Molecular Mechanism and Metabolic Function of the S
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Biochemical Rationale for the Discrete Behavior of Nitroxyl and Nitric Oxide in the Cardiovascular System
A biochemical rationale for the discrete behavior of nitroxyl and nitric oxide in the cardiovascular system Katrina M. Miranda*†‡, Nazareno Paolocci§, Tatsuo Katori§, Douglas D. Thomas*, Eleonora Ford¶, Michael D. Bartbergerʈ, Michael G. Espey*, David A. Kass§, Martin Feelisch**, Jon M. Fukuto¶, and David A. Wink*† *Radiation Biology Branch, Building 10, Room B3-B69, National Cancer Institute, National Institutes of Health, Bethesda, MD 20892; §Division of Cardiology, Department of Medicine, The Johns Hopkins Medical Institutions, Baltimore, MD 21287; ¶Department of Molecular and Medical Pharmacology, Center for the Health Sciences, University of California, Los Angeles, CA 90095; ʈDepartment of Chemistry and Biochemistry, University of California, Los Angeles, CA 90095; and **Department of Molecular and Cellular Physiology, Louisiana State University Health Sciences Center, Shreveport, LA 71130 Edited by Louis J. Ignarro, University of California School of Medicine, Los Angeles, CA, and approved May 20, 2003 (received for review February 20, 2003) The redox siblings nitroxyl (HNO) and nitric oxide (NO) have often cellular thiol functions (14, 15). Conversely, NO reacts only indi- been assumed to undergo casual redox reactions in biological sys- rectly with thiols after RNOS formation (17). tems. However, several recent studies have demonstrated distinct Contrasting effects are also apparent in vivo or ex vivo,for pharmacological effects for donors of these two species. Here, infu- example in models of ischemia reperfusion injury. Exposure to NO sion of the HNO donor Angeli’s salt into normal dogs resulted in donors at the onset of reperfusion provides protection against elevated plasma levels of calcitonin gene-related peptide, whereas reperfusion injury in the heart and other organs (18–20). -

Remodeling Adipose Tissue Through in Silico Modulation of Fat Storage For
Chénard et al. BMC Systems Biology (2017) 11:60 DOI 10.1186/s12918-017-0438-9 RESEARCHARTICLE Open Access Remodeling adipose tissue through in silico modulation of fat storage for the prevention of type 2 diabetes Thierry Chénard2, Frédéric Guénard3, Marie-Claude Vohl3,4, André Carpentier5, André Tchernof4,6 and Rafael J. Najmanovich1* Abstract Background: Type 2 diabetes is one of the leading non-infectious diseases worldwide and closely relates to excess adipose tissue accumulation as seen in obesity. Specifically, hypertrophic expansion of adipose tissues is related to increased cardiometabolic risk leading to type 2 diabetes. Studying mechanisms underlying adipocyte hypertrophy could lead to the identification of potential targets for the treatment of these conditions. Results: We present iTC1390adip, a highly curated metabolic network of the human adipocyte presenting various improvements over the previously published iAdipocytes1809. iTC1390adip contains 1390 genes, 4519 reactions and 3664 metabolites. We validated the network obtaining 92.6% accuracy by comparing experimental gene essentiality in various cell lines to our predictions of biomass production. Using flux balance analysis under various test conditions, we predict the effect of gene deletion on both lipid droplet and biomass production, resulting in the identification of 27 genes that could reduce adipocyte hypertrophy. We also used expression data from visceral and subcutaneous adipose tissues to compare the effect of single gene deletions between adipocytes from each -

