Pdf and Reported If They Occurred
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Geographic Distribution of Hantaviruses Associated with Neotomine and Sigmodontine Rodents, Mexico Mary L
Geographic Distribution of Hantaviruses Associated with Neotomine and Sigmodontine Rodents, Mexico Mary L. Milazzo,1 Maria N.B. Cajimat,1 Hannah E. Romo, Jose G. Estrada-Franco, L. Ignacio Iñiguez-Dávalos, Robert D. Bradley, and Charles F. Fulhorst To increase our knowledge of the geographic on the North American continent are Bayou virus, Black distribution of hantaviruses associated with neotomine or Creek Canal virus (BCCV), Choclo virus (CHOV), New sigmodontine rodents in Mexico, we tested 876 cricetid York virus, and Sin Nombre virus (SNV) (3–7). Other rodents captured in 18 Mexican states (representing at hantaviruses that are principally associated with neotomine least 44 species in the subfamily Neotominae and 10 or North American sigmodontine rodents include Carrizal species in the subfamily Sigmodontinae) for anti-hantavirus virus (CARV), Catacamas virus, El Moro Canyon virus IgG. We found antibodies against hantavirus in 35 (4.0%) rodents. Nucleotide sequence data from 5 antibody-positive (ELMCV), Huitzilac virus (HUIV), Limestone Canyon rodents indicated that Sin Nombre virus (the major cause of virus (LSCV), Montano virus (MTNV), Muleshoe virus hantavirus pulmonary syndrome [HPS] in the United States) (MULV), Playa de Oro virus, and Rio Segundo virus is enzootic in the Mexican states of Nuevo León, San Luis (RIOSV) (8–14). Potosí, Tamaulipas, and Veracruz. However, HPS has not Specifi c rodents (usually 1 or 2 closely related been reported from these states, which suggests that in species) are the principal hosts of the hantaviruses, northeastern Mexico, HPS has been confused with other for which natural host relationships have been well rapidly progressive, life-threatening respiratory diseases. -

Hantavirus Disease Were HPS Is More Common in Late Spring and Early Summer in Seropositive in One Study in the U.K
Hantavirus Importance Hantaviruses are a large group of viruses that circulate asymptomatically in Disease rodents, insectivores and bats, but sometimes cause illnesses in humans. Some of these agents can occur in laboratory rodents or pet rats. Clinical cases in humans vary in Hantavirus Fever, severity: some hantaviruses tend to cause mild disease, typically with complete recovery; others frequently cause serious illnesses with case fatality rates of 30% or Hemorrhagic Fever with Renal higher. Hantavirus infections in people are fairly common in parts of Asia, Europe and Syndrome (HFRS), Nephropathia South America, but they seem to be less frequent in North America. Hantaviruses may Epidemica (NE), Hantavirus occasionally infect animals other than their usual hosts; however, there is currently no Pulmonary Syndrome (HPS), evidence that they cause any illnesses in these animals, with the possible exception of Hantavirus Cardiopulmonary nonhuman primates. Syndrome, Hemorrhagic Nephrosonephritis, Epidemic Etiology Hemorrhagic Fever, Korean Hantaviruses are members of the genus Orthohantavirus in the family Hantaviridae Hemorrhagic Fever and order Bunyavirales. As of 2017, 41 species of hantaviruses had officially accepted names, but there is ongoing debate about which viruses should be considered discrete species, and additional viruses have been discovered but not yet classified. Different Last Updated: September 2018 viruses tend to be associated with the two major clinical syndromes in humans, hemorrhagic fever with renal syndrome (HFRS) and hantavirus pulmonary (or cardiopulmonary) syndrome (HPS). However, this distinction is not absolute: viruses that are usually associated with HFRS have been infrequently linked to HPS and vice versa. A mild form of HFRS in Europe is commonly called nephropathia epidemica. -

