Clinical Syndromes/Conditions with Required Level Or Precautions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Picture of the Month
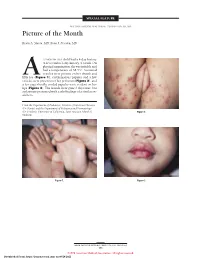
SPECIAL FEATURE SECTION EDITOR: WALTER W. TUNNESSEN, JR, MD Picture of the Month Kevin A. Slavin, MD; Ilona J. Frieden, MD 15-MONTH-OLD child had a 4-day history of fever and a 1-day history of a rash. On physical examination she was irritable and had a temperature of 38.3°C. Scattered vesicles were present on her thumb and Afifth toe (Figure 1), erythematous papules and a few vesicles were present over her perineum (Figure 2), and a few superficially eroded papules were evident on her lips (Figure 3). The lesions were gone 3 days later, but a playmate presented with early findings of a similar ex- anthem. From the Department of Pediatrics, Division of Infectious Diseases (Dr Slavin) and the Department of Pediatrics and Dermatology (Dr Frieden), University of California, San Francisco School of Figure 2. Medicine. Figure 1. Figure 3. ARCH PEDIATR ADOLESC MED/ VOL 152, MAY 1998 505 ©1998 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 09/28/2021 Denouement and Discussion Hand-Foot-and-Mouth Disease Figure 1. Vesicles are present on the thumb and fifth toe. foot-and-mouth disease).1,2,5-9 The lesions on the but- tocks are of the same size and typical of the early forms Figure 2. Multiple erythematous papules and a few scattered vesicles are of the exanthem, but they are not frequently vesicular present over the perineum. in nature. Lesions involving the perineum seem to be more Figure 3. Superficially eroded papules are present on the lips. common in children who wear diapers, suggesting that friction or minor trauma may play a role in the develop- ment of lesions. -

NIH Medlineplus Magazine Winter 2010
Trusted Health Information from the National Institutes of Health ® NIHMedlineWINTER 2010 Plusthe magazine Plus, in this issue! • Treating “ Keep diverticulitis the beat” Healthy blood Pressure • Protecting Helps Prevent Heart disease Yourself from Shingles • Progress against Prostate cancer • Preventing Suicide in Young Adults • relieving the Model Heidi Klum joins The Heart Truth Pain of tMJ Campaign for women’s heart health. • The Real Benefits of Personalized Prevent Heart Medicine Disease Now! You can lower your risk. A publication of the NatioNal Institutes of HealtH and the frieNds of the NatioNal library of MediciNe FRIENDS OF THE NATIONAL LIBRARY OF MEDICINE Saying “Yes!” to Careers in Health Care ecently, the Friends of NLM was delighted to co-sponsor the fourth annual “Yes, I Can Be a Healthcare Professional” conference at Frederick Douglass Academy in Harlem. More than 2,300 students and parents from socioeconomically disadvantaged communities throughout the entire New York City metropolitan area convened for Rthe daylong session. It featured practical skills workshops, discussion groups, and exhibits from local educational institutions, health professional societies, community health services, and health information providers, including the National Library of Medicine (NLM). If you’ll pardon the expression, the enthusiasm among the attendees—current and future Photo: NLM Photo: healthcare professionals—was infectious! donald West King, M.d. fNlM chairman It was especially exciting to mix with some of the students from six public and charter high schools in Harlem and the South Bronx enrolled in the Science and Health Career Exploration Program. The program was created by Mentoring in Medicine, Inc., funded by the NLM and Let Us Hear co-sponsored by the Friends. -