Primate Specific Retrotransposons, Svas, in the Evolution of Networks That Alter Brain Function
Title: Primate specific retrotransposons, SVAs, in the evolution of networks that alter brain function. Olga Vasieva1*, Sultan Cetiner1, Abigail Savage2, Gerald G. Schumann3, Vivien J Bubb2, John P Quinn2*, 1 Institute of Integrative Biology, University of Liverpool, Liverpool, L69 7ZB, U.K 2 Department of Molecular and Clinical Pharmacology, Institute of Translational Medicine, The University of Liverpool, Liverpool L69 3BX, UK 3 Division of Medical Biotechnology, Paul-Ehrlich-Institut, Langen, D-63225 Germany *. Corresponding author Olga Vasieva: Institute of Integrative Biology, Department of Comparative genomics, University of Liverpool, Liverpool, L69 7ZB, [email protected] ; Tel: (+44) 151 795 4456; FAX:(+44) 151 795 4406 John Quinn: Department of Molecular and Clinical Pharmacology, Institute of Translational Medicine, The University of Liverpool, Liverpool L69 3BX, UK, [email protected]; Tel: (+44) 151 794 5498. Key words: SVA, trans-mobilisation, behaviour, brain, evolution, psychiatric disorders 1 Abstract The hominid-specific non-LTR retrotransposon termed SINE–VNTR–Alu (SVA) is the youngest of the transposable elements in the human genome. The propagation of the most ancient SVA type A took place about 13.5 Myrs ago, and the youngest SVA types appeared in the human genome after the chimpanzee divergence. Functional enrichment analysis of genes associated with SVA insertions demonstrated their strong link to multiple ontological categories attributed to brain function and the disorders. SVA types that expanded their presence in the human genome at different stages of hominoid life history were also associated with progressively evolving behavioural features that indicated a potential impact of SVA propagation on a cognitive ability of a modern human. -

Transcriptomic Analysis of Staphylococcus Xylosus in Solid Dairy Matrix Reveals an Aerobic Lifestyle Adapted to Rind
microorganisms Article Transcriptomic Analysis of Staphylococcus xylosus in Solid Dairy Matrix Reveals an Aerobic Lifestyle Adapted to Rind 1, 2 1, 3, 4 Sabine Leroy *, Sergine Even , Pierre Micheau y, Anne de La Foye y, Valérie Laroute , Yves Le Loir 2 and Régine Talon 1 1 Université Clermont Auvergne, INRAE, MEDIS, Clermont-Ferrand, France; [email protected] (P.M.); [email protected] (R.T.) 2 INRAE, Agrocampus Ouest, STLO, Rennes, France; [email protected] (S.E.); [email protected] (Y.L.L.) 3 INRAE, UMRH, Saint-Genès-Champanelle, France; [email protected] 4 TBI, Université de Toulouse, CNRS, INRAE, Toulouse, France; [email protected] * Correspondence: [email protected] Current address: Université Clermont Auvergne, INRAE, UNH, Clermont-Ferrand, France. y Received: 26 October 2020; Accepted: 14 November 2020; Published: 17 November 2020 Abstract: Staphylococcus xylosus is found in the microbiota of traditional cheeses, particularly in the rind of soft smeared cheeses. Despite its frequency, the molecular mechanisms allowing the growth and adaptation of S. xylosus in dairy products are still poorly understood. A transcriptomic approach was used to determine how the gene expression profile is modified during the fermentation step in a solid dairy matrix. S. xylosus developed an aerobic metabolism perfectly suited to the cheese rind. It overexpressed genes involved in the aerobic catabolism of two carbon sources in the dairy matrix, lactose and citrate. Interestingly, S. xylosus must cope with nutritional shortage such as amino acids, peptides, and nucleotides, consequently, an extensive up-regulation of genes involved in their biosynthesis was observed. -

