Dana Alrafaiah
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Female Perineum Doctors Notes Notes/Extra Explanation Please View Our Editing File Before Studying This Lecture to Check for Any Changes
Color Code Important Female Perineum Doctors Notes Notes/Extra explanation Please view our Editing File before studying this lecture to check for any changes. Objectives At the end of the lecture, the student should be able to describe the: ✓ Boundaries of the perineum. ✓ Division of perineum into two triangles. ✓ Boundaries & Contents of anal & urogenital triangles. ✓ Lower part of Anal canal. ✓ Boundaries & contents of Ischiorectal fossa. ✓ Innervation, Blood supply and lymphatic drainage of perineum. Lecture Outline ‰ Introduction: • The trunk is divided into 4 main cavities: thoracic, abdominal, pelvic, and perineal. (see image 1) • The pelvis has an inlet and an outlet. (see image 2) The lowest part of the pelvic outlet is the perineum. • The perineum is separated from the pelvic cavity superiorly by the pelvic floor. • The pelvic floor or pelvic diaphragm is composed of muscle fibers of the levator ani, the coccygeus muscle, and associated connective tissue. (see image 3) We will talk about them more in the next lecture. Image (1) Image (2) Image (3) Note: this image is seen from ABOVE Perineum (In this lecture the boundaries and relations are important) o Perineum is the region of the body below the pelvic diaphragm (The outlet of the pelvis) o It is a diamond shaped area between the thighs. Boundaries: (these are the external or surface boundaries) Anteriorly Laterally Posteriorly Medial surfaces of Intergluteal folds Mons pubis the thighs or cleft Contents: 1. Lower ends of urethra, vagina & anal canal 2. External genitalia 3. Perineal body & Anococcygeal body Extra (we will now talk about these in the next slides) Perineum Extra explanation: The perineal body is an irregular Perineal body fibromuscular mass. -

Unit #2 - Abdomen, Pelvis and Perineum
UNIT #2 - ABDOMEN, PELVIS AND PERINEUM 1 UNIT #2 - ABDOMEN, PELVIS AND PERINEUM Reading Gray’s Anatomy for Students (GAFS), Chapters 4-5 Gray’s Dissection Guide for Human Anatomy (GDGHA), Labs 10-17 Unit #2- Abdomen, Pelvis, and Perineum G08- Overview of the Abdomen and Anterior Abdominal Wall (Dr. Albertine) G09A- Peritoneum, GI System Overview and Foregut (Dr. Albertine) G09B- Arteries, Veins, and Lymphatics of the GI System (Dr. Albertine) G10A- Midgut and Hindgut (Dr. Albertine) G10B- Innervation of the GI Tract and Osteology of the Pelvis (Dr. Albertine) G11- Posterior Abdominal Wall (Dr. Albertine) G12- Gluteal Region, Perineum Related to the Ischioanal Fossa (Dr. Albertine) G13- Urogenital Triangle (Dr. Albertine) G14A- Female Reproductive System (Dr. Albertine) G14B- Male Reproductive System (Dr. Albertine) 2 G08: Overview of the Abdomen and Anterior Abdominal Wall (Dr. Albertine) At the end of this lecture, students should be able to master the following: 1) Overview a) Identify the functions of the anterior abdominal wall b) Describe the boundaries of the anterior abdominal wall 2) Surface Anatomy a) Locate and describe the following surface landmarks: xiphoid process, costal margin, 9th costal cartilage, iliac crest, pubic tubercle, umbilicus 3 3) Planes and Divisions a) Identify and describe the following planes of the abdomen: transpyloric, transumbilical, subcostal, transtu- bercular, and midclavicular b) Describe the 9 zones created by the subcostal, transtubercular, and midclavicular planes c) Describe the 4 quadrants created -