Taxonomy of the Order Bunyavirales: Update 2019
Archives of Virology (2019) 164:1949–1965 https://doi.org/10.1007/s00705-019-04253-6 VIROLOGY DIVISION NEWS Taxonomy of the order Bunyavirales: update 2019 Abulikemu Abudurexiti1 · Scott Adkins2 · Daniela Alioto3 · Sergey V. Alkhovsky4 · Tatjana Avšič‑Županc5 · Matthew J. Ballinger6 · Dennis A. Bente7 · Martin Beer8 · Éric Bergeron9 · Carol D. Blair10 · Thomas Briese11 · Michael J. Buchmeier12 · Felicity J. Burt13 · Charles H. Calisher10 · Chénchén Cháng14 · Rémi N. Charrel15 · Il Ryong Choi16 · J. Christopher S. Clegg17 · Juan Carlos de la Torre18 · Xavier de Lamballerie15 · Fēi Dèng19 · Francesco Di Serio20 · Michele Digiaro21 · Michael A. Drebot22 · Xiaˇoméi Duàn14 · Hideki Ebihara23 · Toufc Elbeaino21 · Koray Ergünay24 · Charles F. Fulhorst7 · Aura R. Garrison25 · George Fú Gāo26 · Jean‑Paul J. Gonzalez27 · Martin H. Groschup28 · Stephan Günther29 · Anne‑Lise Haenni30 · Roy A. Hall31 · Jussi Hepojoki32,33 · Roger Hewson34 · Zhìhóng Hú19 · Holly R. Hughes35 · Miranda Gilda Jonson36 · Sandra Junglen37,38 · Boris Klempa39 · Jonas Klingström40 · Chūn Kòu14 · Lies Laenen41,42 · Amy J. Lambert35 · Stanley A. Langevin43 · Dan Liu44 · Igor S. Lukashevich45 · Tāo Luò1 · Chuánwèi Lüˇ 19 · Piet Maes41 · William Marciel de Souza46 · Marco Marklewitz37,38 · Giovanni P. Martelli47 · Keita Matsuno48,49 · Nicole Mielke‑Ehret50 · Maria Minutolo3 · Ali Mirazimi51 · Abulimiti Moming14 · Hans‑Peter Mühlbach50 · Rayapati Naidu52 · Beatriz Navarro20 · Márcio Roberto Teixeira Nunes53 · Gustavo Palacios25 · Anna Papa54 · Alex Pauvolid‑Corrêa55 · Janusz T. Pawęska56,57 · Jié Qiáo19 · Sheli R. Radoshitzky25 · Renato O. Resende58 · Víctor Romanowski59 · Amadou Alpha Sall60 · Maria S. Salvato61 · Takahide Sasaya62 · Shū Shěn19 · Xiǎohóng Shí63 · Yukio Shirako64 · Peter Simmonds65 · Manuela Sironi66 · Jin‑Won Song67 · Jessica R. Spengler9 · Mark D. Stenglein68 · Zhèngyuán Sū19 · Sùróng Sūn14 · Shuāng Táng19 · Massimo Turina69 · Bó Wáng19 · Chéng Wáng1 · Huálín Wáng19 · Jūn Wáng19 · Tàiyún Wèi70 · Anna E. -

Taxonomy of the Family Arenaviridae and the Order Bunyavirales: Update 2018
Archives of Virology https://doi.org/10.1007/s00705-018-3843-5 VIROLOGY DIVISION NEWS Taxonomy of the family Arenaviridae and the order Bunyavirales: update 2018 Piet Maes1 · Sergey V. Alkhovsky2 · Yīmíng Bào3 · Martin Beer4 · Monica Birkhead5 · Thomas Briese6 · Michael J. Buchmeier7 · Charles H. Calisher8 · Rémi N. Charrel9 · Il Ryong Choi10 · Christopher S. Clegg11 · Juan Carlos de la Torre12 · Eric Delwart13,14 · Joseph L. DeRisi15 · Patrick L. Di Bello16 · Francesco Di Serio17 · Michele Digiaro18 · Valerian V. Dolja19 · Christian Drosten20,21,22 · Tobiasz Z. Druciarek16 · Jiang Du23 · Hideki Ebihara24 · Toufc Elbeaino18 · Rose C. Gergerich16 · Amethyst N. Gillis25 · Jean‑Paul J. Gonzalez26 · Anne‑Lise Haenni27 · Jussi Hepojoki28,29 · Udo Hetzel29,30 · Thiện Hồ16 · Ní Hóng31 · Rakesh K. Jain32 · Petrus Jansen van Vuren5,33 · Qi Jin34,35 · Miranda Gilda Jonson36 · Sandra Junglen20,22 · Karen E. Keller37 · Alan Kemp5 · Anja Kipar29,30 · Nikola O. Kondov13 · Eugene V. Koonin38 · Richard Kormelink39 · Yegor Korzyukov28 · Mart Krupovic40 · Amy J. Lambert41 · Alma G. Laney42 · Matthew LeBreton43 · Igor S. Lukashevich44 · Marco Marklewitz20,22 · Wanda Markotter5,33 · Giovanni P. Martelli45 · Robert R. Martin37 · Nicole Mielke‑Ehret46 · Hans‑Peter Mühlbach46 · Beatriz Navarro17 · Terry Fei Fan Ng14 · Márcio Roberto Teixeira Nunes47,48 · Gustavo Palacios49 · Janusz T. Pawęska5,33 · Clarence J. Peters50 · Alexander Plyusnin28 · Sheli R. Radoshitzky49 · Víctor Romanowski51 · Pertteli Salmenperä28,52 · Maria S. Salvato53 · Hélène Sanfaçon54 · Takahide Sasaya55 · Connie Schmaljohn49 · Bradley S. Schneider25 · Yukio Shirako56 · Stuart Siddell57 · Tarja A. Sironen28 · Mark D. Stenglein58 · Nadia Storm5 · Harikishan Sudini59 · Robert B. Tesh48 · Ioannis E. Tzanetakis16 · Mangala Uppala59 · Olli Vapalahti28,30,60 · Nikos Vasilakis48 · Peter J. Walker61 · Guópíng Wáng31 · Lìpíng Wáng31 · Yànxiăng Wáng31 · Tàiyún Wèi62 · Michael R. -