Supplementary Materials
Supplementary Materials Figure S1. Differentially abundant spots between the mid-log phase cells grown on xylan or xylose. Red and blue circles denote spots with increased and decreased abundance respectively in the xylan growth condition. The identities of the circled spots are summarized in Table 3. Figure S2. Differentially abundant spots between the stationary phase cells grown on xylan or xylose. Red and blue circles denote spots with increased and decreased abundance respectively in the xylan growth condition. The identities of the circled spots are summarized in Table 4. S2 Table S1. Summary of the non-polysaccharide degrading proteins identified in the B. proteoclasticus cytosol by 2DE/MALDI-TOF. Protein Locus Location Score pI kDa Pep. Cov. Amino Acid Biosynthesis Acetylornithine aminotransferase, ArgD Bpr_I1809 C 1.7 × 10−4 5.1 43.9 11 34% Aspartate/tyrosine/aromatic aminotransferase Bpr_I2631 C 3.0 × 10−14 4.7 43.8 15 46% Aspartate-semialdehyde dehydrogenase, Asd Bpr_I1664 C 7.6 × 10−18 5.5 40.1 17 50% Branched-chain amino acid aminotransferase, IlvE Bpr_I1650 C 2.4 × 10−12 5.2 39.2 13 32% Cysteine synthase, CysK Bpr_I1089 C 1.9 × 10−13 5.0 32.3 18 72% Diaminopimelate dehydrogenase Bpr_I0298 C 9.6 × 10−16 5.6 35.8 16 49% Dihydrodipicolinate reductase, DapB Bpr_I2453 C 2.7 × 10−6 4.9 27.0 9 46% Glu/Leu/Phe/Val dehydrogenase Bpr_I2129 C 1.2 × 10−30 5.4 48.6 31 64% Imidazole glycerol phosphate synthase Bpr_I1240 C 8.0 × 10−3 4.7 22.5 8 44% glutamine amidotransferase subunit Ketol-acid reductoisomerase, IlvC Bpr_I1657 C 3.8 × 10−16 -
Download Product Insert (PDF)
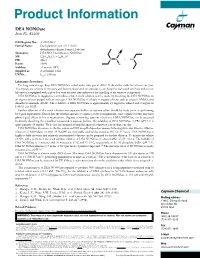
Product Information DEA NONOate Item No. 82100 CAS Registry No.: 372965-00-9 Formal Name: Diethylammonium (Z)-1-(N,N- diethylamino)diazen-1-ium-1,2-diolate O Synonyms: DEA/NO, Diethylamine NONOate N MF: C4H10N3O2 • C4H12N + N N • H N FW: 206.3 2 Purity: ≥98% O- Stability: ≥1 year at -80°C Supplied as: A crystalline solid l UV/Vis.: max: 250 nm Laboratory Procedures For long term storage, keep DEA NONOate sealed under nitrogen at -80°C. It should be stable for at least one year. The crystals are sensitive to moisture and become discolored on exposure to air. Keep the vial sealed until use unless your laboratory is equipped with a glove box with an inert atmosphere for the handling of air sensitive compounds. DEA NONOate is supplied as a crystalline solid. A stock solution may be made by dissolving the DEA NONOate in an organic solvent purged with an inert gas. DEA NONOate is soluble in organic solvents such as ethanol, DMSO, and dimethyl formamide (DMF). The solubility of DEA NONOate is approximately 25 mg/ml in ethanol and 2 mg/ml in DMSO and DMF. Further dilutions of the stock solution into aqueous buffers or isotonic saline should be made prior to performing biological experiments. Ensure that the residual amount of organic solvent is insignificant, since organic solvents may have physiological effects at low concentrations. Organic solvent-free aqueous solutions of DEA NONOate can be prepared by directly dissolving the crystalline compound in aqueous buffers. The solubility of DEA NONOate in PBS (pH 7.2) is approximately 10 mg/ml. -

Genetic and Genomic Analysis of Hyperlipidemia, Obesity and Diabetes Using (C57BL/6J × TALLYHO/Jngj) F2 Mice
University of Tennessee, Knoxville TRACE: Tennessee Research and Creative Exchange Nutrition Publications and Other Works Nutrition 12-19-2010 Genetic and genomic analysis of hyperlipidemia, obesity and diabetes using (C57BL/6J × TALLYHO/JngJ) F2 mice Taryn P. Stewart Marshall University Hyoung Y. Kim University of Tennessee - Knoxville, [email protected] Arnold M. Saxton University of Tennessee - Knoxville, [email protected] Jung H. Kim Marshall University Follow this and additional works at: https://trace.tennessee.edu/utk_nutrpubs Part of the Animal Sciences Commons, and the Nutrition Commons Recommended Citation BMC Genomics 2010, 11:713 doi:10.1186/1471-2164-11-713 This Article is brought to you for free and open access by the Nutrition at TRACE: Tennessee Research and Creative Exchange. It has been accepted for inclusion in Nutrition Publications and Other Works by an authorized administrator of TRACE: Tennessee Research and Creative Exchange. For more information, please contact [email protected]. Stewart et al. BMC Genomics 2010, 11:713 http://www.biomedcentral.com/1471-2164/11/713 RESEARCH ARTICLE Open Access Genetic and genomic analysis of hyperlipidemia, obesity and diabetes using (C57BL/6J × TALLYHO/JngJ) F2 mice Taryn P Stewart1, Hyoung Yon Kim2, Arnold M Saxton3, Jung Han Kim1* Abstract Background: Type 2 diabetes (T2D) is the most common form of diabetes in humans and is closely associated with dyslipidemia and obesity that magnifies the mortality and morbidity related to T2D. The genetic contribution to human T2D and related metabolic disorders is evident, and mostly follows polygenic inheritance. The TALLYHO/ JngJ (TH) mice are a polygenic model for T2D characterized by obesity, hyperinsulinemia, impaired glucose uptake and tolerance, hyperlipidemia, and hyperglycemia. -

