Electroporation-Based Treatments in Urology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Electrochemotherapy
Service: Cancer Services Electrochemotherapy Exceptional healthcare, personally delivered What to expect from your treatment You have been told by your doctor that you need electrochemotherapy to treat the cancer that has either spread from your original cancer and /or is suitable for this treatment. This leaflet is designed to answer your questions about the treatment so that you are fully aware of what to expect. What is Electrochemotherapy? Electrochemotherapy is a treatment combining a low dose of a chemotherapy drug (Bleomycin) and an electrical pulse (electroporation) applied directly to the cancer cells using an electrode. This low level dose of chemotherapy drug is not normally effective against the cancer, as it is difficult to get inside the cells. When the electric pulse is applied, the cells form pores allowing the drug to enter and be active against the cancer. What happens to the normal cells? As the chemotherapy drug is most active against the cancer cells, the normal tissue is unaffected. 2 Electrochemotherapy What type of cancer can be treated? Electrochemotherapy is used to treat cancers that have spread to the skin or just below the skin’s surface (metastasised) from the following types of cancer: n All skin cancer (melanoma & non-melanoma) n Breast cancer recurrence n Head and neck cancer, including oral cancer Electrochemotherapy has the advantage of preserving healthy tissue when compared to other treatment options. It can also be used to shrink large cancers making them easier to remove surgically. What happens during the treatment? The chemotherapy drug is usually given into a vein and after a short time a probe is inserted into the cancer, which releases a small electrical current. -

Scientific Programme for All
Optimal radiotherapy Scientific Programme for all ESTRO ANNUAL CONFE RENCE 27 - 31 August 2021 Onsite in Madrid, Spain & Online Saturday 28 August 2021 Track: Radiobiology Teaching lecture: The microbiome: Its role in cancer development and treatment response Saturday, 28 August 2021 08:00 - 08:40 N104 Chair: Marc Vooijs - 08:00 The microbiome: Its role in cancer development and treatment response SP - 0004 A. Facciabene (USA) Track: Clinical Teaching lecture: Breast reconstruction and radiotherapy Saturday, 28 August 2021 08:00 - 08:40 Plenary Chair: Philip Poortmans - 08:00 Breast reconstruction and radiotherapy SP - 0005 O. Kaidar-Person (Israel) Track: Clinical Teaching lecture: Neurocognitive changes following radiotherapy for primary brain tumours Saturday, 28 August 2021 08:00 - 08:40 Room 1 Chair: Brigitta G. Baumert - 08:00 Evaluation and care of neurocognitive effects after radiotherapy SP - 0006 M. Klein (The Netherlands) 08:20 Imaging biomarkers of dose-induced damage to critical memory regions SP - 0007 A. Laprie (France Track: Physics Teaching lecture: Independent dose calculation and pre-treatment patient specific QA Saturday, 28 August 2021 08:00 - 08:40 Room 2.1 Chair: Kari Tanderup - 08:00 Independent dose calculation and pre-treatment patient specific QA SP - 0008 P. Carrasco de Fez (Spain) 1 Track: Physics Teaching lecture: Diffusion MRI: How to get started Saturday, 28 August 2021 08:00 - 08:40 Room 2.2 Chair: Tufve Nyholm - Chair: Jan Lagendijk - 08:00 Diffusion MRI: How to get started SP - 0009 R. Tijssen (The Netherlands) Track: RTT Teaching lecture: The role of RTT leadership in advancing multi-disciplinary research Saturday, 28 August 2021 08:00 - 08:40 N103 Chair: Sophie Perryck - 08:00 The role of RTT leadership in advancing multi-disciplinary research SP - 0010 M. -