Taxonomy of the Order Bunyavirales: Second Update 2018
HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author Arch Virol Manuscript Author . Author manuscript; Manuscript Author available in PMC 2020 March 01. Published in final edited form as: Arch Virol. 2019 March ; 164(3): 927–941. doi:10.1007/s00705-018-04127-3. TAXONOMY OF THE ORDER BUNYAVIRALES: SECOND UPDATE 2018 A full list of authors and affiliations appears at the end of the article. Abstract In October 2018, the order Bunyavirales was amended by inclusion of the family Arenaviridae, abolishment of three families, creation of three new families, 19 new genera, and 14 new species, and renaming of three genera and 22 species. This article presents the updated taxonomy of the order Bunyavirales as now accepted by the International Committee on Taxonomy of Viruses (ICTV). Keywords Arenaviridae; arenavirid; arenavirus; bunyavirad; Bunyavirales; bunyavirid; Bunyaviridae; bunyavirus; emaravirus; Feraviridae; feravirid, feravirus; fimovirid; Fimoviridae; fimovirus; goukovirus; hantavirid; Hantaviridae; hantavirus; hartmanivirus; herbevirus; ICTV; International Committee on Taxonomy of Viruses; jonvirid; Jonviridae; jonvirus; mammarenavirus; nairovirid; Nairoviridae; nairovirus; orthobunyavirus; orthoferavirus; orthohantavirus; orthojonvirus; orthonairovirus; orthophasmavirus; orthotospovirus; peribunyavirid; Peribunyaviridae; peribunyavirus; phasmavirid; phasivirus; Phasmaviridae; phasmavirus; phenuivirid; Phenuiviridae; phenuivirus; phlebovirus; reptarenavirus; tenuivirus; tospovirid; Tospoviridae; tospovirus; virus classification; virus nomenclature; virus taxonomy INTRODUCTION The virus order Bunyavirales was established in 2017 to accommodate related viruses with segmented, linear, single-stranded, negative-sense or ambisense RNA genomes classified into 9 families [2]. Here we present the changes that were proposed via an official ICTV taxonomic proposal (TaxoProp 2017.012M.A.v1.Bunyavirales_rev) at http:// www.ictvonline.org/ in 2017 and were accepted by the ICTV Executive Committee (EC) in [email protected]. -
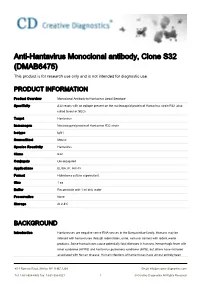
Anti-Hantavirus Monoclonal Antibody, Clone S32 (DMAB6475) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-Hantavirus Monoclonal antibody, Clone S32 (DMAB6475) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Product Overview Monoclonal Antibody to Hantavirus Seoul Serotype Specificity S32 reacts with an epitope present on the nucleocapsid protein of Hantavirus strain R22 (also called Seoul or SEO) Target Hantavirus Immunogen Nucleocapsid protein of Hantavirus R22 strain Isotype IgG1 Source/Host Mouse Species Reactivity Hantavirus Clone S32 Conjugate Unconjugated Applications ELISA, IF, IHC-Fr Format Hybridoma culture supernatant Size 1 ea Buffer Reconstitute with 1 ml dist. water Preservative None Storage At 2-8℃ BACKGROUND Introduction Hantaviruses are negative sense RNA viruses in the Bunyaviridae family. Humans may be infected with hantaviruses through rodent bites, urine, saliva or contact with rodent waste products. Some hantaviruses cause potentially fatal diseases in humans, hemorrhagic fever with renal syndrome (HFRS) and hantavirus pulmonary syndrome (HPS), but others have not been associated with human disease. Human infections of hantaviruses have almost entirely been 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved linked to human contact with rodent excrement, but recent human-to-human transmission has been reported with the Andes virus in South America. The name hantavirus is derived from the Hantan River area in South Korea, which provided the founding member of the group: Hantaan virus (HTNV), isolated in the late 1970s by Ho-Wang Lee and colleagues. HTNV is one of several hantaviruses that cause HFRS, formerly known as Korean hemorrhagic fever. -