Juvenile Recurrent Parotitis and Sialolithiasis: an Noteworthy Co-Existence
Otolaryngology Open Access Journal ISSN: 2476-2490 Juvenile Recurrent Parotitis and Sialolithiasis: An Noteworthy Co-Existence Venkata NR* and Sanjay H Case Report Department of ENT and Head & Neck Surgery, Kohinoor Hospital, India Volume 3 Issue 1 Received Date: April 20, 2018 *Corresponding author: Nataraj Rajanala Venkata, Department of ENT and Head & Published Date: May 21, 2018 Neck Surgery, Kohinoor Hospital, Kurla (W), Mumbai, India, Tel: +918691085580; DOI: 10.23880/ooaj-16000168 Email: [email protected] Abstract Juvenile Recurrent Parotitis is a relatively rare condition. Sialolithiasis co-existing along with Juvenile Recurrent Parotitis is an even rarer occurrence. We present a case of Juvenile Recurrent Parotitis and Sialolithiasis in a 6 years old male child and how we managed it. Keywords: Juvenile Recurrent Parotitis; Parotid gland; Swelling; Sialolithiasis Introduction child. Tuberculosis was suspected but the tests yielded no results. Even MRI of the parotid gland failed to reveal any Juvenile Recurrent Parotitis is characterized by cause. Then the patient was referred to us for definitive recurring episodes of swelling usually accompanied by management. Taking the history into consideration, a pain in the parotid gland. Associated symptoms usually probable diagnosis of Juvenile Recurrent Parotitis due to include fever and malaise. It is most commonly seen in sialectasis was considered. CT Sialography revealed children, but may persist into adulthood. Unlike parotitis, dilatation of the main duct and the ductules with which is caused by infection or obstructive causes like collection of the dye at the termination of the terminal calculi, fibromucinous plugs, duct stenosis and foreign ductules, in the left parotid gland. -

Kellie ID Emergencies.Pptx
4/24/11 ID Alert! recognizing rapidly fatal infections Susan M. Kellie, MD, MPH Professor of Medicine Division of Infectious Diseases, UNMSOM Hospital Epidemiologist UNMHSC and NMVAHCS Fever and…. Rash and altered mental status Rash Muscle pain Lymphadenopathy Hypotension Shortness of breath Recent travel Abdominal pain and diarrhea Case 1. The cross-country trucker A 30 year-old trucker driving from Oklahoma to California is hospitalized in Deming with fever and headache He is treated with broad-spectrum antibiotics, but deteriorates with obtundation, low platelet count, and a centrifugal petechial rash and is transferred to UNMH 1 4/24/11 What is your diagnosis? What is the differential diagnosis of fever and headache with petechial rash? (in the US) Tickborne rickettsioses ◦ RMSF Bacteria ◦ Neisseria meningitidis Key diagnosis in this case: “doxycycline deficiency” Key vector-borne rickettsioses treated with doxycycline: RMSF-case-fatality 5-10% ◦ Fever, nausea, vomiting, myalgia, anorexia and headache ◦ Maculopapular rash progresses to petechial after 2-4 days of fever ◦ Occasionally without rash Human granulocytotropic anaplasmosis (HGA): case-fatality<1% Human monocytotropic ehrlichiosis (HME): case fatality 2-3% 2 4/24/11 Lab clues in rickettsioses The total white blood cell (WBC) count is typicallynormal in patients with RMSF, but increased numbers of immature bands are generally observed. Thrombocytopenia, mild elevations in hepatic transaminases, and hyponatremia might be observed with RMSF whereas leukopenia -

Hand, Foot, and Mouth Disease (Coxsackievirus) Fact Sheet
Hand, Foot, and Mouth Disease (Coxsackievirus) Fact Sheet Hand, foot, and mouth disease is caused by one of several types of viruses Hand, foot, and mouth disease is usually characterized by tiny blisters on the inside of the mouth and the palms of the hands, fingers, soles of the feet. It is commonly caused by coxsackievirus A16 (an enterovirus), and less often by other types of viruses. Anyone can get hand, foot, and mouth disease Young children are primarily affected, but it may be seen in adults. Most cases occur in the summer and early fall. Outbreaks may occur among groups of children especially in child care centers or nursery schools. Symptoms usually appear 3 to 5 days after exposure. Hand, foot, and mouth disease is usually spread through person-to-person contact People can spread the disease when they are shedding the virus in their feces. It is also spread by the respiratory tract from mouth or respiratory secretions (such as from saliva on hands or toys). The virus has also been found in the fluid from the skin blisters. The infection is spread most easily during the acute phase/stage of illness when people are feeling ill, but the virus can be spread for several weeks after the onset of infection. The symptoms are much like a common cold with a rash The rash appears as blisters or ulcers in the mouth, on the inner cheeks, gums, sides of the tongue, and as bumps or blisters on the hands, feet, and sometimes other parts of the skin. The skin rash may last for 7 to 10 days. -