Boosting the Immune Response with the Combination of Electrochemotherapy and Immunotherapy: a New Weapon for Squamous Cell Carcinoma of the Head and Neck?
cancers Communication Boosting the Immune Response with the Combination of Electrochemotherapy and Immunotherapy: A New Weapon for Squamous Cell Carcinoma of the Head and Neck? Francesco Longo 1 , Francesco Perri 2,* , Francesco Caponigro 2, Giuseppina Della Vittoria Scarpati 3, Agostino Guida 4 , Ettore Pavone 4, Corrado Aversa 4, Paolo Muto 5, Mario Giuliano 6, Franco Ionna 4 and Raffaele Solla 7 1 Department of Otolaryngology Surgery and Oncology, Ospedale Casa Sollievo della Sofferenza, 71013 San Giovanni Rotondo, Italy; [email protected] 2 Head and Neck Medical Oncology Unit, INT IRCCS Fondazione G. Pascale, 80131 Naples, Italy; [email protected] 3 Medical Oncology Unit, Hospital of Pollena Trocchia, ASLNA3 sud, 80040 Naples, Italy; [email protected] 4 Department of Otolaryngology Surgery and Oncology, INT IRCCS Fondazione G. Pascale, 80131 Naples, Italy; [email protected] (A.G.); [email protected] (E.P.); [email protected] (C.A.); [email protected] (F.I.) 5 Department of Radiation Oncology, INT IRCCS Fondazione G. Pascale, 80131 Naples, Italy; [email protected] 6 Department of Experimental and Clinical Oncology, University of Naples “Federico II”, 80131 Naples, Italy; [email protected] 7 Italian National Research Council, Institute of Biostructure & Bioimaging, 80131 Naples, Italy; raff[email protected] * Correspondence: [email protected]; Tel.: +0039-0815903362 Received: 19 August 2020; Accepted: 23 September 2020; Published: 28 September 2020 Simple Summary: Squamous cell carcinoma of the head and neck (SCCHN) represents a problem of utmost concern and, for many clinicians and surgeons, an enormous challenge. -

World Resources Institute the Monsanto Company
World Resources Institute Sustainable Enterprise Program A program of the World Resources Institute The Monsanto Company: Quest for Sustainability (A) “Biotechnology represents a potentially sustainable For more than a decade, WRI's solution to the issue, not only of feeding people, but of providing Sustainable Enterprise Program (SEP) the economic growth that people are going to need to escape has harnessed the power of business to poverty…… [Biotechnology] poses the possibility of create profitable solutions to leapfrogging the industrial revolution and moving to a post- environment and development industrial society that is not only economically attractive, but challenges. BELL, a project of SEP, is also environmentally sustainable.i ” focused on working with managers and academics to make companies --Robert Shapiro, CEO, Monsanto Company more competitive by approaching social and environmental challenges as unmet market needs that provide Upon his promotion to CEO of chemical giant The business growth opportunities through Monsanto Company in 1995, Robert Shapiro became a vocal entrepreneurship, innovation, and champion of sustainable development and sought to redefine the organizational change. firm’s business strategy along principles of sustainability. Shapiro’s rhetoric was compelling. He captured analysts’ Permission to reprint this case is attention with the specter of mass hunger and environmental available at the BELL case store. degradation precipitated by rapid population growth and the Additional information on the Case -

Quick and Efficient Method for Genetic Transformation of Biopolymer
Technical Note Received: 29 July 2009 Revised: 14 September 2009 Accepted: 14 September 2009 Published online in Wiley Interscience: 29 October 2009 (www.interscience.wiley.com) DOI 10.1002/jctb.2284 Quick and efficient method for genetic transformation of biopolymer-producing bacteria Qin Wang,a Alexander P. Mueller,a Chean Ring Leong,b Ken’ichiro Matsumoto,b Seiichi Taguchib and Christopher T. Nomuraa∗ Abstract In order to genetically modify microorganisms capable of producing polyhydroxyalkanoate (PHA) biopolymers, a simple and rapid method to prepare freshly plated Pseudomonas cells for transformation via electroporation was developed. This method can be used to transfer both replicative plasmids and linear DNA to knock out genes into the cells. The transformation efficiencies were in the range of ≥107 transformants µg−1 DNA for replicative plasmids and ≥106 transformants µg−1 DNA for linear DNA, which are comparable with commercially available competent cells. Furthermore, this transformation procedure can be performed in less than 10 min, saving a great deal of time compared with traditional methods. Knockout mutants of several Pseudomonas species were generated by transformation of linear DNA and these mutations were verified by PCR and analysis of PHA content. c 2009 Society of Chemical Industry Keywords: transformation; electroporation; Pseudomonas putida; polyhydroxyalkanoates (PHAs) INTRODUCTION using various strains of P. putida.StrainsweregrowninLuria- Pseudomonas putida is a Gram-negative soil bacterium that plays Bertani (LB) medium (1% tryptone, 0.5% yeast extract, and 0.5% animportantroleinelementcycling innature,bioremediation,and NaCl) with the appropriate antibiotic when necessary. For selection production of polyhydroxyalkanoates (PHAs), which are environ- of transformants, kanamycin (Km) and gentamycin (Gm) were mentally friendly biodegradable plastics.1–3 Despite having a fully added to LB agar plates and liquid media at final concentrations sequenced genome,3 the functions of many ORFs in this organ- of 50 µgmL−1 and 20 µgmL−1, respectively. -
ES Cell Targeting Handbook
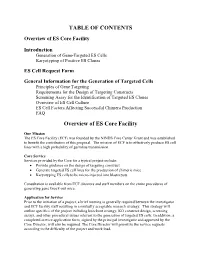
TABLE OF CONTENTS Overview of ES Core Facility Introduction Generation of Gene-Targeted ES Cells Karyotyping of Positive ES Clones ES Cell Request Form General Information for the Generation of Targeted Cells Principles of Gene Targeting Requirements for the Design of Targeting Constructs Screening Assay for the Identification of Targeted ES Clones Overview of ES Cell Culture ES Cell Factors Affecting Successful Chimera Production FAQ Overview of ES Core Facility Our Mission The ES Core Facility (ECF) was founded by the NINDS Core Center Grant and was established to benefit the contributors of this proposal. The mission of ECF is to effectively produce ES cell lines with a high probability of germline transmission. Core Service Services provided by the Core for a typical project include: • Provide guidance on the design of targeting construct • Generate targeted ES cell lines for the production of chimeric mice • Karyotyping ES cells to be micro-injected into blastocysts Consultation is available from ECF directors and staff members on the entire procedures of generating gene knock-out mice. Application for Service Prior to the initiation of a project, a brief meeting is generally required between the investigator and ECF facility staff resulting in a mutually acceptable research strategy. This strategy will outline specifics of the project including knockout strategy, KO construct design, screening assays, and other procedural issues relevant to the generation of targeted ES cells. In addition, a completed service application form, signed by the principal investigator and approved by the Core Director, will also be required. The Core Director will prioritize the service requests according to the difficulty of the project and work load. -

