic Despite development. this activity Nitroaro and a clearmatic need antibiotics for require thereductive development bioactivation of new treatments for activity for theseand this conditions, reductive the associatedmetabolism toxicity can convert -

Current Advances of Nitric Oxide in Cancer and Anticancer Therapeutics
Review Current Advances of Nitric Oxide in Cancer and Anticancer Therapeutics Joel Mintz 1,†, Anastasia Vedenko 2,†, Omar Rosete 3 , Khushi Shah 4, Gabriella Goldstein 5 , Joshua M. Hare 2,6,7 , Ranjith Ramasamy 3,6,* and Himanshu Arora 2,3,6,* 1 Dr. Kiran C. Patel College of Allopathic Medicine, Nova Southeastern University, Davie, FL 33328, USA; [email protected] 2 John P Hussman Institute for Human Genomics, Miller School of Medicine, University of Miami, Miami, FL 33136, USA; [email protected] (A.V.); [email protected] (J.M.H.) 3 Department of Urology, Miller School of Medicine, University of Miami, Miami, FL 33136, USA; [email protected] 4 College of Arts and Sciences, University of Miami, Miami, FL 33146, USA; [email protected] 5 College of Health Professions and Sciences, University of Central Florida, Orlando, FL 32816, USA; [email protected] 6 The Interdisciplinary Stem Cell Institute, Miller School of Medicine, University of Miami, Miami, FL 33136, USA 7 Department of Medicine, Cardiology Division, Miller School of Medicine, University of Miami, Miami, FL 33136, USA * Correspondence: [email protected] (R.R.); [email protected] (H.A.) † These authors contributed equally to this work. Abstract: Nitric oxide (NO) is a short-lived, ubiquitous signaling molecule that affects numerous critical functions in the body. There are markedly conflicting findings in the literature regarding the bimodal effects of NO in carcinogenesis and tumor progression, which has important consequences for treatment. Several preclinical and clinical studies have suggested that both pro- and antitumori- Citation: Mintz, J.; Vedenko, A.; genic effects of NO depend on multiple aspects, including, but not limited to, tissue of generation, the Rosete, O.; Shah, K.; Goldstein, G.; level of production, the oxidative/reductive (redox) environment in which this radical is generated, Hare, J.M; Ramasamy, R.; Arora, H. -

Nitroglycerin Sublingual Tablets, USP)
NDA 021134/S-004 Page 4 Nitrostat® (Nitroglycerin Sublingual Tablets, USP) DESCRIPTION Nitrostat is a stabilized sublingual compressed nitroglycerin tablet that contains 0.3 mg , 0.4 mg , or 0.6 mg nitroglycerin; as well as lactose monohydrate, NF; glyceryl monostearate, NF; pregelatinized starch, NF; calcium stearate, NF powder; and silicon dioxide, colloidal, NF. Nitroglycerin, an organic nitrate, is a vasodilating agent. The chemical name for nitroglycerin is 1, 2, 3 propanetriol trinitrate and the chemical structure is: NO2 O O N O CH2CHCH2 O NO 2 2 C3H5N309 Molecular weight: 227.09 CLINICAL PHARMACOLOGY The principal pharmacological action of nitroglycerin is relaxation of vascular smooth muscle. Although venous effects predominate, nitroglycerin produces, in a dose-related manner, dilation of both arterial and venous beds. Dilation of postcapillary vessels, including large veins, promotes peripheral pooling of blood, decreases venous return to the heart, and reduces left ventricular end-diastolic pressure (preload). Nitroglycerin also produces arteriolar relaxation, thereby reducing peripheral vascular resistance and arterial pressure (afterload), and dilates large epicardial coronary arteries; however, the extent to which this latter effect contributes to the relief of exertional angina is unclear. Therapeutic doses of nitroglycerin may reduce systolic, diastolic, and mean arterial blood pressure. Effective coronary perfusion pressure is usually maintained, but can be compromised if blood pressure falls excessively, or increased heart rate decreases diastolic filling time. Elevated central venous and pulmonary capillary wedge pressures, and pulmonary and systemic vascular resistance are also reduced by nitroglycerin therapy. Heart rate is usually slightly increased, presumably due to a compensatory response to the fall in blood pressure. -