Cutaneous Melioidosis Dermatology Section
DOI: 10.7860/JCDR/2016/18823.8463 Case Report Cutaneous Melioidosis Dermatology Section BASAVAPRABHU ACHAPPA1, DEEPAK MADI2, K. VIDYALAKSHMI3 ABSTRACT Melioidosis is an emerging infection in India. It usually presents as pneumonia. Melioidosis presenting as cutaneous lesions is uncommon. We present a case of cutaneous melioidosis from Southern India. Cutaneous melioidosis can present as an ulcer, pustule or as crusted erythematous lesions. A 22-year-old gentleman known case of diabetes mellitus was admitted in our hospital with an ulcer over the left thigh. Discharge from the ulcer grew Burkholderia pseudomallei. He was successfully treated with ceftazidime. Melioidosis must be considered in the differential diagnosis of nodular or ulcerative cutaneous lesion in a diabetic patient. Keywords: B. pseudomallei, Diabetes Mellitus, Skin ulcer CASE REPORT melioidosis is a rare entity. Cutaneous melioidosis may be primary A 22-year-old gentleman was admitted in our hospital with (presenting symptom is skin infection) or secondary (melioidosis complaints of an ulcer over the left thigh of seven days duration. at other sites in the body with incidental skin involvement) [3]. History of fever was present for four days. He also complained of There is limited published data from India documenting cutaneous pain in the thigh. The patient initially noticed a nodule on the left melioidosis. thigh which eventually progressed to form a discharging ulcer. He B. pseudomallei reside in soil and water [4]. Inoculation, inhalation was a known case of diabetes mellitus (type 1) on insulin. Clinical or ingestion of infected food or water are the modes of transmission examination revealed a 5cm× 5cm ulcer on the left thigh with [5]. -
Necrotizing Fasciitis
INFORMATION ABOUT NECROTIZING FASCIITIS • Information has been circulating on social media/media outlets of an individual who developed an infection after visiting our area. We are taking this issue seriously and are working with the Indiana Department of Health to determine if this infection was caused by bacteria such as Vibrio vulnificus or other reportable disease. Currently, we do not have any information about this individual’s illness. • Necrotizing fasciitis (many times called “flesh eating bacteria” by the media) is caused by more than one type of bacteria. Several bacteria, common in our environment can cause this condition – the most common cause of necrotizing fasciitis is Group A strep. • People do not “catch” necrotizing fasciitis; it is a complication or symptom of a bacterial infection that has not been promptly or properly treated. • Sometimes people call Vibrio vulnificus the “flesh eating bacteria.” Vibrio vulnificus is a naturally occurring bacteria found in warm salty waters such as the Gulf of Mexico and surrounding bays. Concentrations of this bacteria are higher when the water is warmer. • Necrotizing fasciitis and severe infections with Vibrio vulnificus are rare. These infections can be treated with antibiotics and sometimes require surgery to remove damaged tissue. Rapid diagnosis is the key to effective treatment and recovery. • If you are healthy with a strong immune system, your chances of developing or having complications due to this condition are extremely low. HOW TO REDUCE YOUR RISK OF EXPOSURE • The Centers for Disease Control and Prevention (CDC) encourages all people to avoid open bodies of water (such as the Gulf), pools and hot tubs with breaks in the skin. -

Staging of Necrotizing Fasciitis Based on the Evolving Cutaneous Features
ReportBlackwellOxford,IJDInternational0011-905945 UK Publishing Journal LtdLtd,of Dermatology 2006 StagingWang,Case report Wong, of necrotizing and Tay fascitis of necrotizing fasciitis based on the evolving cutaneous features Yi-Shi Wang, MBBS, MRCP, Chin-Ho Wong, MBBS, MRCS, and Yong-Kwang Tay, MBBS, FRCP From the Division of Dermatology, Changi Abstract General Hospital, Department of Plastic Background Necrotizing fasciitis is a severe soft-tissue infection characterized by a fulminant Reconstructive and Aesthetic Surgery, course and high mortality. Early recognition is difficult as the disease is often clinically Singapore General Hospital, Singapore indistinguishable from cellulitis and other soft-tissue infections early in its evolution. Our aim was Correspondence to study the manifestations of the cutaneous signs of necrotizing fasciitis as the disease evolves. Yi-Shi Wang, MBBS, MRCP Methods This was a retrospective study on patients with necrotizing fasciitis at a single Division of Dermatology institution. Their charts were reviewed to document the daily cutaneous changes from the time Changi General Hospital of presentation (day 0) through to day 4 from presentation. 2 Simei Street 3 Singapore 529889 Results Twenty-two patients were identified. At initial assessment (day 0), almost all patients E-mail: [email protected] presented with erythema, tenderness, warm skin, and swelling. Blistering occurred in 41% of patients at presentation whereas late signs such as skin crepitus, necrosis, and anesthesia Presented at the European Academy of were infrequently seen (0–5%). As time elapsed, more patients had blistering (77% had blisters Dermatology and Venereology (EADV) 14th at day 4) and eventually the late signs of necrotizing fasciitis characterized by skin crepitus, Congress, London, October 12 to 16, 2005. -