Pelvic Diaphragm, Pelvic Floor Levator
Clinical topographic anatomy 2017/2018 Pelvis, perineal region Miloš Grim Institute of Anatomy, First Faculty of Medicine, Charles University PELVIS Bony pelvis, external measurements Pelvic planes and their measurements Pelvic floor muscles in relation to childbirth Uterine tubes and ovaries Female endopelvic fascias, ligaments supporting uterus, uterine prolapse Nerve blocks of the perineum (pudendal and ilioinguinal) Mechanisms of urinary continence Peritoneum and the female pelvis Peritoneum and the male pelvis Syntopy of the prostate, per rectum examination Syntopy of the rectum, per rectum examination Blood supply of pelvic viscera Perineum and episiotomy Bony pelvis, external measurements Pelvic planes and their measurements Pelvis types in women: A. Gynoid type (frequency 40%) B. Android type (frequency 30%) C.Anthropoid type (frequency 20%). D. Platypelloid type (frequency 3%). Vascular space Muscular space Obturatory canal infrapiriform foramen suprapiriform foramen Pelvic floor muscles in relation to childbirth, Female endopelvic fascia, Pelvic diaphragm, pelvic floor Levator ani pubic part – pubococcygeus (pubovisceral) pubovaginal puboprostatic puboperineal pubo-analis – puborectal iliac part – iliococcygeus Coccygeus – ischiococcygeus anococcygeal body, tendinous arch of levator ani, perineal body, urogenital hiatus, anal hiatus Levator ani muscle and parts of external anal sphincter (9): deep part (10), superficial part (11), subcutaneous part (12) Levator ani Tendinous arch of levator ani Tendinous arch of endopelvic fascia -

Female Perineum and External Genitalia
Female Perineum and External Genitalia Drs. Sanaa Alshaarawy & Saeed Vohra OBJECTIVES • At the end of the lecture, the student should be able to describe the: • Boundaries of the perineum. • Division of perineum into two triangles. • Boundaries & Contents of anal & urogenital triangles. • Lower part of Anal canal. • Boundaries & contents of Ischiorectal fossa. • Innervation, Blood supply and lymphatic drainage of perineum. Perineum • Perineum is the region of the body below the pelvic diaphragm (The outlet of the pelvis) • It is a diamond shaped area between the thighs • Boundaries: • Anteriorly Mons pubis • Laterally Medial surfaces of the thighs • Posteriorly Intergluteal folds • Contents: Perineal body • Lower ends of urethra, vagina & anal canal • External genitalia • Perineal body & Anococcygeal body Perineal Body • Perineal body is an irregular fibromuscular mass of variable size and consistency, located at midpoint of the line between the ischial tuberosities • Lies in the subcutaneous tissue, posterior to vaginal vestibule and anterior to the anal canal & anus • Forms the central point of the perineum & blends anteriorly with the perineal membrane Function: • Gives attachment to perineal muscles • Plays an important role in Perineal membrane visceral support especially in female Anococcygeal Body • The anococcygeal body is a complex musculotendinous structure • Situated between the anterior aspect of the coccyx and the posterior wall of the anorectal canal • Receives insertion of fibers of levator ani muscle Boundaries & Division of Perineum Boundaries: • Its bony boundaries are: • Anterior: Symphysis pubis. • Posterior: Coccyx. • Lateral: Ischiopubic rami, ischial tuberosities & sacrotuberous ligaments. Division: • By an imaginary line passing through two ischial tuberosities, it is divided into: ▪ Urogenital triangle anteriorly. ▪ Anal triangle posteriorly. -

Anatomy Pelvic Floor & Colorectal
I ANATOMY PELVIC FLOOR & COLORECTAL OVERVIEW Definition of pelvic floor From genitalia to organs, superior endopelvic supportive tissues 3 layers of muscle, different muscles within each layer Intervening layers of fascia surrounding each muscle Fascial thickening = ligaments Endopelvic connective tissue surrounding all viscera Functions of pelvic floor Support of the organs Sphincteric of the outlets (urethra, vagina, rectum) and openings (meatus, introitus, anus) Sexual – providing tone for the vaginal and rectal canals Stabilization “Sump Pump” Lymphatic Terminology Confusing as to what specific anatomical reference Different disciplines emphasize different structures Changing – pubococcygeus is now the pubovesical Mobility versus stability concept Organs and outlets need to expand and be mobile Too much mobility is prolapse or incontinence Too much fixation/stability is painful The concept of organ mobility and stability is key to understanding dysfunctions of the pelvic floor. The organs are sacs that are meant to move, expand and empty. This is true for the bladder, uterus, vagina, rectum and colon. Should they not be able to expand fully because of fibrotic attachments, endometrial adhesions, tissue changes or scarring from surgery, the patient may present with symptoms of pressure, pain, constipation, urinary frequency, dyspareunia, urethral syndrome, to name but a few. Should the organs not be stabilized in their proper positions because of weakened or torn muscles and ligaments, problems such as prolapse, perineal pressure, -

