Dermoscopy in Viral Infections: an Observational Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Picture of the Month
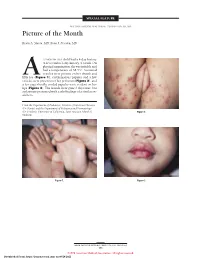
SPECIAL FEATURE SECTION EDITOR: WALTER W. TUNNESSEN, JR, MD Picture of the Month Kevin A. Slavin, MD; Ilona J. Frieden, MD 15-MONTH-OLD child had a 4-day history of fever and a 1-day history of a rash. On physical examination she was irritable and had a temperature of 38.3°C. Scattered vesicles were present on her thumb and Afifth toe (Figure 1), erythematous papules and a few vesicles were present over her perineum (Figure 2), and a few superficially eroded papules were evident on her lips (Figure 3). The lesions were gone 3 days later, but a playmate presented with early findings of a similar ex- anthem. From the Department of Pediatrics, Division of Infectious Diseases (Dr Slavin) and the Department of Pediatrics and Dermatology (Dr Frieden), University of California, San Francisco School of Figure 2. Medicine. Figure 1. Figure 3. ARCH PEDIATR ADOLESC MED/ VOL 152, MAY 1998 505 ©1998 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 09/28/2021 Denouement and Discussion Hand-Foot-and-Mouth Disease Figure 1. Vesicles are present on the thumb and fifth toe. foot-and-mouth disease).1,2,5-9 The lesions on the but- tocks are of the same size and typical of the early forms Figure 2. Multiple erythematous papules and a few scattered vesicles are of the exanthem, but they are not frequently vesicular present over the perineum. in nature. Lesions involving the perineum seem to be more Figure 3. Superficially eroded papules are present on the lips. common in children who wear diapers, suggesting that friction or minor trauma may play a role in the develop- ment of lesions. -

Chapter 3 Bacterial and Viral Infections
GBB03 10/4/06 12:20 PM Page 19 Chapter 3 Bacterial and viral infections A mighty creature is the germ gain entry into the skin via minor abrasions, or fis- Though smaller than the pachyderm sures between the toes associated with tinea pedis, His customary dwelling place and leg ulcers provide a portal of entry in many Is deep within the human race cases. A frequent predisposing factor is oedema of His childish pride he often pleases the legs, and cellulitis is a common condition in By giving people strange diseases elderly people, who often suffer from leg oedema Do you, my poppet, feel infirm? of cardiac, venous or lymphatic origin. You probably contain a germ The affected area becomes red, hot and swollen (Ogden Nash, The Germ) (Fig. 3.1), and blister formation and areas of skin necrosis may occur. The patient is pyrexial and feels unwell. Rigors may occur and, in elderly Bacterial infections people, a toxic confusional state. In presumed streptococcal cellulitis, penicillin is Streptococcal infection the treatment of choice, initially given as ben- zylpenicillin intravenously. If the leg is affected, Cellulitis bed rest is an important aspect of treatment. Where Cellulitis is a bacterial infection of subcutaneous there is extensive tissue necrosis, surgical debride- tissues that, in immunologically normal individu- ment may be necessary. als, is usually caused by Streptococcus pyogenes. A particularly severe, deep form of cellulitis, in- ‘Erysipelas’ is a term applied to superficial volving fascia and muscles, is known as ‘necrotiz- streptococcal cellulitis that has a well-demarcated ing fasciitis’. This disorder achieved notoriety a few edge. -

A. Syphilis Is a Systemic, Sexually Transmitted Disease (STD) Caused by the Treponema Pallidum Bacterium
Oklahoma State Department of Health 03-2018 Revised SYPHILIS I. DEFINITION: A. Syphilis is a systemic, sexually transmitted disease (STD) caused by the Treponema pallidum bacterium. B. It can cause long-term complications if not treated correctly. Symptoms in adults are divided into stages. These stages are described below in the Clinical Features. Syphilis has been called ‘the great imitator’ because it has so many possible symptoms, many of which look like symptoms from other diseases. The painless syphilis chancre that clients get after they are first infected can be confused for an ingrown hair, zipper cut, or other seemingly harmless bump. Many times the client does not know they had a sore. The non-itchy body rash that develops during the second stage of syphilis can show up on the palms of the client’s hands and soles of their feet, all over the body, or in just a few places. The rash is usually bilateral, meaning it appears equally on both sides of the body. C. The three means of syphilis transmission are: 1. Person to person via vaginal, anal, or oral sex through direct contact with a syphilis chancre. 2. Person to person during foreplay, even when there is no penetrative sex (much less common). 3. Pregnant mother with syphilis to fetus - very serious complications may occur (fetal demise, long bone deformities, “saddle nose”). II. CLINICAL FEATURES: If left untreated, the disease progresses through several stages during which the infected person may or may not be symptomatic. The DIS and ‘Syphilis Diagnosis and Treatment Algorithm’ (Appendix 1) can assist with staging. -