Enzyme DHRS7
Toward the identification of a function of the “orphan” enzyme DHRS7 Inauguraldissertation zur Erlangung der Würde eines Doktors der Philosophie vorgelegt der Philosophisch-Naturwissenschaftlichen Fakultät der Universität Basel von Selene Araya, aus Lugano, Tessin Basel, 2018 Originaldokument gespeichert auf dem Dokumentenserver der Universität Basel edoc.unibas.ch Genehmigt von der Philosophisch-Naturwissenschaftlichen Fakultät auf Antrag von Prof. Dr. Alex Odermatt (Fakultätsverantwortlicher) und Prof. Dr. Michael Arand (Korreferent) Basel, den 26.6.2018 ________________________ Dekan Prof. Dr. Martin Spiess I. List of Abbreviations 3α/βAdiol 3α/β-Androstanediol (5α-Androstane-3α/β,17β-diol) 3α/βHSD 3α/β-hydroxysteroid dehydrogenase 17β-HSD 17β-Hydroxysteroid Dehydrogenase 17αOHProg 17α-Hydroxyprogesterone 20α/βOHProg 20α/β-Hydroxyprogesterone 17α,20α/βdiOHProg 20α/βdihydroxyprogesterone ADT Androgen deprivation therapy ANOVA Analysis of variance AR Androgen Receptor AKR Aldo-Keto Reductase ATCC American Type Culture Collection CAM Cell Adhesion Molecule CYP Cytochrome P450 CBR1 Carbonyl reductase 1 CRPC Castration resistant prostate cancer Ct-value Cycle threshold-value DHRS7 (B/C) Dehydrogenase/Reductase Short Chain Dehydrogenase Family Member 7 (B/C) DHEA Dehydroepiandrosterone DHP Dehydroprogesterone DHT 5α-Dihydrotestosterone DMEM Dulbecco's Modified Eagle's Medium DMSO Dimethyl Sulfoxide DTT Dithiothreitol E1 Estrone E2 Estradiol ECM Extracellular Membrane EDTA Ethylenediaminetetraacetic acid EMT Epithelial-mesenchymal transition ER Endoplasmic Reticulum ERα/β Estrogen Receptor α/β FBS Fetal Bovine Serum 3 FDR False discovery rate FGF Fibroblast growth factor HEPES 4-(2-Hydroxyethyl)-1-Piperazineethanesulfonic Acid HMDB Human Metabolome Database HPLC High Performance Liquid Chromatography HSD Hydroxysteroid Dehydrogenase IC50 Half-Maximal Inhibitory Concentration LNCaP Lymph node carcinoma of the prostate mRNA Messenger Ribonucleic Acid n.d. -

Molecule Based on Evans Blue Confers Superior Pharmacokinetics and Transforms Drugs to Theranostic Agents
Novel “Add-On” Molecule Based on Evans Blue Confers Superior Pharmacokinetics and Transforms Drugs to Theranostic Agents Haojun Chen*1,2, Orit Jacobson*2, Gang Niu2, Ido D. Weiss3, Dale O. Kiesewetter2, Yi Liu2, Ying Ma2, Hua Wu1, and Xiaoyuan Chen2 1Department of Nuclear Medicine, Xiamen Cancer Hospital of the First Affiliated Hospital of Xiamen University, Xiamen, China; 2Laboratory of Molecular Imaging and Nanomedicine, National Institute of Biomedical Imaging and Bioengineering, National Institutes of Health, Bethesda, Maryland; and 3Laboratory of Molecular Immunology, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Bethesda, Maryland One of the major design considerations for a drug is its The goal of drug development is to achieve high activity and pharmacokinetics in the blood. A drug with a short half-life in specificity for a desired biologic target. However, many potential the blood is less available at a target organ. Such a limitation pharmaceuticals that meet these criteria fail as therapeutics because dictates treatment with either high doses or more frequent doses, of unfavorable pharmacokinetics, in particular, rapid blood clearance, both of which may increase the likelihood of undesirable side effects. To address the need for additional methods to improve which prevents the achievement of therapeutic concentrations. For the blood half-life of drugs and molecular imaging agents, we some drugs, the administration of large or frequently repeated doses developed an “add-on” molecule that contains 3 groups: a trun- is required to achieve and maintain therapeutic levels (1) but can, in cated Evans blue dye molecule that binds to albumin with a low turn, increase the probability of undesired side effects. -