Intramuscular Electroporation Delivery of IFN- Gene Therapy for Inhibition of Tumor Growth Located at a Distant Site
Gene Therapy (2001) 8, 400–407 2001 Nature Publishing Group All rights reserved 0969-7128/01 $15.00 www.nature.com/gt RESEARCH ARTICLE Intramuscular electroporation delivery of IFN-␣ gene therapy for inhibition of tumor growth located at a distant site S Li, X Zhang, X Xia, L Zhou, R Breau, J Suen and E Hanna Department of Otolaryngology/Head and Neck Surgery, University of Arkansas School of Medicine, 4001 W Capital Avenue, Little Rock, AR 72205, USA Although electroporation has been shown in recent years to 2 or endostatin gene, also delivered by electro-injection. The be a powerful method for delivering genes to muscle, no increased therapeutic efficacy was associated with a high gene therapy via electro-injection has been studied for the level and extended duration of IFN-␣ expression in muscle treatment of tumors. In an immunocompetent tumor-bearing and serum. We also discovered that the high level of IFN-␣ murine model, we have found that delivery of a low dose of expression correlated with increased expression levels of reporter gene DNA (10 g) to muscle via electroporation the antiangiogenic genes IP-10 and Mig in local tumor under specific pulse conditions (two 25-ms pulses of 375 tissue, which may have led to the reduction of blood vessels V/cm) increased the level of gene expression by two logs of observed at the local tumor site. Delivery of increasing doses magnitude. Moreover, administration of 10 g of interferon (10–100 g) of IFN-␣ plasmid DNA by injection alone did (IFN)-␣ DNA plasmid using these parameters once a week not increase antitumor activity, whereas electroporation for 3 weeks increased the survival time and reduced squam- delivery of increasing doses (10–40 g) of IFN-␣ plasmid ous cell carcinoma (SCC) growth at a distant site in the DNA did increase the survival time. -