On the Distinction Between Nitroxyl and Nitric Oxide Using Nitronyl Nitroxides
Published on Web 05/26/2010 On the Distinction between Nitroxyl and Nitric Oxide Using Nitronyl Nitroxides Uri Samuni,† Yuval Samuni,‡ and Sara Goldstein*,§ Department of Chemistry and Biochemistry, Queens College, City UniVersity of New York, Flushing, New York 11367, and Department of Prosthodontics, School of Dental Medicine, and Institute of Chemistry, The Accelerator Laboratory, The Hebrew UniVersity of Jerusalem, Jerusalem 91904, Israel Received March 8, 2010; E-mail: [email protected] Abstract: A better understanding of the origins of NO and HNO and their activities and biological functions requires accurate methods for their detection and quantification. The unique reaction of NO with nitronyl nitroxides such as 2-(4-carboxyphenyl)-4,4,5,5-tetramethylimidazoline-1-oxyl 3-oxide (C-PTIO), which yields the corresponding imino nitroxides, is widely used for NO detection (mainly by electron paramagnetic resonance spectroscopy) and for modulation of NO-induced physiological functions. The present study demonstrates that HNO readily reacts with nitronyl nitroxides, leading to the formation of the respective imino nitroxides and hydroxylamines via a complex mechanism. Through the use of the HNO donor Angeli’s salt (AS) with metmyoglobin as a competing agent, the rate constant for C-PTIO reduction by HNO has been determined to be (1.4 ( 0.2) × 105 M-1 s-1 at pH 7.0. This reaction yields the corresponding nitronyl • hydroxylamine C-PTIO-H and NO, which is trapped by C-PTIO to form NO2 and the corresponding imino • nitroxide, C-PTI. NO2 oxidizes the nitronyl and imino nitroxides to their respective oxoammonium cations, which decay mainly via comproportionation with the nitronyl and imino hydroxylamines. -

Nitric Oxide Attenuates Hypoxia-Induced 5-FU Resistance
Sasabe et al. Int J Cancer Clin Res 2015, 2:2 DOI: 10.23937/2378-3419/2/2/1014 International Journal of Cancer and Clinical Research ISSN: 2378-3419 Original Article: Open Access Nitric Oxide Attenuates Hypoxia-Induced 5-FU Resistance of Oral Squamous Cell Carcinoma Cells Eri Sasabe*, Ayumi Tomomura, Mayuko Hamada, Naoya Kitamura, Tomohiro Yamada and Tetsuya Yamamoto Department of Oral and Maxillofacial Surgery, Kochi Medical School, Kochi University Kohasu, Japan *Corresponding author: Eri Sasabe, Department of Oral and Maxillofacial Surgery, Kochi Medical School, Kochi University Kohasu, Oko-cho, Nankoku, Kochi 783-8505, Japan, Tel: +81-88-880-2423, Fax: +81-88-880-2424, E-mail: [email protected] to development and progression of malignancies, and resistance Abstract to cancer therapy. The heterodimeric transcription factor Hypoxia Hypoxic environments in tumors induce expression of hypoxia- inducible factor (HIF) is a master regulator that can adapt tumor cells inducible factor (HIF). HIF contributes to the development of the to hypoxic conditions [1]. Overexpression of HIF has been observed malignant progression through the induction of various target genes. in many different cancers, including head and neck squamous cell We previously reported that treatment with chemotherapeutic drugs and γ-rays enhances expression and nuclear translocation carcinomas, and is associated with increased patient mortality [2-4]. of HIF-1α under normoxic conditions; susceptibility of oral HIF consists of an oxygen-regulated α-subunit and a constitutively squamous cell carcinoma (OSCC) cells to the drugs and γ-rays expressed β-subunit, also known as aryl hydrocarbon receptor is negatively correlated with expression of HIF-1α protein. -