Pathogenic Landscape of Transboundary Zoonotic Diseases in the Mexico–US Border Along the Rio Grande
University of Texas Rio Grande Valley ScholarWorks @ UTRGV Biology Faculty Publications and Presentations College of Sciences 11-17-2014 Pathogenic landscape of transboundary zoonotic diseases in the Mexico–US border along the Rio Grande Maria Dolores Esteve-Gassent Adalberto A. Pérez de León Dora Romero-Salas Teresa Patricia Feria-Arroyo The University of Texas Rio Grande Valley Ramiro Patino The University of Texas Rio Grande Valley See next page for additional authors Follow this and additional works at: https://scholarworks.utrgv.edu/bio_fac Part of the Animal Sciences Commons, and the Biology Commons Recommended Citation Esteve-Gassent, Maria Dolores, Adalberto A. Pérez de León, Dora Romero-Salas, Teresa P. Feria-Arroyo, Ramiro Patino, Ivan Castro-Arellano, Guadalupe Gordillo-Pérez, et al. 2014. “Pathogenic Landscape of Transboundary Zoonotic Diseases in the Mexico–US Border Along the Rio Grande.” Frontiers in Public Health 2. https://doi.org/10.3389/fpubh.2014.00177. This Article is brought to you for free and open access by the College of Sciences at ScholarWorks @ UTRGV. It has been accepted for inclusion in Biology Faculty Publications and Presentations by an authorized administrator of ScholarWorks @ UTRGV. For more information, please contact [email protected], [email protected]. Authors Maria Dolores Esteve-Gassent, Adalberto A. Pérez de León, Dora Romero-Salas, Teresa Patricia Feria- Arroyo, Ramiro Patino, and John A. Goolsby This article is available at ScholarWorks @ UTRGV: https://scholarworks.utrgv.edu/bio_fac/128 REVIEW ARTICLE published: 17 November 2014 PUBLIC HEALTH doi: 10.3389/fpubh.2014.00177 Pathogenic landscape of transboundary zoonotic diseases in the Mexico–US border along the Rio Grande Maria Dolores Esteve-Gassent 1*†, Adalberto A. -

Pathogenic Landscape of Transboundary Zoonotic Diseases in the Mexico–US Border Along the Rio Grande
REVIEW ARTICLE published: 17 November 2014 PUBLIC HEALTH doi: 10.3389/fpubh.2014.00177 Pathogenic landscape of transboundary zoonotic diseases in the Mexico–US border along the Rio Grande Maria Dolores Esteve-Gassent 1*†, Adalberto A. Pérez de León2†, Dora Romero-Salas 3,Teresa P. Feria-Arroyo4, Ramiro Patino4, Ivan Castro-Arellano5, Guadalupe Gordillo-Pérez 6, Allan Auclair 7, John Goolsby 8, Roger Ivan Rodriguez-Vivas 9 and Jose Guillermo Estrada-Franco10 1 Department of Veterinary Pathobiology, College of Veterinary Medicine and Biomedical Sciences, Texas A&M University, College Station, TX, USA 2 USDA-ARS Knipling-Bushland U.S. Livestock Insects Research Laboratory, Kerrville, TX, USA 3 Facultad de Medicina Veterinaria y Zootecnia, Universidad Veracruzana, Veracruz, México 4 Department of Biology, University of Texas-Pan American, Edinburg, TX, USA 5 Department of Biology, College of Science and Engineering, Texas State University, San Marcos, TX, USA 6 Unidad de Investigación en Enfermedades Infecciosas, Centro Médico Nacional SXXI, IMSS, Distrito Federal, México 7 Environmental Risk Analysis Systems, Policy and Program Development, Animal and Plant Health Inspection Service, United States Department of Agriculture, Riverdale, MD, USA 8 Cattle Fever Tick Research