Mclaren Health Plan Medicaid Prior Authorization Guidelines
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Drug Administration Routes - Summary
Only Use L6. DrugCourse Administration & Transport 207 by Fluid Motion 243/CENG April 19, 2018 NANO Only Use Course 207 243/CENG Part I: Drug Administration NANO Routes of Drug Administration Only Topical: local effect, substanceUse is applied directly where its action is desired. EnteralCourse: systemic effect, substance is 207given via the gastrointestinal (GI) tract. Parenteral: systemic effect, substance is given by routes other than the gastrointestinal (GI) tract. 243/CENG NANO Topical Drug Delivery Epicutaneous – directly onto the surface of the skin Only allergy testing local anesthesia… Use Eye drops antibiotics for conjunctivitis … Course Inhalational207 asthma medications acute infection in upper airway … 243/CENG Intranasal route decongestant nasal sprays … NANO Enteral Drug Delivery Any form of administration that involves any part of the gastrointestinalOnly tract Use Course 207 Oral: Rectal: Gastric feeding tube: many drugs as tablets, various drugs in many drugs, enteral capsules, drops… suppository or enema nutrition… form… 243/CENG NANO Parenteral Drug Delivery Intravenous: into a vein (many drugs, total parenteral nutrition…) Only Intramuscular: into a muscle (many vaccines, antibiotics…) Use Subcutaneous: under the skin (insulin…) Intraarterial: into an artery (vasodilator drugs in the treatment of vasospasm…) Course Intradermal: into the skin itself (skin testing some allergens, tattoos…) 207 Transdermal: diffusion through the intact skin (transdermal opioid patches in pain management, nicotine patches for treatment -
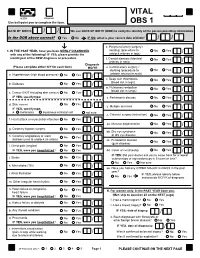
VITAL Jan 2019 Follow-Up
VITAL 6308 Request Use ball-point pen to complete the form. OBS 1 DATE OF BIRTH: / / We use DATE OF BIRTH (DOB) to verify the identity of the person providing information. Is the DOB above correct? Yes No IF NO, what is your correct date of birth? / / s. Peripheral artery surgery / 1. IN THE PAST YEAR, have you been NEWLY DIAGNOSED stenting (procedure to No Yes / with any of the following? IF YES, please provide the unblock arteries in legs) month/year of the NEW diagnosis or procedure. t. Carotid stenosis (blocked No Yes Answer NO/YES on each line. arteries in neck) / Diagnosis (Please complete either N/Y for each item) MO/YR u. Carotid artery surgery / stenting (procedure to No Yes / a. Hypertension (high blood pressure) No Yes / unblock arteries in neck) v. Deep vein thrombosis No Yes (blood clot in legs) / b. Diabetes No Yes / w. Pulmonary embolism No Yes (blood clot in lungs) / c. Cancer (NOT including skin cancer) No Yes / IF YES, specify type: _______________________ x. Parkinson's disease No Yes / d. Skin cancer No Yes / y. Multiple sclerosis No Yes IF YES, specify type: / e. melanoma squamous or basal cell not sure z. Cataract surgery (extraction) No Yes / f. Heart attack or myocardial infarction No Yes / aa. Macular degeneration No Yes / g. Coronary bypass surgery No Yes / bb. Dry eye syndrome No Yes or dry eye disease / h. Coronary angioplasty or stent No Yes (balloon used to unblock an artery) / cc. Periodontal disease No Yes (gum disease) / i. Chest pain (angina) No Yes / IF YES, were you hospitalized? No Yes dd. -

Effects of Intraoperative Insufflation with Warmed, Humidified CO2 During Abdominal Surgery: a Review
Annals of Original Article Coloproctology Ann Coloproctol 2018;34(3):125-137 pISSN 2287-9714 eISSN 2287-9722 https://doi.org/10.3393/ac.2017.09.26 www.coloproctol.org Effects of Intraoperative Insufflation With Warmed, Humidified CO2 during Abdominal Surgery: A Review Ju Yong Cheong1,2, Anil Keshava1, Paul Witting2, Christopher John Young1 1Colorectal Surgical Department, Concord Repatriation General Hospital, Sydney Medical School, The University of Sydney, Sydney; 2Discipline of Pathology, Charles Perkins Centre, Sydney Medical School, The University of Sydney, Sydney, Australia Purpose: During a laparotomy, the peritoneum is exposed to the cold, dry ambient air of the operating room (20°C, 0%– 5% relative humidity). The aim of this review is to determine whether the use of humidified and/or warmed CO2 in the intraperitoneal environment during