Nitroxyl-Mediated Peroxide Modification of Polypropylene
Nitroxyl-Mediated Peroxide Modification of Polypropylene by Benjamin Rhys Jones A thesis submitted to the Department of Chemical Engineering In conformity with the requirements for the degree of Master of Applied Science Queen’s University Kingston, Ontario, Canada (May 2021) Copyright ©Benjamin Rhys Jones, 2021 Abstract The thermal stability of alkoxyamine derivatives of polypropylene (PP) is examined through studies of model hydrocarbon systems and atactic-PP substrates. Primary, secondary and tertiary alkoxyamines are integral to modern techniques for modifying the architecture of linear PP materials, and detailed knowledge of their stability at polymer processing temperatures is needed to further understand the underlying principles of nitroxyl-based formulations. GC analysis of alkoxyamines derived from 2,4-dimethylpentane + TEMPO show that the tertiary regioisomer is susceptible to disproportionation to alkene + HOTEMPO at temperatures as low as 140 oC. Extension of these thermolysis experiments to atactic PP-g-HOTEMPO mirrored the model compound results, with appreciable extents of nitroxyl generation observed over a 20 min timescale at 180 oC. This reaction extent is not expected to dramatically alter the performance of nitroxyl-based formulations that modify the structure and composition of PP homopolymers. The yield of H-atom abstraction by peroxide-derived alkoxy radicals is another fundamental reaction that underlies polyolefin modifications. Indirect measures based on analysis of peroxide byproducts are supplemented with a fluorescence spectroscopy method that quantifies polymer- bound alkoxyamines. H-atom transfer from high density polyethylene (HDPE) and poly(ethylene-co-propylene) (EPR) was gained by using napthoyloxy-TEMPO, whose fluorophore supports a highly sensitive analytical method. This technique is extended to studies of reactive HDPE/EPR blending to ascertain the extent of peroxide migration from one phase to the other during the compounding process. -
NITROGYLCERIN and ETHYLENE GLYCOL DINITRATE Criteria for a Recommended Standard OCCUPATIONAL EXPOSURE to NITROGLYCERIN and ETHYLENE GLYCOL DINITRATE
CRITERIA FOR A RECOMMENDED STANDARD OCCUPATIONAL EXPOSURE TO NITROGYLCERIN and ETHYLENE GLYCOL DINITRATE criteria for a recommended standard OCCUPATIONAL EXPOSURE TO NITROGLYCERIN and ETHYLENE GLYCOL DINITRATE U.S. DEPARTMENT OF HEALTH, EDUCATION, AND WELFARE Public Health Service Center for Disease Control National Institute for Occupational Safety and Health June 1978 For »ale by the Superintendent of Documents, U.S. Government Printing Office, Washington, D.C. 20402 DISCLAIMER Mention of company name or products does not constitute endorsement by the National Institute for Occupational Safety and Health. DHEW (NIOSH) Publication No. 78-167 PREFACE The Occupational Safety and Health Act of 1970 emphasizes the need for standards to protect the health and provide for the safety of workers occupationally exposed to an ever-increasing number of potential hazards. The National Institute for Occupational Safety and Health (NIOSH) evaluates all available research data and criteria and recommends standards for occupational exposure. The Secretary of Labor will weigh these recommendations along with other considerations, such as feasibility and means of implementation, in promulgating regulatory standards. NIOSH will periodically review the recommended standards to ensure continuing protection of workers and will make successive reports as new research and epidemiologic studies are completed and as sampling and analytical methods are developed. The contributions to this document on nitroglycerin (NG) and ethylene glycol dinitrate (EGDN) by NIOSH staff, other Federal agencies or departments, the review consultants, the reviewers selected by the American Industrial Hygiene Association, and by Robert B. O ’Connor, M.D., NIOSH consultant in occupational medicine, are gratefully acknowledged. The views and conclusions expressed in this document, together with the recommendations for a standard, are those of NIOSH. -

