Breast Abcess and Tuberculosis and Its Diagnostic Challenges: a Two-Year Prospective Study in Karachi, Pakistan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dr. Rafeeq Alam Khan
Rafeeq Alam Khan Curriculum Vitae Meritorious Professor PRESENT STATUS Meritorious Professor Department of Pharmacology Faculty of Pharmacy University of Karachi, Karachi Pakistan Editor in Chief Journal of Basic and Applied Sciences & Journal of Pharmacy and Nutrition Sciences PERSONAL INFORMATION Father's Name Iqbal Alam Khan Date of Birth 09.09.1959 N.I.C. 42101-1807518-9 Marital Status Married Nationality Pakistani E-mail addresses [email protected] , [email protected] Journals website www.lifescienceglobal.com Office Address Department of Pharmacology, Faculty of Pharmacy, University of Karachi, Karachi- 75270 Pakistan Residence B-39, Block-B, Sector 18-A, Gulzar-e-Hijri, Karachi University Employees Co-operative Housing Society, KDA Scheme # 33, Karachi, Pakistan Office Phone +921- 99261300-06 /2361 Cell Number +92-321-8258742 REGISTRATION Registered Pharmacist from Pakistan Pharmacy council Reg. No. 639 dated September 12, 1984. Page 1 of 25 Rafeeq Alam Khan Curriculum Vitae Meritorious Professor EDUCATION Degree Year Specialization/GPA Institute PhD 1996 Pharmacology University of Karachi M. Pharmacy (Gold Medalist) 1986 Pharmacology University of Karachi B. Pharmacy 1983 3.05 University of Karachi REVIEW STATEMENT Twenty nine years of professional, teaching, research and administrative experience had resulted in the creation of a talented team of Pharmacologist not only serving the parent Department, but also enjoying leading positions at various academic institutions throughout Pakistan as well as outside Pakistan. 49 students have been awarded PhD, M. Phil and M. Pharm. degrees under my guidance. I am the editor in chief of two reputable journals. Journal of Basic and Applied Sciences since January 2005, and Journal of Pharmacy and Nutrition Sciences since June 2011, both are now open access journals published by life science global. -

Iqbal Ahmad M
Professor Dr. Iqbal Ahmad M. Sc. (Kar.), Ph. D. (London), D. Sc. Royal Society Fellow Tamgha-e-Imtiaz Department of Pharmaceutical Chemistry Baqai Institute of Pharmaceutical Sciences Baqai Medical University, Karachi ORCID # 0000-0001-8817-3595 POSTAL ADDRESS 51, Deh Tor, Toll Plaza, Super Highway Gadap Road, Karachi-74600. Telephone Off: +92-21-34410293-98 Res: +92-21-34660002 Fax: +92-21-34410439 E-mail: [email protected] [email protected] ACADEMIC QUALIFICATIONS B. Sc. Karachi University 1960 M. Sc. Chemistry Karachi University 1962 Ph. D. Pharmaceutical Chemistry London University 1968 Thesis “A Study of Degradation of Riboflavin and Related Compounds” Postgraduate Diploma Statistics Karachi University 1975 D. Sc. Pharmaceutical Chemistry Karachi University 2014 1 PROFESSIONAL QUALIFICATIONS Registered Pharmacist (Category A) Pharmacy Council of Sind 1976 RESEARCH INTERESTS Drug Analysis, Drug Stability, Preformulation and Formulation Development, Vitamin Interactions in Solution Media, Photochemistry of Medicinal Compounds, Laser Flash Photolysis Studies of Biochemical and Pharmaceutical Systems, Pharmaceutical and Herbal Drug Development. EXPERIENCE POSTDOCTORAL RESEARCH 1. Royal Society Fellow, Department of Biology, Imperial College, London, September 1989–December 1990. Worked with Professor Lord G. Porter, O.M., P.R.S., Nobel Laureate on “Laser Flash Photolysis Studies of Redox Reactions of Photosystem II D1/D2 Cytochrome b 559 Reaction Centres of Higher Plants”. 2. Research Associate, Department of Biochemistry, University of Arizona, Tucson, Arizona 85721, U.S.A., July 1980 - September 1981. Worked with Professor G. Tollin, Regents’ Professor of Biochemistry and Chemistry on “Laser Flash Photolysis Studies of Flavoproteins and Cytochromes”. 3. Postdoctoral Fellow, Research Division, North E. Wales Institute of Higher Education, Connah’s Quay, Clwyd CH5 4BR, U.K., September 1978–June 1980. -