Wake Forest Comprehensive Cancer Center Annual Report 2014
2014 CANCER PROGRAM ANNUAL REPORT WITH 2013 STATISTICS TABLE OF CONTENTS 1 MESSAGE FROM THE DIRECTOR 2 CANCER REGISTRY 4 CANCER COMMITTEE MEMBERS/ CANCER REGISTRY STAFF 5 CANCER ACTIVITIES 23 CANCER DATA 29 PUBLISHED ABSTRACTS Giant Cell Carcinoma Courtesy of Dr. A. Julian Garvin, Department of Pathology 2014 1 CANCER PROGRAM ANNUAL REPORT ANNUAL PROGRAM CANCER Comprehensive Cancer Center AT WAKE FOREST BAPTIST MEDICAL CENTER “ We are extremely proud of the achievements of our Comprehensive Cancer Center as we strive to deliver the best care possible to our patients, their families and caregivers.” – Boris Pasche, MD, PhD, FACP Director, Comprehensive Cancer Center The Comprehensive Cancer Center The Cancer Center recognizes the existing floors, which house all at Wake Forest Baptist Medical the importance of building cross- outpatient oncology services as well Center was founded in the early departmental and transdisciplinary clinical trial staff. This new building 1960s and became a National Cancer team approaches to advance the provides an exceptional environment Institute-designated cancer center science and treatment of cancer. for patients, family and caregiver in 1974, shortly after the National Teams have been developed in cancer experience. Cutting-edge research Cancer Act was placed into law. genomics, tumor microenvironment, and precision medicine is available The Cancer Center received an NCI nanotechnology, imaging, novel to all patients, who have access to “comprehensive” designation in 1990. anticancer drugs, novel anticancer approximately 200 clinical trials. It is one of the longest-standing NCI devices, cancer survivorship, tobacco The Cancer Center was founded with centers, and we are proud to be a part control and cancer health disparities. -

In Vitro and Numerical Support for Combinatorial Irreversible Electroporation and Electrochemotherapy Glioma Treatment
Annals of Biomedical Engineering (Ó 2013) DOI: 10.1007/s10439-013-0923-2 In Vitro and Numerical Support for Combinatorial Irreversible Electroporation and Electrochemotherapy Glioma Treatment 1,2 3 3 4 1 R. E. NEAL II, J. H. ROSSMEISL JR., V. D’ALFONSO, J. L. ROBERTSON, P. A. GARCIA, 5 1 S. ELANKUMARAN, and R. V. DAVALOS 1Bioelectromechanical Systems Lab, Virginia Tech – Wake Forest School of Biomedical Engineering and Sciences, Blacksburg, VA, USA; 2Radiology Research Unit, The Alfred Hospital, 55 Commercial Road, Melbourne, VIC 3004, Australia; 3Neurology/ Neurosurgery Service and Center for Comparative Oncology, VA-MD Regional College of Veterinary Medicine, Blacksburg, VA, USA; 4Cancer Engineering Group, Virginia Tech – Wake Forest School of Biomedical Engineering and Sciences, Blacksburg, VA, USA; and 5Department of Biomedical Sciences and Pathobiology, VA-MD Regional College of Veterinary Medicine, Blacksburg, VA, USA (Received 12 April 2013; accepted 4 October 2013) Associate Editor Agata A. Exner oversaw the review of this article. Abstract—Irreversible electroporation (IRE) achieves tar- ABBREVIATIONS geted volume non-thermal focal ablation using a series of brief electric pulses to kill cells by disrupting membrane IRE Irreversible electroporation integrity. Electrochemotherapy (ECT) uses lower numbers of ECT Electrochemotherapy sub-lethal electric pulses to disrupt membranes for improved BBB Blood–brain-barrier drug uptake. Malignant glioma (MG) brain tumors are difficult to treat due to diffuse peripheral margins into healthy neural tissue. Here, in vitro experimental data and numerical simulations investigate the feasibility for IRE- INTRODUCTION relevant pulse protocols with adjuvant ECT drugs to enhance MG treatment. Cytotoxicity curves were produced on two Therapeutic options for brain and central nervous glioma cell lines in vitro at multiple pulse strengths and drug system malignancies include radiation therapy, surgical doses with Bleomycin or Carboplatin. -

Electrochemotherapy Compared to Surgery for Treatment of Canine Mast Cell Tumours
in vivo 23: 55-62 (2009) Electrochemotherapy Compared to Surgery for Treatment of Canine Mast Cell Tumours VERONIKA KODRE1, MAJA CEMAZAR2, JANI PECAR3, GREGOR SERSA2, ANDREJ CŐR4 and NATASA TOZON3 1Janssen-Cilag, Division of Johnson-Johnson, Ljubljana; 2Institute of Oncology Ljubljana, Ljubljana; 3University of Ljubljana, Veterinary Faculty, Clinic for Small Animal Medicine and Surgery, Ljubljana; 4University of Ljubljana, Medical Faculty, Ljubljana, Slovenia Abstract. The aim of this study was to evaluate the behaviour, making these tumours challenging to diagnose effectiveness of local treatment electrochemotherapy (ECT) with and to treat. MCTs predominantly occur in middle-aged dogs cisplatin and to compare it with effectiveness of surgery for of many breeds, but more frequently in Boxers, Staffordshire treatment of mast cell tumours (MCT) in dogs. Materials and Bull Terriers, Labradors, Golden Retrievers, Weimeraner and Methods: In the present retrospective study, 25 dogs of different Schnauzers, with no gender predisposition (1). Several breeds with MCT were divided into two treatment groups: factors have been evaluated as prognostic factors, including surgery (16 dogs with 16 tumours) and those whose owners histological grade, which is the most accurate predictor of refused surgery being included into the ECT group (9 dogs with behaviour, as well as clinical stage, size, growth rate, breed, 12 tumours). Response rate and duration of response to the completeness of surgical excision, presence of systemic treatment were evaluated and comparison between groups was signs, argyrophilic nuclear organizer region count, DNA made. Results: The clinical stages of the tumours were stage I in ploidy, matrix metalloproteinases, microvessel density and 4 (45% ) and stage III in 5 (55% ) dogs treated by ECT; 12 abnormal expression of the p53 tumour suppressor gene. -