The Pelvic Floor
The Pelvic Floor By Dr.Mazenah Objectives At the end of this lecture the student should be able to : Describe the structure and function of the pelvic floor and name the main muscle groups Describe the function of the perineal body Describe the main types of pelvic floor dysfunction List the causes of and risk factors for pelvic floor dysfunction Describe in outline the treatments available for pelvic floor dysfunction The pelvic floor is formed from muscular layer(s) which support the pelvic viscera. It exerts a sphincter action on rectum and vagina and can resist increases in intra-abdominal pressure associated with coughing, defecation, heavy lifting etc. Damage to pelvic floor (e.g. as a consequence to childbirth leads to stress urinary incontinence & fecal incontinence..etc. The pelvic floor is composed of A. Pelvic diaphragm Bowl, or funnel, shaped consisting of: 1. levator ani 2. coccygeus, and 3. related fascial coverings B. Superficial muscles and structures ) 1. anterior (urogenital) perineum 2. posterior (anal) perineum The pelvic diaphragm lies within the lesser pelvis, separating the pelvic cavity from the perineum. •Levator ani are paired muscles forming 3 slings of muscle extending from the posterior aspect of pubic bone, the fascia over obturator internus and the ischial spines The 3 slings of levator ani are: 1. anterior fibres anteriorly sling around prostate (levator prostatae ) in male or vagina in female (Pubovaginalis) 2. intermediate fibres around rectum (puborectalis) and into anococcygeal body (pubococcygeus) -

Pelvic Wall Joints of the Pelvis Pelvic Floor
ANATOMY OF THE PELVIS Prof. Saeed Abuel Makarem OBJECTIVES • By the end of the lecture, you should be able to: • Describe the anatomy of the pelvis regarding (bones, joints & muscles). • Describe the boundaries and subdivisions of the pelvis. • Differentiate the different types of the female pelvis. • Describe the pelvic walls & floor. • Describe the components & function of the pelvic diaphragm. • List the blood & nerves & lymphatic of the pelvis. The bony pelvis is composed of four bones: • Two hip bones, which form the anterior and lateral walls. • Sacrum and coccyx, which form the posterior wall. • These 4 bones are lined by 4 muscles and connected by 4 joints. • The bony pelvis with its joints and muscles form a strong basin-shaped structure (with multiple foramina), that contains & protects the lower parts of the alimentary & urinary tracts and internal organs of reproduction. 3 FOUR JOINTS 1- Anteriorly: Symphysis pubis (2nd cartilaginous joint). 2- Posteriorlateraly: Two Sacroiliac joints. (Synovial joins) 3- Posteriorly: Sacrococcygeal joint (cartilaginous), between sacrum and coccyx. 4 The pelvis is divided into two parts by the pelvic brim. Above the brim is the False or greater pelvis, which is part of the abdominal cavity. Pelvic Below the brim is the True or brim lesser pelvis. The False pelvis is bounded by: Posteriorly: Lumbar vertebrae. Laterally: Iliac fossae and the iliacus. Anteriorly: Lower part of the anterior abdominal wall. It supports the abdominal contents. 5 The True pelvis has: • An Inlet. • An Outlet. and a Cavity. The cavity is a short, curved canal, with a shallow anterior wall and a deeper posterior wall. -