open or laparoscopic operations influences postoperative outcomes. Methods: A review was performed in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. The PubMed, OVID MEDLINE, Cochrane Central Register of Controlled Trials and Embase databases were searched for articles published between 1980 and 2016 (October). Comparative studies on humans or nonhuman animals that involved randomized controlled trials (RCTs) or prospective cohort studies were included. Both laparotomy and laparoscopic studies were included. The primary outcomes identified were peritoneal inflammation, core body temperature, and postoperative pain. Results: The literature search identified 37 articles for analysis, including 30 RCTs, 7 prospective cohort studies, 23 human studies, and 14 animal studies. Four studies found that compared with warmed/humidified CO2, cold, dry CO2 resulted in significant peritoneal injury, with greater lymphocytic infiltration, higher proinflammatory cytokine levels and peritoneal adhesion formation. -

West Virginia Nerve Injury Slides
Anesthesia for Robotic Surgery: Is it a Different Ball Game? Michael A. Olympio, M.D. Professor of Anesthesiology Wake Forest University School of Medicine YES, it is… Access to, and monitoring the patient Combined Pneumoperitoneum and Trendelenburg – Type and amount of inflation gas – Pulmonary impairments – Hydrostatic gradients – Cardiovascular derangements – Circulation to the lower limb – Confounding obesity Anesthetic adjuncts and outcomes – Routine general anesthesia – General and regional? – Multimodal, narcotic-sparing, “ideal” anesthetic Olympio, MA. “Anesthetic Considerations for Robotic Urologic Surgery” In, Hemal AK, Menon M (eds.) Robotic Urologic Surgery. New York: Springer-Verlag, 2011. Photo of RALRP At the end of this lecture, the learner will explain or understand: – the physiological derangements associated with combined pneumoperitoneum and Trendelenburg posture – the relationships between, and significance of hydrostatic pressure, blood pressure measurement and the risks of organ hypo/hyper-perfusion – the reasons for choosing specific anesthetic management techniques and drugs. No disclosures. What you should know about your own surgical outcomes: operative time nausea and vomiting rates blood loss use of intermittent morbidity types and rates pneumatic serial compression (IPSC) length of stay and criteria for discharge desired extremes of TP mortality (if any and its desired intra-abdominal cause) inflation pressures (IAP) postoperative pain and and, type of inflation gas analgesic regimens Pre-Anesthetic -
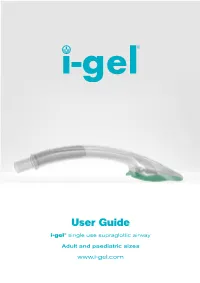
I-Gel User Guide
User Guide i-gel® single use supraglottic airway Adult and paediatric sizes www.i-gel.com Contents 1.0 Introduction .................................................................................................................... 2 1.1 The i-gel design ..................................................................................................................................................2 1.2 Key components and their function .........................................................................................................3 1.2.1 Soft non-inflatable cuff ................................................................................................................4 1.2.2 Gastric channel .............................................................................................................................4 1.2.3 Epiglottic rest ................................................................................................................................4 1.2.4 Buccal cavity stabiliser ................................................................................................................4 1.2.5 15mm connector ..........................................................................................................................5 1.2.6 Important key points.....................................................................................................................5 2.0 Indications ..................................................................................................................... -

Clinical and Biochemical Outcomes of Cinacalcet Treatment of Familial