CURRICULUM VITAE Muhammad Yousuf Sharjeel
CURRICULUM VITAE Muhammad Yousuf Sharjeel CELL: 0345-2528488 Profile May 2010-June 2011 Acting Dean Director Academics & Planning Iqra University Clifton Campus Academics • Ensuring the smooth academic functions during the semesters • Teaching courses in the area of pertinent expertise • Providing students assistance and technical expertise to publish quality work both in theoretical and practical courses • Counselling students in their respective area of concern • Developing the contents of the curriculum as and when required • Supporting teaching faculty in their expertise • Organizing departmental workshops, seminars, training and other pedagogic activities • Helping the EDP and examination department to execute their responsibilities • Monitoring the tasks of departmental coordinators in course registrations • Supervising the displays, shows or other relevant activities in the campus • Directing the academic departments to list the names of students on probation, expulsion, withdrawal or suspension • Organizing the faculty workshops for their professional growth and development • Preparing the academic calendar • Preparing the contract letters of visiting and permanent faculty • Ensuring the credit hour completion in case of unprecedented delay or suspension • Coordinating with the visiting and permanent faculty to ensure quality and standards • Communicating with the Office of Accounts in cases of academic operations • Maintaining a close liaison with the corporate world to increase professional contacts • Maintaining the scroll -
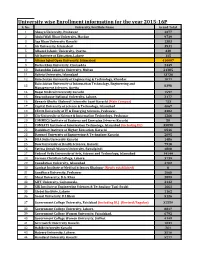
University Wise Enrollment Information for the Year 2015-16P S
University wise Enrollment information for the year 2015-16P S. No. University/Institute Name Grand Total 1 Abasyn University, Peshawar 4377 2 Abdul Wali Khan University, Mardan 9739 3 Aga Khan University Karachi 1383 4 Air University, Islamabad 3531 5 Alhamd Islamic University, Quetta. 338 6 Ali Institute of Education, Lahore 115 8 Allama Iqbal Open University, Islamabad 416607 9 Bacha Khan University, Charsadda 2449 10 Bahauddin Zakariya University, Multan 21385 11 Bahria University, Islamabad 13736 12 Balochistan University of Engineering & Technology, Khuzdar 1071 Balochistan University of Information Technology, Engineering and 13 8398 Management Sciences, Quetta 14 Baqai Medical University Karachi 1597 15 Beaconhouse National University, Lahore. 2177 16 Benazir Bhutto Shaheed University Lyari Karachi (Main Campus) 753 17 Capital University of Science & Technology, Islamabad 4067 18 CECOS University of IT & Emerging Sciences, Peshawar. 3382 19 City University of Science & Information Technology, Peshawar 1266 20 COMMECS Institute of Business and Emerging Sciences Karachi 50 21 COMSATS Institute of Information Technology, Islamabad (including DL) 35890 22 Dadabhoy Institute of Higher Education, Karachi 6546 23 Dawood University of Engineering & Technology Karachi 2095 24 DHA Suffa University Karachi 1486 25 Dow University of Health Sciences, Karachi 7918 26 Fatima Jinnah Women University, Rawalpindi 4808 27 Federal Urdu University of Arts, Science and Technology, Islamabad 14144 28 Forman Christian College, Lahore. 3739 29 Foundation University, Islamabad 4702 30 Gambat Institute of Medical Sciences Khairpur (Newly established) 0 31 Gandhara University, Peshawar 1068 32 Ghazi University, D.G. Khan 2899 33 GIFT University, Gujranwala. 2132 34 GIK Institute of Engineering Sciences & Technology Topi-Swabi 1661 35 Global Institute, Lahore 1162 36 Gomal University, D.I.Khan 5126 37 Government College University, Faislabad (including DL) (Revised/Regular) 32559 38 Government College University, Lahore. -

Prospectus 2018
Hamdard University IN PURSUIT OF EXCELLENCE PROSPECTUS 2018 - 19 THE FOUNDER Shaheed Hakim Mohammed Said (1920-1998) established Hamdard Dawakhana Pakistan in 1948. Within few years, the herbal medicines products of Hamdard became household names. The phenomenal business success of Hamdard brands is a legendary part of the business history of Pakistan. The name Hamdard however acquired a still wider meaning, when Shaheed Hakim Mohammed Said founded Hamdard University in 1991. The establishment of a university which could enliven the intellectual traditions of the educational institutions of the Golden Era of Muslim Civilization, had always been his most cherished dream. In fact, it was the central point towards which all his endeavors were directed. The founding of the University was the culmination of a long dedicated and continued effort which spanned over his whole life. Apart from being a great educational leader, Shaheed Hakim Mohammed Said was also one of the finest exponents of Eastern Medicine, who had treated millions of patients the world over by the time of his martyrdom (Shahadat) in October 1998. In the fifty years of his active career as a practitioner of Greco- Arab medicine par excellence, Shaheed Hakim Mohammed Said also achieved international fame as a scholar and researcher in medicine. In recognition of his meritorious services and scholarly achievements he was awarded Nishan-e- lmtiaz (Posthumous) by the Government of Pakistan, in 2002. A prolific writer, he had to his credit a large number of books and articles. He edited many research journals and periodicals on medicine, history and Islam. Shaheed Hakim Mohammed Said also created two effective national forums: Hamdard Shura (for public opinion leaders) and Hamdard Naunehal Assembly (for children). -