A Beginners Look Into Pelvic Physical Therapy
THE LAND DOWN UNDER Presented by: Karla Giramonti MS FNP With support from Carin Cappadocia, PT, DPT DISCLOSURE In the past 12 months, I have not had a significant financial interest or other relationship with the manufacturer(s) of the product(s) or provider(s) of the service(s) that will be discussed in my presentation. This presentation will not include discussion of pharmaceuticals or devices that have not been approved by the FDA or if you will be discussing unapproved or “off-label” uses of pharmaceuticals or devices. WHAT IS THE PELVIC FLOOR? “All visceral, neurovascular, and myofascial structures contained in the bony pelvis from pubis to coccyx and between lateral ischial walls” – APTA SOWH FUNCTION OF THE PELVIC FLOOR MUSCLES 1. Support 2. Sphincteric 3. Sexual 4. Trunk and Pelvic Stabilization 5. Lymphatic PELVIC GIRDLE aka BONEY LANDMARKS http://classconnection.s3.amazonaws.com/551/flashcards/1673551/png/sc reen_shot_2014-03-07_at_40412_pm-1449E5C571029BC2ABD.png FIRST LAYER PELVIC FLOOR MUSCLES • Ischiocavernosus (S2,3,4) • Superficial Transverse Perineal • O: Ischial tuberosity and ramus Muscle (S2,3,4) • I: Inferolateral apponeurosis over • O: Ischial Tuberosity cura of clitoris/penis • I: Central perineal tendon/Perineal • A: Erection (clitoral, penile) Body • Bulbocavernosus/Bulbospongios • A: Pelvic Floor Stability us (S2,3,4) • External Anal Sphincter • O: Central perineal tendon, • O: Perineal Body (F) Palpable under • I: Partial coccyx and surrounds anal labia canal (M) Midline Scrotum • A: Voluntary opening of anal -
1. Relations & Boundaries
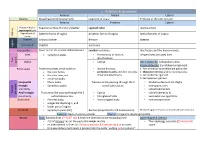
1. Relations & boundaries Anterior Medial Lateral Ovaries Broad ligament (mesovarium) Ligament of ovary Fimbriae of the uterine tube Anterior Posterior Lateral Fundus + body + Superior surface of urinary bladder sigmoid colon uterine artery supravaginal part Vaginal part of Anterior fornix of vagina posterior fornix of vagina lateral fornices of vagina Uterus cervix In pelvis Urinary bladder Rectum Ureters In perineum Urethra anal canal vagina False pelvis Lower part of the anterior abdominal wall. Lumbar vertebrae. Iliac fossae and the iliacus muscle. Inlet symphysis pubis. • Promontory of sacrum, Ileopectineal (arcuate) lines. • ala of sacrum. True True pelvis Outlet • Coccyx Anterolaterally: ischiopubic ramus Posterolaterally: Sacrotuberous ligament. Pelvic walls Posterior surfaces of the bodies of: • Sacrum & coccyx, 1- Part of the hip bone below the pelvic inlet the pubic bones, • piriformis muscles and their covering 2- Obturator internus and its covering fascia the pubic rami, and of parietal pelvic fascia. 3- Sacrotuberous ligament. symphysis pubis. 4- Sacrospinous ligament. Urogenital • Mons pubis Transverse line passing through the 2 • Medial surfaces of the thighs triangle • Symphysis pubis. ischial tuberosities. • Ischiopubic rami, anteriorly. • ischial tuberosities Female • • perineum Anal triangle Transverse line passing through the 2 Coccyx ischial tuberosity & posteriorly. ischial tuberosities. • Intergluteal folds • sacrotuberous ligaments. Anal canal • Perineal body, • Anococcygeal body. • Ischiorectal fossae. • urogenital diaphragm, and • lower part of vagina Prostate • Symphysis pubis (SP). Rectum (important for PR Examination) Medial margins of levator ani muscles (levator prostate) Superior: Neck of urinary bladder. Inferior: Urogenital diaphragm (UGD). Breast Base: Extends from 2nd to 6th ribs & from the sternum to the midaxillary line Apex (Nipple & Areola) • 2/3 of its base lies on the pectoralis major muscle • The nipple lies opposite 4th intercostal • its inferolateral 1/3 lies on: Serratus anterior & External oblique muscles. -