Oxidative Stress and the Guanosine Nucleotide Triphosphate Pool: Implications for a Biomarker and Mechanism of Impaired Cell Function
University of Montana ScholarWorks at University of Montana Graduate Student Theses, Dissertations, & Professional Papers Graduate School 2008 OXIDATIVE STRESS AND THE GUANOSINE NUCLEOTIDE TRIPHOSPHATE POOL: IMPLICATIONS FOR A BIOMARKER AND MECHANISM OF IMPAIRED CELL FUNCTION Celeste Maree Bolin The University of Montana Follow this and additional works at: https://scholarworks.umt.edu/etd Let us know how access to this document benefits ou.y Recommended Citation Bolin, Celeste Maree, "OXIDATIVE STRESS AND THE GUANOSINE NUCLEOTIDE TRIPHOSPHATE POOL: IMPLICATIONS FOR A BIOMARKER AND MECHANISM OF IMPAIRED CELL FUNCTION" (2008). Graduate Student Theses, Dissertations, & Professional Papers. 728. https://scholarworks.umt.edu/etd/728 This Dissertation is brought to you for free and open access by the Graduate School at ScholarWorks at University of Montana. It has been accepted for inclusion in Graduate Student Theses, Dissertations, & Professional Papers by an authorized administrator of ScholarWorks at University of Montana. For more information, please contact [email protected]. OXIDATIVE STRESS AND THE GUANOSINE NUCLEOTIDE TRIPHOSPHATE POOL: IMPLICATIONS FOR A BIOMARKER AND MECHANISM OF IMPAIRED CELL FUNCTION By Celeste Maree Bolin B.A. Chemistry, Whitman College, Walla Walla, WA 2001 Dissertation presented in partial fulfillment of the requirements for the degree of Doctor of Philosophy in Toxicology The University of Montana Missoula, Montana Spring 2008 Approved by: Dr. David A. Strobel, Dean Graduate School Dr. Fernando Cardozo-Pelaez, -

Sustained Formation of Nitroglycerin-Derived Nitric Oxide
Supplemental material to this article can be found at: http://molpharm.aspetjournals.org/content/suppl/2018/01/22/mol.117.110783.DC1 1521-0111/93/4/335–343$35.00 https://doi.org/10.1124/mol.117.110783 MOLECULAR PHARMACOLOGY Mol Pharmacol 93:335–343, April 2018 Copyright ª 2018 The Author(s). This is an open access article distributed under the CC BY Attribution 4.0 International license. Sustained Formation of Nitroglycerin-Derived Nitric Oxide by Aldehyde Dehydrogenase-2 in Vascular Smooth Muscle without Added Reductants: Implications for the Development of Nitrate Tolerance s Marissa Opelt, Gerald Wölkart, Emrah Eroglu, Markus Waldeck-Weiermair, Roland Malli, Wolfgang F. Graier, Alexander Kollau, John T. Fassett, Astrid Schrammel, Bernd Mayer, and Antonius C. F. Gorren Downloaded from Institute of Pharmaceutical Sciences, Department of Pharmacology and Toxicology, Karl-Franzens University (M.O., G.W., A.K., J.T.F., A.S., B.M., A.C.F.G.), and Institute of Molecular Biology and Biochemistry, Center of Molecular Medicine, Medical University Graz (E.E., M.W.-W., R.M., W.F.G.), Graz, Austria Received October 4, 2017; accepted January 18, 2018 molpharm.aspetjournals.org ABSTRACT According to current views, oxidation of aldehyde dehydrogenase-2 ALDH2, thiol-refractive inactivation was observed, particularly under (ALDH2) during glyceryltrinitrate (GTN) biotransformation is essen- high-turnover conditions. Organ bath experiments with rat aortas tially involved in vascular nitrate tolerance and explains the de- showed that relaxation by GTN lasted longer than that caused by the pendence of this reaction on added thiols. Using a novel fluorescent NO donor diethylamine/NONOate, in line with the long-lasting intracellular nitric oxide (NO) probe expressed in vascular smooth nanomolar NO generation from GTN observed in VSMCs.