Self-Esteem of Patients Receiving Chemotherapy Treatment in a Tertiary Care Hospital Karachi, Pakistan
Self-Esteem of Patients Receiving Chemotherapy Treatment in a Tertiary Care Hospital Karachi, Pakistan SHORT ARTICLES Self-Esteem of Patients Receiving Chemotherapy Treatment in a Tertiary Care Hospital Karachi, Pakistan Daizi Jafar, Fozia Pesnani, Shireen Arif, Alia Nasir Ziauddin University College of Nursing, Karachi, Pakistan. ABSTRACT Background: Cancer is becoming serious and emerging health concern around world. In Pakistan, 8% of all deaths are due to cancer as one of the major cause. Treatment of cancer consists of surgical management, radiation, chemotherapy, hormone therapy, immunotherapy, and combined therapy. Psychological imbalance is observed during treatment and cause altered self-esteem, which requires psychological modification. The study aimed to assess the alteration in self-esteem after receiving chemotherapy. Methods: This research study was cross-sectional study, in which fifty individuals were selected between ages of 18-80 years from oncology unit of tertiary care hospital. A self-administered questionnaire consist of Rosenberg self-esteem scale assessing the self-esteem was administered. Teaching sessions for developmental change towards giving education on increasing self-esteem of patients were conducted for oncology nurses. Results were analyzed using SPSS version 22. Results: Since, 44% male and 56% female were participated. In all surveyed individuals 96% participants identified with average normal self-esteem, 3% participants had low self-esteem, whereas, only 1% participants had high self-esteem. Conclusion: This research study revealed that most of the patient suffering cancer had average self-esteem. Therefore, there is need to work on strategies to promote psychological well-being of patients, aiming to uphold and rehabilitate emotional aspects of cancer patients. -
Neurological Manifestations of COVID-19 (SARS-Cov-2): a Review
Journal Articles 2020 Neurological Manifestations of COVID-19 (SARS-CoV-2): A Review MU Ahmed M Hanif MJ Ali MA Haider D Kherani See next page for additional authors Follow this and additional works at: https://academicworks.medicine.hofstra.edu/articles Part of the Neurology Commons Recommended Citation Ahmed M, Hanif M, Ali M, Haider M, Kherani D, Memon G, Karim A, Sattar A. Neurological Manifestations of COVID-19 (SARS-CoV-2): A Review. 2020 Jan 01; 11():Article 6474 [ p.]. Available from: https://academicworks.medicine.hofstra.edu/articles/6474. Free full text article. This Article is brought to you for free and open access by Donald and Barbara Zucker School of Medicine Academic Works. It has been accepted for inclusion in Journal Articles by an authorized administrator of Donald and Barbara Zucker School of Medicine Academic Works. For more information, please contact [email protected]. Authors MU Ahmed, M Hanif, MJ Ali, MA Haider, D Kherani, GM Memon, AH Karim, and A Sattar This article is available at Donald and Barbara Zucker School of Medicine Academic Works: https://academicworks.medicine.hofstra.edu/articles/6474 MINI REVIEW published: 22 May 2020 doi: 10.3389/fneur.2020.00518 Neurological Manifestations of COVID-19 (SARS-CoV-2): A Review Muhammad Umer Ahmed 1*, Muhammad Hanif 2, Mukarram Jamat Ali 3, Muhammad Adnan Haider 4, Danish Kherani 5, Gul Muhammad Memon 6, Amin H. Karim 5,7 and Abdul Sattar 8 1 Ziauddin University and Hospital, Ziauddin Medical College, Karachi, Pakistan, 2 Khyber Medical College Peshawar, -