Laboratory, United States Department of Agriculture, Agricultural Research Service, Edinburg, TX, USA 9 Facultad de Medicina Veterinaria y Zootecnia, Cuerpo Académico de Salud Animal, Universidad Autónoma de Yucatán, Mérida, México 10 Facultad de Medicina Veterinaria Zootecnia, Centro de Investigaciones y Estudios Avanzados en Salud Animal, Universidad Autónoma del Estado de México, Toluca, México Edited by: Transboundary zoonotic diseases, several of which are vector borne, can maintain a dynamic Juan-Carlos Navarro, Universidad focus and have pathogens circulating in geographic regions encircling multiple geopoliti- Central de Venezuela, Venezuela cal boundaries. -

Infarto Da Artéria De Percheron: Relato De Caso
REVISTA BRASILEIRA DE NEUROLOGIA Órgão Oficial do Instituto de Neurologia Deolindo Couto Vol. 56 • Nº 3 • JUL / AGO / SET - 2020 Revista Brasileira de Neurologia » Volume 56 » Nº 3 » JUL/AGO/SET 2020 1 ISSN 0101-8469 CODEN RBNEES ISSN eletrônico: 2447-2573 Acesso pelo LILACS-Express REVISTA BRASILEIRA DE NEUROLOGIA Órgão Oficial do Instituto de Neurologia Deolindo Couto Editorial............................................................................................................................. 4 Pulmonary capacity of patients with total traumatic injury of the brachial plexus submitted to neurotization with the phrenic nerve: a case series................................................................................................... 5 Camilla Fernandes de Melo, Armèle Dornelas de Andrade, Fernando Henrique Souza, Helen Kerlen Bastos Fuzari, Juliana Fernandes, Silvya Nery Bernardino, Daniella Araújo de Oliveira Conhecimento da população sobre Acidente Vascular Cerebral em Torres RS........................................... 11 Valmir Soares Machado, Lidiane de Medeiros Hahn, Maria Isabel Morgan Martins, Luiz Carlos Porcello Marrone Guillain-Barré syndrome: advances and future perspectives................................................................ 15 Rabello, Francisco de AP Cabral Júnior; Pupe, Camila Castelo Branco; Nascimento, Osvaldo JM. Infarto da artéria de Percheron: relato de caso................................................................................ 21 João Carlos Cervelin, Matheus Muller da Rosa, Rafael -

The Tangled Story of Alois Alzheimer
Bratisl Lek Listy 2006; 107 (910): 343345 343 TOPICAL REVIEW The tangled story of Alois Alzheimer Zilka N, Novak M Institute of Neuroimmunology, AD Centre of Excellence, Slovak Academy of Sciences, Bratislava, Slovakia. [email protected] Abstract In 1907, Bavarian psychiatrist Alois Alzheimer, who is considered to be a founding father of neuropa- thology, was first to describe the main neuropathologic characteristics of the peculiar disease in the brain of a woman showing progressive dementia when she was in her early 50s. Using a newly deve- loped Bielschowskys silver staining method, Alzheimer observed degenerating neurons with bundles of fibrils (neurofibrillary tangles) and miliary foci of silver-staining deposits scattered over the cortex (senile plaques). In 1910 Emil Kraepelin (Alois Alzheimers superior) coined the term Alzheimers disease to distinguish the presenile form of dementia from the more common senile variant. Alzheimers findings were followed up, and soon a number of reports of similar cases appeared in the literature. During the time, both pathological hallmarks of Alzheimers disease became the gold standard for post-mortem diagnosis of the disease. One hundred years later, dementia of Alzheimers type is con- sidered to be one of the most devastating illnesses of old age. Despite intensive research the cause of the disease still remains elusive (Fig. 2, Ref. 17). Key words: Alzheimers disease, Alois Alzheimer, Augusta D, neurofibrillary tangles, senile plaques. Alois Alzheimer was born in June 14, 1864 in Markbreit am pathology of the nervous system, studying in particular the nor- Main in Southern Germany. He commenced the study of medi- mal and pathological anatomy of the cerebral cortex. -