Rasmussen et al. Journal of Medical Case Reports 2011, 5:564 JOURNAL OF MEDICAL http://www.jmedicalcasereports.com/content/5/1/564 CASE REPORTS CASEREPORT Open Access Clinical and biochemical outcomes of cinacalcet treatment of familial hypocalciuric hypercalcemia: a case series Anne Qvist Rasmussen1*, Niklas Rye Jørgensen1,2 and Peter Schwarz1,3 Abstract Introduction: Familial hypocalciuric hypercalcemia is a rare benign autosomal-dominant genetic disease with high penetrance. In most cases, patients with familial hypocalciuric hypercalcemia experience unspecific physical discomfort or asymptomatic disease. These patients are typically characterized by mild to moderately increased blood ionized calcium and a normal to slightly elevated serum parathyroid hormone. Case presentation: Four female patients with familial hypocalciuric hypercalcemia with inactivating mutations in the CaSR gene were included in the treatment study. Three patients were related: two were siblings and one was the daughter of one of these. The ages of the related patients were 51 years, 57 years and 35 years. All three patients were carriers of the same mutation. The fourth patient, unrelated to the others, was 53 years old, and a carrier of a novel and previously unknown mutation leading to familial hypocalciuric hypercalcemia. All four patients were Caucasians of Danish nationality. Biochemically, all patients had elevated blood ionized calcium, serum parathyroid hormone, serum magnesium and total serum calcium, except one, whose serum parathyroid hormone was within the normal range prior to treatment. All patients were treated with cinacalcet in a dosage of 30 mg to 60 mg per day. Conclusion: Three months after the initiation of cinacalcet treatment, all our patients experiencing clinical signs of hypercalcemia had improved in self -reported well-being and in biochemical parameters. -
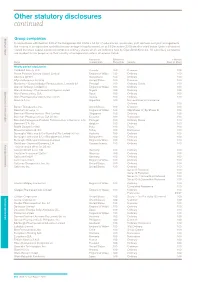
Other Statutory Disclosures Continued
Other statutory disclosures continued Strategic reportGroup companies Governance & remuneration Financial statements In accordance with Section 409 of the Companies Act 2006 a full list of subsidiaries, associates, joint ventures and joint arrangements, the country of incorporation and effective percentage of equity owned, as at 31 December 2015 are disclosed below. Unless otherwise stated the share capital disclosed comprises ordinary shares which are indirectly held by GlaxoSmithKline plc. All subsidiary companies are resident for tax purposes in their country of incorporation unless otherwise stated. Country of Effective % % Held by Name incorporation Ownership Security Class of Share Wholly owned subsidiaries 1506369 Alberta ULC Canada 100 Common 100 Action Potential Venture Capital Limited England & Wales 100 Ordinary 100 Adechsa GmbH Switzerland 100 Ordinary 100 Affymax Research Institute United States 100 Common 100 Alenfarma – Especialidades Farmaceuticas, Limitada (iv) Portugal 100 Ordinary Quota 100 Allen & Hanburys Limited (iv) England & Wales 100 Ordinary 100 Allen & Hanburys Pharmaceutical Nigeria Limited Nigeria 100 Ordinary 100 Allen Farmaceutica, S.A. Spain 100 Ordinary 100 Allen Pharmazeutika Gesellschaft m.b.H. Austria 100 Ordinary 100 Aners S.A (iv) Argentina 100 Non-endorsable Nominative Ordinary 100 Barrier Therapeutics, Inc. United States 100 Common 100 Beecham Group p l c England & Wales 100 20p Shares 'A'; 5p Shares B 100 Beecham Pharmaceuticals (Pte) Limited Singapore 100 Ordinary 100 Beecham Pharmaceuticals S.A (iv) (vi) Ecuador 100 Nominative 100 Beecham Portuguesa-Produtos Farmaceuticos e Quimicos, Lda Portugal 100 Ordinary Quota 100 Beecham S.A. (iv) Belgium 100 Ordinary 100 Biddle Sawyer Limited India 100 Equity 100 Biovesta Ilaçlari Ltd. Sti. Turkey 100 Nominative 100 Burroughs Wellcome & Co (Australia) Pty Limited (iv) (vi) Australia 100 Ordinary 100 Burroughs Wellcome & Co (Bangladesh) Limited Bangladesh 100 Ordinary 100 Burroughs Wellcome International Limited England & Wales 100 Ordinary 100 Caribbean Chemical Company, Ltd. -

Mimpara, INN-Cinacalcet