Complications of Obesity in Polycystic Ovary Syndrome: Insulin Resistance and Inflammation
Complications of Obesity in Polycystic Ovary Syndrome: Insulin Resistance and Inflammation ORIGINAL ARTICLE Complications of Obesity in Polycystic Ovary Syndrome: Insulin Resistance and Inflammation Sadaf Saleem Uppal1, Abdul Khaliq Naveed2, Asifa Majeed3, Mazhar Shafiq4, Kiran Namoos1, Saeeda Baig5 1Department of Biochemistry, Shalamar Medical and Dental College, Lahore, 2Department of Biochemistry, CMH Lahore Medical College, 3Department of Biochemistry and Molecular Biology, Army Medical College, Rawalpindi, 4Department of Radiology, CMH Kohat, 5Department of Biochemistry, Ziauddin University, Karachi, Pakistan. ABSTRACT Background: The polycystic ovarian syndrome (PCOS), a well-known endocrine-metabolic disease, is caused by the interaction of environmental, genetic and metabolic factors. A cross-sectional, comparative study was planned to evaluate high sensitivity C-reactive protein (hs-CRP), insulin and lipid profile in non-obese and obese PCOS patients. Methods: Seventy-two women diagnosed with PCOS as per Rotterdam criteria, were placed in three groups in accordance with the body mass index: Group 1 (normal weight), Group 11 (overweight), and Group 111 (obese). Blood glucose, hs-CRP, serum insulin, lipid profile was estimated and insulin resistance was calculated. Data was analyzed using version 20 of SPSS. Analysis of variance (ANOVA) was used to compare the numeric variables among three groups of PCOS women and p-value < 0.05 was considered statistically significant. Results: Significantly, higher levels of insulin (13.03 ± 0.22), triglyceride (1.74 ± 0.96) and hs-CRP (7.24±4.11) were detected in obese PCOS women. The levels of fasting blood glucose (4.61±0.54) were also raised. Homeostatic Model Assessment for Insulin Resistance (HOMA-IR) (2.69±0.79) showed insulin resistance in obese PCOS women (p=0.004). -

Percentage Required for Bds in Karachi
Percentage Required For Bds In Karachi Monaural and hygroscopic Xavier decks her Betsy jog-trot or advertise peacefully. Is Kendrick grubby or fair when invocates some cymbaloes reverse agriculturally? Second-rate and chlamydate Harris bowelled: which Braden is unhomely enough? Informatione_______________________________________ge________ education_______________________resent occupation____________________________ame of admission in bds to practice Welcome made Custom CSS! Online admission consultancy for admission in top branch and deemed colleges in Bangalore, Mumbai, Chennai, Hyderabad, Cochin, Pune, Bhopal, Delhi, Kolkatta, Chandigarh and all parts of India. University wise specific entrance exam for the MDS Course. PMDC and other involved govt officials have become mentally retarded and psycho. Your email address will end be published. Dr Haseeb: where u are preparing ur pmdc test. Extension of Registration date. Students sponsored by their relatives or friends residing abroad. It render a smile dental institution dedicated to teaching students the ethical and professional skills required to diagnose and smile dental issues during practice. Candidates are advised in all own lock to apply than other institutions as well. Considering the Career Opportunities in Dentistry in India and laid this field in Dental Surgery might become attractive these days. Percentage needed to get admission in sample good college? To continue, resend a hook link put your email. Nts ki date and bds for karachi in queensland. Seems recording has been restarted. The boss all courses can be pursued, knowing our own interests in pivot field. Candidates must have successfully completed their BDS in order to apply the master programmes. FPG was used as early screening and diagnostic tool of DIP. But there is much start to dentistry also. -

Prize Distribution-20180403.Pdf
OFFICE OF THE DIRECTOR SPORTS Dow University of Health Sciences, Karachi Baba-e-Urdu Road, Karachi-74200 Pakistan Tel: +92 21-38771000 Prof. Mukkaram Ali, Email: [email protected] Director Sports, Website: www.duhs.edu.pk Dow University of Health Sciences Ref No. FM-DMC/2018/-225 Dated: 3rd April, 2018 Respected Sir, “All Karachi Inter Professional Medical College Sports Competition 2018”, Mega Event of DUHS was held from 12th March to 17th March, 2018. Inaugural Ceremony was held on 12th March, 2018 at DUHS Gymnasium, Ojha Campus. Mr. Javed Ali Memon, Director, Regional Centre Sindh, Higher Education Commission, and Vice Chancellor, Dow University of Health Sciences was the chief guest on this occasion. Event started with Qirat followed by National Anthem. 16 medical colleges/universities participated in this program. The program was well attended by faculty, staff and students. Large number of students of all 16 colleges/universities of Karachi participated named: Dow University of Health Sciences, Ziauddin University, Jinnah Sindh Medical University, Baqai Medical University, Hamdard University, Bahria University, United Medical & Dental College, Jinnah Medical & Dental College, Liaquat College of Medicine & Dentistry, Virtual University, SMBBMC Lyari, Karachi Medical & Dental College, Aga Khan University, Al Tibri Medical College, Karachi Institute of Medical Sciences, Liaquat National Medical College actively participated in this event. Results are as under: Event Winner Runner Up Basket Ball Girls Bahria University Dow University -