Hand, Foot, and Mouth Disease (Coxsackievirus) Fact Sheet
Hand, Foot, and Mouth Disease (Coxsackievirus) Fact Sheet Hand, foot, and mouth disease is caused by one of several types of viruses Hand, foot, and mouth disease is usually characterized by tiny blisters on the inside of the mouth and the palms of the hands, fingers, soles of the feet. It is commonly caused by coxsackievirus A16 (an enterovirus), and less often by other types of viruses. Anyone can get hand, foot, and mouth disease Young children are primarily affected, but it may be seen in adults. Most cases occur in the summer and early fall. Outbreaks may occur among groups of children especially in child care centers or nursery schools. Symptoms usually appear 3 to 5 days after exposure. Hand, foot, and mouth disease is usually spread through person-to-person contact People can spread the disease when they are shedding the virus in their feces. It is also spread by the respiratory tract from mouth or respiratory secretions (such as from saliva on hands or toys). The virus has also been found in the fluid from the skin blisters. The infection is spread most easily during the acute phase/stage of illness when people are feeling ill, but the virus can be spread for several weeks after the onset of infection. The symptoms are much like a common cold with a rash The rash appears as blisters or ulcers in the mouth, on the inner cheeks, gums, sides of the tongue, and as bumps or blisters on the hands, feet, and sometimes other parts of the skin. The skin rash may last for 7 to 10 days. -

Condylomata Acuminata of the Penis and Scrotum Case Report and Literature Review
World Journal of Research and Review (WJRR) ISSN:2455-3956, Volume-8, Issue-1, January 2019 Pages 07-09 Condylomata Acuminata of the Penis and Scrotum Case Report and Literature Review Otei Otei O. O, Ozinko M, Ekpo R, Egiehiokhin Isiwere, Nabie N.F same Hospital with a histological diagnosis of Abstract— The case of an affected 36-year old male and Condylomata Acuminata following a history of multiple review of relevant literature which utilize to highlight the scrotal and penile swellings of 10 year duration and the diagnostic and management challenges of this case. The patient challenges faced in the management of the condition. was initially received medical treatment at the Dermatology CASE REPORT Clinic of the University Calabar. The latter was not successful and the patient was referred to the Burns and Plastic Surgery A 36 year old married Driver was referred from Unit of the same hospital where scrotal sac excision, flap cover dermatology clinic to the Surgical outpatient Department of and electrocautery were done. This treatment was successful the University of Calabar Teaching Hospital, Calabar with a but there was mild penile contracture and we intend to follow histological diagnosis of Condylomata Acuminata of the up patient closely for early detection and treatment of Penis and Scrotum following a history of multiple recurrence. peno-scrotal swellings of 10 years duration. BACKGROUND A swelling was first noticed as a hard painful boil on his Condylomata Acuminata or genital wart refers to the epidermal manifestation attributed to the epidermotropic left inguinal region . Multiple swellings appeared in the same Human Papiloma Virus (HPV) particularly types 6 and 11 . -

Treatment of Warts with Topical Cidofovir in a Pediatric Patient
Volume 25 Number 5| May 2019| Dermatology Online Journal || Case Report 25(5):6 Treatment of warts with topical cidofovir in a pediatric patient Melissa A Nickles BA, Artem Sergeyenko MD, Michelle Bain MD Affiliations: Department of Dermatology, University of Illinois at Chicago College of Medicine, Chicago, llinois, USA Corresponding Author: Artem Sergeyenko MD, 808 South Wood Street Suite 380, Chicago, IL 60612, Tel: 847-338-0037, Email: a.serge04@gmail topical cidofovir is effective in treating HPV lesions Abstract and molluscum contagiosum in adult patients with Cidofovir is an antiviral nucleotide analogue with HIV/AIDS [2]. Case reports have also found topical relatively new treatment capacities for cidofovir to effectively treat anogenital squamous dermatological conditions, specifically verruca cell carcinoma (SCC), bowenoid papulosis, vulgaris caused by human papilloma virus infection. condyloma acuminatum, Kaposi sarcoma, and HSV-II In a 10-year old boy with severe verruca vulgaris in adult patients with HIV/AIDS [3]. Cidofovir has recalcitrant to multiple therapies, topical 1% experimentally been shown to be effective in cidofovir applied daily for eight weeks proved to be an effective treatment with no adverse side effects. treating genital condyloma acuminata in adult This case report, in conjunction with multiple immunocompetent patients [4] and in a pediatric published reports, suggests that topical 1% cidofovir case [5]. is a safe and effective treatment for viral warts in Cidofovir has also been used in pediatric patients to pediatric patients. cure verruca vulgaris recalcitrant to traditional treatment therapies. There have been several reports Keywords: cidofovir, verruca vulgaris, human papilloma that topical 1-3% cidofovir cream applied once or virus twice daily is effective in treating verruca vulgaris with no systemic side effects and low rates of recurrence in immunocompetent children [6-8], as Introduction well as in immunocompromised children [9, 10]. -