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Mimpara 30 mg film-coated tablets Mimpara 60 mg film-coated tablets Mimpara 90 mg film-coated tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Mimpara 30 mg film-coated tablets Each tablet contains 30 mg cinacalcet (as hydrochloride). Excipient with known effect Each tablet contains 2.74 mg of lactose. Mimpara 60 mg film-coated tablets Each tablet contains 60 mg cinacalcet (as hydrochloride). Excipient with known effect Each tablet contains 5.47 mg of lactose. Mimpara 90 mg film-coated tablets Each tablet contains 90 mg cinacalcet (as hydrochloride). Excipient with known effect Each tablet contains 8.21 mg of lactose. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Film-coated tablet (tablet). Mimpara 30 mg film-coated tablets Light green, oval (approximately 9.7 mm long and 6.0 mm wide), film-coated tablet marked “AMG” on one side and “30” on the other. Mimpara 60 mg film-coated tablets Light green, oval (approximately 12.2 mm long and 7.6 mm wide), film-coated tablet marked “AMG” on one side and “60” on the other. Mimpara 90 mg film-coated tablets Light green, oval (approximately 13.9 mm long and 8.7 mm wide), film-coated tablet marked “AMG” on one side and “90” on the other. 2 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Secondary hyperparathyroidism Adults Treatment of secondary hyperparathyroidism (HPT) in adult patients with end-stage renal disease (ESRD) on maintenance dialysis therapy. Paediatric population Treatment of secondary hyperparathyroidism (HPT) in children aged 3 years and older with end-stage renal disease (ESRD) on maintenance dialysis therapy in whom secondary HPT is not adequately controlled with standard of care therapy (see section 4.4). -

In This Section
Strategic report In this section Chairman’s statement 2 CEO’s review 4 Business overview 6 The global context 8 Our business model 12 Our strategic priorities 14 How we performed 16 Risk management 18 Grow 20 Deliver 32 Simplify 44 Our financial architecture 48 Responsible business 50 Financial review 58 Strategic report Chairman’s statement Chairman’s statement To shareholders The value of the significant changes that have been made in recent years is evidenced in our performance this year “ Since Sir Andrew became It is clear from the following pages that Through the Audit & Risk Committee, we the Group made good progress against oversee the issues and challenges faced by CEO, the company has its strategy in 2013. management, and encourage the creation of an environment in which GSK can achieve The Board believes the business is seeing returned £30 billion its strategic ambitions in a responsible and the benefits of the significant changes the sustainable manner. to shareholders.” management team has driven over recent years to deliver sustainable growth, reduce risk and I have no doubt that commercial success is enhance returns to shareholders. directly linked to operating in a responsible way and which meets the changing expectations of The notably strong performance from the society. In this respect, the company continues R&D organisation in 2013 – with six major to adopt industry-leading positions on a range new product approvals in areas including of issues. respiratory disease, HIV and cancer – is critical to the longer-term prospects of the The announcement of plans during 2013 to Group. -

Download the Evonik for More Information!
ADVANCED APPROACHES THE PRESCRIPTION CAN WE ACHIEVE FOR DELAYED-RELEASE ABUSE EPIDEMIC: EFFECTIVE ORAL P04 FORMULATIONS P18 DESIGNING A SOLUTION P32 DELIVERY OF VACCINES? NOVEL ORAL DELIVERY SYSTEMS 77 O 2017 • ISSUE N 2017 TH JULY 17 JULY Contents o TH ONdrugDelivery Issue N 77, July 17 , 2017 Advanced Approaches for Delayed-Release Formulations Maria Montero Mirabet, Senior Project Manager, NOVEL ORAL DELIVERY SYSTEMS Drug Delivery Services, Business Line Health Care, and 4 - 9 Brigitte Skalsky, Senior Director, Scientific Communication, This edition is one in the ONdrugDelivery series Business Line Health Care of publications from Frederick Furness Publishing. Evonik Nutrition & Care Each issue focuses on a specific topic within the field of drug delivery, and is supported by industry Technologies & Clinical Studies for the Oral Delivery of Calcitonin Nozer Mehta, Principal leaders in that field. Peptide Technologies James P Gilligan, Chief Scientific Officer 12 MONTH EDITORIAL CALENDAR 10 - 16 Tarsa Therapeutics Sep Wearable Injectors William Stern, Consultant Peptide Drug Development Oct Prefilled Syringes Nov Pulmonary & Nasal Delivery The Prescription Abuse Epidemic: Designing a Solution Dec Connecting Drug Delivery Aia Malik, Healthcare Product Manager, and 18 - 20 Gemma Budd, Director of Technologies and Strategy Jan ‘18 Ophthalmic Delivery Lucideon Feb Prefilled Syringes Mar Skin Drug Delivery: Targeting the End Goal: Opportunities & Innovations in Colonic Drug Delivery Dermal, Transdermal & Microneedles Sejal R Ranmal, Director -