Mouse Anti-HFRS Virus, Hanta Strain Monoclonal Antibody
SPECIFICATION SHEET Rev 110621MAB-S0006 Mouse Anti-HFRS Virus, Hanta strain Monoclonal Antibody Mouse, Monoclonal (HFRS Virus, Hanta strain) Cat. No. DMAB3487 Lot. No. (See product label) PRODUCT INFORMATION BACKGROUND Introduction: Hantaviruses (family Bunyaviridae, genus Han- Product Overview: Monoclonal Antibody to Hemorrhagic tavirus) are rodent-borne, zoonotic (acquired from animals), fever with renal syndrome (HFRS) Virus, Hanta Strain enveloped RNA viruses, and include the causative agents of Specificity: Specific for HFRS Virus. Strain: Hanta haemorrhagic fever with renal syndrome (HFRS). The viruses Immunogen: Inactivated virus particles that cause HFRS include Hanta, Dobrava, Seoul, and Puu- Clone: C963M mala. Dobrova and Hanta viruses cause a more severe HFRS Isotype: IgG1 with fever, haemorrhage, and renal failure, and a mortality rate Host animal: Mouse. Hybridization of Sp2/0 myeloma cells of up to 15%. The mildest form of HFRS is caused by Puu- with spleen cells from BALB/c mice. mala virus. Source: Ascites Keywords: Hemorrhagic fever with renal syndrome Virus; Format: Purified, Liquid HFRS virus, Hanta strain; HFRS virus; Hemorrhagic fever with Applications: Suitable for use in ELISA. Each laboratory renal syndrome Virus, Hanta strain; Hantaviruses; Bunyaviri- should determine an optimum working titer for use in its par- dae; Hantavirus; Hemorrhagic fever with renal syndrome Vi- ticular application. Other applications have not been tested rus; HFRS Virus Dobrava, Puumala, Hanta and Seoul Strains; but use in such assays -

Ethics of Ambient Assisted Living Technologies for Persons with Dementia, © January 2016 DECLARATION
peter novitzky ETHICSOFAMBIENTASSISTEDLIVINGTECHNOLOGIESFOR PERSONSWITHDEMENTIA ETHICSOFAMBIENTASSISTEDLIVING TECHNOLOGIESFORPERSONSWITHDEMENTIA peter novitzky ThLic., M.A., MSc. A Dissertation submitted in fulfilment of the requirements for the award of Doctor of Philosophy (Ph.D.) to the Dublin City University School of Computing Prof Bert Gordijn Prof Alan F. Smeaton (supervisory panel) January 2016 Peter Novitzky: Ethics of Ambient Assisted Living Technologies for Persons with Dementia, © January 2016 DECLARATION I hereby certify that this material, which I now submit for assessment on the programme of study leading to the award of Ph.D. is entirely my own work, that I have exercised reasonable care to ensure that the work is original, and does not to the best of my knowledge breach any law of copyright, and has not been taken from the work of others save and to the extent that such work has been cited and acknowledged within the text of my work. Signed: ID No.: 12210395 Date: 04/01/2016 ACKNOWLEDGMENTS My first and foremost thanks goes to my supervisors Prof Bert Gordijn, and Prof Alan F. Smeaton. Their contribution to the successful completion of this thesis was invaluable, as was their continuous support during the times of joy but also despair, which cannot be emphasised enough. I would also like to express my thanks to all the people at CLARITY – Centre For Sensor Web Technologies, Dublin City University, and INSIGHT – Centre For Data Ana- lytics who supported me in my work, particularly, Renaat Verbruggen, Eamon Newman, Tim Jacquemard, Deirdre Sheridan, Margaret Malone, Jonny Hobson, as well as many others. I wish to express my deep gratitude to my family, those passed away and alive, who supported or contributed to the success of my work.