Designing and Evaluating a Health Belief Model Based Intervention to Increase Intent of HPV Vaccination Among College Men: Use of Qualitative and Quantitative Methodology
Designing and evaluating a health belief model based intervention to increase intent of HPV vaccination among college men: Use of qualitative and quantitative methodology A dissertation submitted to the Graduate School of the University of Cincinnati In partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY In the School of Human Services of the College of Education, Criminal Justice, and Human Services 2012 by Purvi Mehta MS, University of Cincinnati Committee Chair: Manoj Sharma, M.B.; B.S., MCHES, Ph.D Abstract Humanpapilloma virus (HPV) is a common sexually transmitted disease/infection (STD/STI), leading to cervical and anal cancers. Annually, 6.2 million people are newly diagnosed with HPV and 20 million currently are diagnosed. According to the Centers for Disease Control and Prevention, 51.1% of men carry multiple strains of HPV. Recently, HPV vaccine was approved for use in boys and young men to help reduce the number of HPV cases. Currently limited research is available on HPV and HPV vaccination in men. The purpose of the study was to determine predictors of HPV vaccine acceptability among college men through the qualitative approach of focus groups and to develop an intervention to increase intent to seek vaccination in the target population The study took place in two phases. During Phase I, six focus groups were conducted with 50 participants. In Phase II using a randomized controlled trial a HBM based intervention was compared with a traditional knowledge based intervention in 90 college men. In Phase I lack of perceived susceptibility, perceived severity of HPV and barriers towards taking the HPV vaccine were major themes identified from the focus groups. -

A Guide to Clinical Management and Public Health Response for Hand, Foot and Mouth Disease (HFMD)
A Guide to Clinical Management and Public Health Response for Hand, Foot and Mouth Disease (HFMD) WHO Western Pacific Region PUBLICATION ISBN-13 978 92 9061 525 5 A Guide to Clinical Management and Public Health Response for Hand, Foot and Mouth Disease (HFMD) WHO Library Cataloguing in Publication Data A Guide to clinical management and public health response for hand, foot and mouth disease (HFMD) 1. Hand, foot and mouth disease – epidemiology. 2. Hand, foot and mouth disease – prevention and control. [ ii ] 3. Disease outbreaks. 4. Enterovirus A, Human. I. Regional Emerging Disease Intervention Center. ISBN 978 92 9061 525 5 (NLM Classification: WC 500) © World Health Organization 2011 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: [email protected]). For WHO Western Pacific Regional Publications, request for permission to reproduce should be addressed to the Publications Office, World Health Organization, Regional Office for the Western Pacific, P.O. Box 2932, 1000, Manila, Philippines, (fax: +632 521 1036, e-mail: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. -

Fundamentals of Dermatology Describing Rashes and Lesions
Dermatology for the Non-Dermatologist May 30 – June 3, 2018 - 1 - Fundamentals of Dermatology Describing Rashes and Lesions History remains ESSENTIAL to establish diagnosis – duration, treatments, prior history of skin conditions, drug use, systemic illness, etc., etc. Historical characteristics of lesions and rashes are also key elements of the description. Painful vs. painless? Pruritic? Burning sensation? Key descriptive elements – 1- definition and morphology of the lesion, 2- location and the extent of the disease. DEFINITIONS: Atrophy: Thinning of the epidermis and/or dermis causing a shiny appearance or fine wrinkling and/or depression of the skin (common causes: steroids, sudden weight gain, “stretch marks”) Bulla: Circumscribed superficial collection of fluid below or within the epidermis > 5mm (if <5mm vesicle), may be formed by the coalescence of vesicles (blister) Burrow: A linear, “threadlike” elevation of the skin, typically a few millimeters long. (scabies) Comedo: A plugged sebaceous follicle, such as closed (whitehead) & open comedones (blackhead) in acne Crust: Dried residue of serum, blood or pus (scab) Cyst: A circumscribed, usually slightly compressible, round, walled lesion, below the epidermis, may be filled with fluid or semi-solid material (sebaceous cyst, cystic acne) Dermatitis: nonspecific term for inflammation of the skin (many possible causes); may be a specific condition, e.g. atopic dermatitis Eczema: a generic term for acute or chronic inflammatory conditions of the skin. Typically appears erythematous, -