Engineering of Primary Human B Cells with CRISPR/Cas9 Targeted Nuclease Received: 26 January 2018 Matthew J
www.nature.com/scientificreports OPEN Engineering of Primary Human B cells with CRISPR/Cas9 Targeted Nuclease Received: 26 January 2018 Matthew J. Johnson1,2,3, Kanut Laoharawee1,2,3, Walker S. Lahr1,2,3, Beau R. Webber1,2,3 & Accepted: 23 July 2018 Branden S. Moriarity1,2,3 Published: xx xx xxxx B cells ofer unique opportunities for gene therapy because of their ability to secrete large amounts of protein in the form of antibody and persist for the life of the organism as plasma cells. Here, we report optimized CRISPR/Cas9 based genome engineering of primary human B cells. Our procedure involves enrichment of CD19+ B cells from PBMCs followed by activation, expansion, and electroporation of CRISPR/Cas9 reagents. We are able expand total B cells in culture 10-fold and outgrow the IgD+ IgM+ CD27− naïve subset from 35% to over 80% of the culture. B cells are receptive to nucleic acid delivery via electroporation 3 days after stimulation, peaking at Day 7 post stimulation. We tested chemically modifed sgRNAs and Alt-R gRNAs targeting CD19 with Cas9 mRNA or Cas9 protein. Using this system, we achieved genetic and protein knockout of CD19 at rates over 70%. Finally, we tested sgRNAs targeting the AAVS1 safe harbor site using Cas9 protein in combination with AAV6 to deliver donor template encoding a splice acceptor-EGFP cassette, which yielded site-specifc integration frequencies up to 25%. The development of methods for genetically engineered B cells opens the door to a myriad of applications in basic research, antibody production, and cellular therapeutics. -

Cutting Eugenics out of CRISPR-Cas9
Ethics in Biology, Engineering & Medicine - An International Journal, 6(3–4): 263–279 (2015) Cutting Eugenics Out of CRISPR-Cas9 Carolyn Brokowski,a,* Marya Pollack,b & Robert Pollackc aBioethics (Medical Ethics) Department, Columbia University School of Professional Studies, New York, New York; bDepartment of Psychiatry, Columbia University College of Physicians and Surgeons, Inwood Clinic, New York, New York; cBiological Sciences Department, Columbia University School of the Arts, New York, New York *Address all correspondence to: Carolyn Brokowski, M.S. Candidate; Bioethics (Medical Ethics) Department, Columbia University School of Professional Studies, 203 Lewisohn Hall, 2970 Broadway, MC 4119, New York, NY 10027; E-mail: [email protected] ABSTRACT: The use of clustered regularly interspaced short palindromic repeats (CRISPR) and their associated (Cas) proteins (the CRISPR-Cas system) in genomic engineering is among the most promising biomedical innovations to occur in the last few decades. One of this system’s most profound features is its ability to edit genomes with impressive specificity, which may cause significant alterations of cellular, tissue, and organismal phenotypes at the near instance of the editing, over the lifespan of the organism and potentially into any number of future genera- tions. We argue that the use of the CRISPR-Cas9 system to edit the human germline should be legally prohibited on account of the system’s potential for generating an unjust eugenic future. Its use in nongermline experimentation and applications, however, should not be constrained on eugenic grounds. Such a blanket legal prohibition might limit the progress gleaned from this technology. Allowing experimentation in human subjects more broadly might expose par- ticipants to considerable risk and potentially harmful outcomes, and the system might prove unable to realize tangible therapeutic outcomes that seem likely ex ante.