Chapter 1: Clinical Anatomy of the Pelvis and Reproductive Tract
Chapter 1: Clinical anatomy of the pelvis and reproductive tract Alan Farthing Introduction structures on the anterior abdominalwallare: T7 xiphisternum This chapter aims to summarize the important aspects of T10 umbilicus the anatomy of the abdomen and the pelvis, which should L1 symphysis pubis be known to the Obstetric or Gynaecological specialist. The blood supply is via the superior epigastric (branch Many of the investigations and treatments we order on a of the internalthoracic artery) and the inferior epigas- daily basis require good anatomical knowledge in order tric (branch of the external iliac artery) vessels. During to be properly understood. laparoscopy, the inferior epigastric vessels can be seen between the peritoneum and rectus muscle on the anterior Surface anatomy abdominalwallandcommence their journey superiorly from approximately two thirds of the way along the The anterior abdominalwallcanbe divided into four inguinal ligament closer to the symphysis pubis. Care quadrants by lines passing horizontally and vertically needs to be taken to avoid them while using acces- through the umbilicus (Fig. 1.1). In the upper abdomen sory trochars during laparoscopy and to ensure that they is the epigastrium, which is the area just inferior to the are identified when making a Maylard incision of the xiphisternum, and in the lower abdomen lie the right and abdominal wall. left iliac fossae and the hypogastrium. The cutaneous nerve supply of the anterior abdominal wall arises from the anterior rami of the lower thoracic The anterior abdominal wall and lumbar vertebrae. The dermatomes of significant Beneath the skin and the fat of the superficialanterior abdominalwallliesa sheath and combination of mus- cles including the rectus abdominus, external and internal oblique and tranversalis muscles (Fig. -

A Clinical Study on the Efficacy of Homeopathic Remedies in Bleeding Haemorrhoids
©www.similima.com A Clinical study on the Efficacy of Homeopathic Remedies in Bleeding Haemorrhoids Dr. Thanka.R Acknowledgement “Ex nihilo nihil fit” out of nothing, nothing comes except Him, the Alpha and the Omega, the Prime Mover, who is the sum and substance of every being. It is He who has ordained me to part take of the divine task of the healing power. The physician prescribes the medicine but He administers the healing. I offer my very being in thanks giving to the Almighty for making me add my simple string to the divine lute of curing through this work of mine. Next to God, I would like to thank my mother and father for enabling me to become a drop in the ocean of the mystery and the miracle of Homoeopathic practice and contribute my own little might to the saga of Homoeopathic theory and practice through this maiden work. Without a devoted teacher no disciple ever achieved anything. A sincere teacher moulds the mettle and calibre of the students given to her care. I render my heartfelt gratitude and sincere appreciation to my teacher and guide Dr. Aleyamma Thomas, without whose timely guidance, scholarly deliberations and patient discussions, my work would not have been successfully completed. I would like to extend my sincere thanks to Dr. Abdul Rahman, the Principal, Government Homoeopathic Medical College, Thiruvananthapuram for his overall supervision. A special word of appreciation and gratitude to Dr.Jaya, the Superintendent, Government Homoeopathic Medical College Hospital, Thiruvananthapuram for her guidance and support. My cordial thanks to Dr. -

Female Perineum and External Genitalia
Female Perineum and External Genitalia By : Associate Prof. Sanaa Alshaarawy & OBJECTIVES • At the end of the lecture, the student should be able to describe the: • Boundaries of the perineum. • Division of perineum into two triangles. • Boundaries & Contents of anal & urogenital triangles. • Lower part of Anal canal. • Boundaries & contents of Ischiorectal fossa. • Innervation, Blood supply and lymphatic drainage of perineum. Perineum • Perineum is the region of the body below the pelvic diaphragm (The outlet of the pelvis) • It is a diamond shaped area between the thighs • Boundaries: • Anteriorly Mons pubis • Laterally Medial surfaces of the thighs • Posteriorly Intergluteal folds • Contents: Perineal body • Lower ends of urethra, vagina & anal canal • External genitalia • Perineal body & Anococcygeal body Perineal Body • Perineal body is an irregular fibromuscular mass of variable size and consistency, located at midpoint of the line between the ischial tuberosities • Lies in the subcutaneous tissue, posterior to vaginal vestibule and anterior to the anal canal & anus • Forms the central point of the perineum & blends anteriorly with the perineal membrane Function: • Gives attachment to perineal muscles • Plays an important role in Perineal membrane visceral support especially in female Anococcygeal Body • The anococcygeal body is a complex musculotendinous structure • Situated in the floor of pelvis between the coccyx and the posterior wall of the anal canal • Receives insertion of fibers of levator ani muscle Boundaries & Division of Perineum Boundaries: • Its bony boundaries are: • Anterior: Symphysis pubis. • Posterior: Coccyx. • Lateral: Ischiopubic rami, ischial tuberosities & sacrotuberous ligaments. Division: • By an imaginary line passing through two ischial tuberosities, it is divided into: § Urogenital triangle anteriorly. § Anal triangle posteriorly.