GET YOURSELF TESTED Testing Is Confidential
GET YOURSELF TESTED Testing is confidential. If you are under 18 years old, you can consent to be checked and treated for STIs. • Warts may grow on or around the genital area virus will still be in your body and you may still pass (penis, scrotum, vagina, vulva), the anus, or mouth. it during sex. They can also grow inside the body where they are hard to see. • Talk with your provider about when it’s safe to have • Usually are painless, but if the warts are injured, sex after getting treatment. they may become sore when touched. • It’s important to talk with your partner(s) about any sexually transmitted infections (STIs) you may have. Why Does It Matter? • Certain types of HPV can lead to cervical cancer in To Learn More females, or cancer of the penis in males. Some types of HPV may also lead to oral or anal cancer. Contact a health care provider or your local STI clinic. • In some cases, warts can become quite large and To learn more about STIs, or to find your local STI cause discomfort. clinic, visit www.health.ny.gov/STD. • A small percentage of pregnant people with You can find other STI testing locations at genital warts can pass the virus to the baby https://gettested.cdc.gov. during birth. Partners Because symptoms of HPV can take a long time to show up, if at all, it’s hard to know when a person first got it. • If you have genital warts, tell your partner(s) so they can be checked by a health care provider, and treated if they have them. -

Koi Herpesvirus Disease (KHVD)1 Kathleen H
VM-149 Koi Herpesvirus Disease (KHVD)1 Kathleen H. Hartman, Roy P.E. Yanong, Deborah B. Pouder, B. Denise Petty, Ruth Francis-Floyd, Allen C. Riggs, and Thomas B. Waltzek2 Introduction Koi herpesvirus (KHV) is a highly contagious virus that causes significant morbidity and mortality in common carp (Cyprinus carpio) varieties (Hedrick et al. 2000, Haenen et al. 2004). Common carp is raised as a foodfish in many countries and has also been selectively bred for the ornamental fish industry where it is known as koi. The first recognized case of KHV occurred in the United Kingdom in 1996 (Haenen et al. 2004). Since then other cases have been confirmed in almost all countries that culture koi and/ or common carp with the exception of Australia (Hedrick et al. 2000; Haenen et al. 2004, Pokorova et al. 2005). This information sheet is intended to inform veterinarians, biologists, fish producers and hobbyists about KHV disease. What Is KHV? Figure 1. Koi with mottled gills and sunken eyes due to koi Koi herpesvirus (also known as Cyprinid herpesvirus 3; herpesvirus disease. Credit: Deborah B. Pouder, University of Florida CyHV3) is classified as a double-stranded DNA virus herpesvirus, based on virus morphology and genetics, and belonging to the family Alloherpesviridae (which includes is closely related to carp pox virus (Cyprinid herpesvirus fish herpesviruses). The work of Waltzek and colleagues 1; CyHV1) and goldfish hematopoietic necrosis virus (Waltzek et al. 2005, 2009) revealed that KHV is indeed a (Cyprinid herpesvirus 2; CyHV2). Koi herpesvirus disease has been diagnosed in koi and common carp (Hedrick 1. -
Guidelines for Occupational Health Follow up of Communicable Diseases for Manager/Supervisors
Winnipeg Regional Health Authority Occupational and Environmental Safety & Health (OESH) Guidelines for Occupational Health Follow Up of Communicable Diseases For Manager/Supervisors Page | 1 2019.02.04 version 2 Winnipeg Regional Health Authority Occupational and Environmental Safety & Health (OESH) INTRODUCTION ................................................................................................................................................................................. 3 WORKERS COMPENSATION BOARD (WCB) CLAIMS ........................................................................................................................... 5 ANTIBIOTIC RESISTANT ORGANISMS (AROS) ..................................................................................................................................... 6 BLOOD AND BODY FLUID EXPOSURES ............................................................................................................................................... 9 CIMEX LECTULARIUS (BED BUGS) .................................................................................................................................................... 10 CREUTZFELDT-JAKOB DISEASE (CJD) ................................................................................................................................................ 11 DIARRHEA (BACTERIAL, CLOSTRIDIUM DIFFICILE (C. DIFFICILE), VIRAL) ........................................................................................... 12 GROUP A STREPTOCOCCUS ............................................................................................................................................................