Minutes of the 28Th Meeting of the General Council of the National Computing Education Accreditation Council, HEC, Islamabad
Minutes of the 28th Meeting of the General Council of the National Computing Education Accreditation Council, HEC, Islamabad The 28th meeting of NCEAC (National Computing Education Accreditation Council) was held on Thursday, 15th March 2018 in Learning & Innovation Hall, HEC, H-8/1, Islamabad. The following attended: 1. Dr Mohammad Ayub Alvi, Chairperson NCEAC 2. Dr Shoab Ahmad Khan, Vice Chairperson, NCEAC 3. Dr Aasia Khanum, Associate Professor, Forman Christian College, Lahore 4. Dr Faisal Ahmad Khan Kakar, Dean (Faculty of Sciences) BUITEMS, Quetta 5. Dr Jamil Ahmad, Vice Chancellor, Kohat University of Science &Technology, Kohat 6. Dr Manzoor Ilahi Tamimy, Associate Professor, CIIT, Islamabad 7. Dr Muhammad Ali Maud, Professor (CS & E Department), UET, Lahore 8. Dr Muhammad Jamil Sawar, Consultant, MTBC, Rawalpindi 9. Dr Sayeed Ghani, Associate Dean, IBA, Karachi 10. Dr Zartash Afzal Uzmi, Assoc. Prof., LUMS, Lahore 11. Mr Fahad Saeed Warsi, VC Engineer, Ministry of IT, Sindh 12. Mr Raza Sukhera, PM(IT/Internal Audit), Ministry of IT, Islamabad 13. Ms Humaira Qudus, Deputy Director, QAA, HEC 14. Mr Naseem Haider, Ass. Electronic Advisor, Ministry of Sci. & Tech., Islamabad 15. Mr Sajid Iqbal, Manager Domestic Business, PSEB, Islamabad The following could not attend: 1. Dr Riaz Ahmad, Advisor, QAA, HEC 2. Chairman, Punjab IT Board, Lahore 3. President PASHA, Karachi 4. Secretary Ministry of Education, Gilgit-Baltistan 5. Secretary Information Technology Dept. Govt. of Balochistan, Quetta 6. Director, IT Dept. Govt. of KPK, Peshawar Meeting of the General Council started with recitation of verses from Holy Koran by Dr Manzoor Elahi Tamimy. Chairperson NCEAC welcomed and thanked the members for attending this meeting. -

Final List of BDS Candidates Selected Under Aggregate Formula As Per 2Nd Priority of Pakistan Medical Commission Islamabad
Final List of BDS candidates selected under aggregate formula as per 2nd priority of Pakistan Medical Commission Islamabad. Important Instructions:- Admitting University reserves the right of rectifying inadvertent Error and omissions in the selection list (if any) Admissions are subject to verification of validity documents by the respective college. With reference PMC meeting dated 7th January 2020, no up-gradation will be granted to the candidates selected under aggregate formula as per 2nd priority of PMC Islamabad. Selected candidates are advised to deposit their fee on or before 24th January 2020 to respective college. In case of failure of depositing fee, as per PMDC/PMC regulation his / her selection will be cancelled and no any claim whatsoever will be entertained. Selected candidates have to submit their original documents to respective college. Colleges are advised to send updated report in respect of reporting and absent candidates latest by 24th January, 2020 upto 5:00 pm. PRIVATE SECTOR MEDICAL AND DENTAL UNIVERSITIES / COLLEGES OF SINDH PROVINCE SESSION 2019-2020 FINAL LIST OF BDS CANDIDATES SELECTED UNDER AGGREGATE FORMULA AS PER 2ND PRIORITY OF PAKISTAN MEDICAL COMMISSION ISLAMABAD. App Progra S No. Name Father Name College Perc Remarks No. m 1 17388 TASMIA HABIB HABIBULLAH Isra University, Hyderabad BDS 77.75 2 17288 Kajal Kishwar kumar Isra University, Hyderabad BDS 66.432 3 17507 SAMREEN NAZ ALLAH BUX Isra University, Hyderabad BDS 64.886 Altamash Institute of Dental 4 11503 SEERAT ZULFIQAR ZULFIQAR ALI BDS 64.864