Pepperdine University Editorial Style Guide INTRODUCTION
Pepperdine University Editorial Style Guide INTRODUCTION Editorial Stance Pepperdine University has adopted a unified editorial style for both print and digital media, which principally follows the Chicago Manual of Style (17th edition) with certain exceptions noted in this guide. Pepperdine style is a “down” style, meaning that capitals are to be used sparingly and intentionally. References to the 17th edition (when applicable) are provided within entries where Pepperdine and Chicago coincide. Ideal Pepperdine style is minimalist yet pragmatic, intended to provide clarity, consistent logic, and elegant structure to its communications, using the least amount of punctuation and type to most effectively and quickly deliver an author’s message to the intended audience. Editorial/Aesthetic License Pepperdine style should give writers and designers a broad range of creative freedom in which to work. Deviations from standard practice in University-branded, flagship publications are permitted only by agreement with Integrated Marketing Communications. As a general rule, in all University publications using another company’s word mark and/or logo, we should make sure we have written permission to do so. All factual claims must be verifiable. Grammar and usage must follow standard current practices. Standard Reference Books Consult the 17th edition of the Chicago Manual of Style for questions of style, punctuation, and grammar not treated in this guide. Consult the 11th edition of the Merriam-Webster Collegiate Dictionary to check correct and preferred spelling, syllable division, hyphenation, and abbreviated forms. The American Heritage Dictionary, any edition, is recommended for reference on how words are popularly understood in the United States. Pepperdine-Chicago vs. -

Solutions to 7.012 Problem Set 1
MIT Biology Department 7.012: Introductory Biology - Fall 2004 Instructors: Professor Eric Lander, Professor Robert A. Weinberg, Dr. Claudette Gardel Solutions to 7.012 Problem Set 1 Question 1 Bob, a student taking 7.012, looks at a long-standing puddle outside his dorm window. Curious as to what was growing in the cloudy water, he takes a sample to his TA, Brad Student. He wanted to know whether the organisms in the sample were prokaryotic or eukaryotic. a) Give an example of a prokaryotic and a eukaryotic organism. Prokaryotic: Eukaryotic: All bacteria Yeast, fungi, any animial or plant b) Using a light microscope, how could he tell the difference between a prokaryotic organism and a eukaryotic one? The resolution of the light microscope would allow you to see if the cell had a true nucleus or organelles. A cell with a true nucleus and organelles would be eukaryotic. You could also determine size, but that may not be sufficient to establish whether a cell is prokaryotic or eukaryotic. c) What additional differences exist between prokaryotic and eukaryotic organisms? Any answer from above also fine here. In addition, prokaryotic and eukaryotic organisms differ at the DNA level. Eukaryotes have more complex genomes than prokaryotes do. Question 2 A new startup company hires you to help with their product development. Your task is to find a protein that interacts with a polysaccharide. a) You find a large protein that has a single binding site for the polysaccharide cellulose. Which amino acids might you expect to find in the binding pocket of the protein? What is the strongest type of interaction possible between these amino acids and the cellulose? Cellulose is a polymer of glucose and as such has many free hydroxyl groups. -

Biochemistry I Enzymes
BIOCHEMISTRY I 3rd. Stage Lec. ENZYMES Biomedical Importance: Enzymes, which catalyze the biochemical reactions, are essential for life. They participate in the breakdown of nutrients to supply energy and chemical building blocks; the assembly of those building blocks into proteins, DNA, membranes, cells, and tissues; and the harnessing of energy to power cell motility, neural function, and muscle contraction. The vast majority of enzymes are proteins. Notable exceptions include ribosomal RNAs and a handful of RNA molecules imbued with endonuclease or nucleotide ligase activity known collectively as ribozymes. The ability to detect and to quantify the activity of specific enzymes in blood, other tissue fluids, or cell extracts provides information that complements the physician’s ability to diagnose and predict the prognosis of many diseases. Further medical applications include changes in the quantity or in the catalytic activity of key enzymes that can result from genetic defects, nutritional deficits, tissue damage, toxins, or infection by viral or bacterial pathogens (eg, Vibrio cholerae). Medical scientists address imbalances in enzyme activity by using pharmacologic agents to inhibit specific enzymes and are investigating gene therapy as a means to remedy deficits in enzyme level or function. In addition to serving as the catalysts for all metabolic processes, their impressive catalytic activity, substrate specificity, and stereospecificity enable enzymes to fulfill key roles in additional processes related to human health and well-being. Proteases and amylases augment the capacity of detergents to remove dirt and stains, and enzymes play important roles in producing or enhancing the nutrient value of food products for both humans and animals.