MSM Chapter 1200 3/1/21
MEDICAID SERVICES MANUAL TRANSMITTAL LETTER February 23, 2021 TO: CUSTODIANS OF MEDICAID SERVICES MANUAL FROM: JESSICA KEMMERER, HIPAA PRIVACY AND CIVIL RIGHTS OFFICER /Jessica Kemmerer/ BACKGROUND AND EXPLANATION The DHCFP is proposing revisions to Medicaid Services Manual (MSM), Chapter 1200 – Prescribed Drugs, Appendix A, to reflect recommendations approved on October 22, 2020, by the Drug Use Review (DUR) Board. The proposed changes include the addition of new prior authorization criteria for Doxepine Topical, the addition of new prior authorization criteria for Zeposia® (ozanimod), addition of new prior authorization for Evenity® (romosozumab-aqqg), Prolia® (denosumab), Forteo® (teriparatide) and Tymlos® (abaloparatide) within a new combined osteoporosis agents section, and addition of new prior authorization criteria for Orilissa® (elagolix) and Oriahnn® (elagolix, estradiol, and norethindrone) within a new Gonadorpin Hormone Receptor (GnRH) Antagonist and Combinations section. Additionally, the DHCFP is proposing revisions to the existing prior authorization criteria for psychotropic medications for children and adolescents, and revision to the existing clinical criteria for Epidiolex® (cannabidiol). Throughout the chapter, grammar, punctuation and capitalization changes were made, duplications removed, acronyms used and standardized, and language reworded for clarity. Renumbering and re- arranging of sections was necessary. These changes are effective March 1, 2021. MATERIAL TRANSMITTED MATERIAL SUPERSEDED MTL N/A MTL N/A MSM Ch 1200 – Prescribed Drugs MSM Ch 1200 – Prescribed Drugs Background and Explanation of Policy Changes, Manual Section Section Title Clarifications and Updates Appendix A Psychotropic Added new policy language criteria on which specific Section N Medications for drug classes may bypass polypharmacy clinical criteria. Children and Adolescents Appendix A Reserved for Future Created a new section titled “Doxepin Topical.” Added Section W Use new prior authorization criteria for doxepin topical. -

2017 Fda Peptide Harvest
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 10 April 2018 doi:10.20944/preprints201804.0126.v1 Peer-reviewed version available at Pharmaceuticals 2018, 11, 42; doi:10.3390/ph11020042 1 Review 2 2017 FDA PEPTIDE HARVEST 3 Othman Al Musaimi,1,2,# Danah Alshaer, 1,2,# Beatriz G. de la Torre,3,* Fernando Albericio,2,4,5.* 4 1 College of Health Sciences, University of KwaZulu-Natal, Durban 4000, South Africa 5 2 School of Chemistry, University of KwaZulu-Natal, Durban 4001, South Africa 6 3 KRISP, College of Health Sciences, University of KwaZulu-Natal, Durban 4001, South Africa 7 4 CIBER-BBN, Networking Centre on Bioengineering, Biomaterials and Nanomedicine, University of 8 Barcelona, 08028 Barcelona, Spain 9 5 Department of Organic Chemistry, University of Barcelona, 08028 Barcelona, Spain 10 * Correspondence: [email protected]; [email protected]; Tel.: +27-614009144 11 12 13 Abstract: 2017 was an excellent year in terms of new drugs (chemical entities and biologics) 14 approved by the FDA, with a total of forty-six. In turn, one of the highlights was the number of 15 peptides (six) included in this list. Here, the six peptides are analysed in terms of chemical structure, 16 synthetic strategy used for their production, source, biological target, and mode of action. 17 Keywords: pharmaceutical market; drugs; drug discovery; solid-phase peptide synthesis 18 Introduction 19 The financial investment associated with the pharmaceutical industry is one of the largest in the 20 industrial sector—surpassed only by the telecommunications sector. However, the number of new 21 products (drugs) entering the market each year is relatively low.