Orofacial Manifestations of COVID-19: a Brief Review of the Published Literature
CRITICAL REVIEW Oral Pathology Orofacial manifestations of COVID-19: a brief review of the published literature Esam HALBOUB(a) Abstract: Coronavirus disease 2019 (COVID-19) has spread Sadeq Ali AL-MAWERI(b) exponentially across the world. The typical manifestations of Rawan Hejji ALANAZI(c) COVID-19 include fever, dry cough, headache and fatigue. However, Nashwan Mohammed QAID(d) atypical presentations of COVID-19 are being increasingly reported. Saleem ABDULRAB(e) Recently, a number of studies have recognized various mucocutaneous manifestations associated with COVID-19. This study sought to (a) Jazan University, College of Dentistry, summarize the available literature and provide an overview of the Department of Maxillofacial Surgery and potential orofacial manifestations of COVID-19. An online literature Diagnostic Sciences, Jazan, Saudi Arabia. search in the PubMed and Scopus databases was conducted to retrieve (b) AlFarabi College of Dentistry and Nursing, the relevant studies published up to July 2020. Original studies Department of Oral Medicine and published in English that reported orofacial manifestations in patients Diagnostic Sciences, Riyadh, Saudi Arabia. with laboratory-confirmed COVID-19 were included; this yielded 16 (c) AlFarabi College of Dentistry and Nursing, articles involving 25 COVID-19-positive patients. The results showed a Department of Oral Medicine and Diagnostic Sciences, Riyadh, Saudi Arabia. marked heterogeneity in COVID-19-associated orofacial manifestations. The most common orofacial manifestations were ulcerative lesions, (d) AlFarabi College of Dentistry and Nursing, Department of Restorative Dental Sciences, vesiculobullous/macular lesions, and acute sialadentitis of the parotid Riyadh, Saudi Arabia. gland (parotitis). In four cases, oral manifestations were the first signs of (e) Primary Health Care Corporation, Madinat COVID-19. -

Oral Manifestations of Systemic Disease Their Clinical Practice
ARTICLE Oral manifestations of systemic disease ©corbac40/iStock/Getty Plus Images S. R. Porter,1 V. Mercadente2 and S. Fedele3 provide a succinct review of oral mucosal and salivary gland disorders that may arise as a consequence of systemic disease. While the majority of disorders of the mouth are centred upon the focus of therapy; and/or 3) the dominant cause of a lessening of the direct action of plaque, the oral tissues can be subject to change affected person’s quality of life. The oral features that an oral healthcare or damage as a consequence of disease that predominantly affects provider may witness will often be dependent upon the nature of other body systems. Such oral manifestations of systemic disease their clinical practice. For example, specialists of paediatric dentistry can be highly variable in both frequency and presentation. As and orthodontics are likely to encounter the oral features of patients lifespan increases and medical care becomes ever more complex with congenital disease while those specialties allied to disease of and effective it is likely that the numbers of individuals with adulthood may see manifestations of infectious, immunologically- oral manifestations of systemic disease will continue to rise. mediated or malignant disease. The present article aims to provide This article provides a succinct review of oral manifestations a succinct review of the oral manifestations of systemic disease of of systemic disease. It focuses upon oral mucosal and salivary patients likely to attend oral medicine services. The review will focus gland disorders that may arise as a consequence of systemic upon disorders affecting the oral mucosa and salivary glands – as disease. -

ADVERSE FACTORS THAT CAN AFFECT on the COURSE of CHRONIC PARENCHIMATIC PAROTITIS in CHILDREN DOI: 10.36740/Wlek202006118
© Aluna Publishing Wiadomości Lekarskie, VOLUME LXXIII, ISSUE 6, JUNE 2020 ORIGINAL ARTICLE ADVERSE FACTORS THAT CAN AFFECT ON THE COURSE OF CHRONIC PARENCHIMATIC PAROTITIS IN CHILDREN DOI: 10.36740/WLek202006118 Pavlo I. Tkachenko, Serhii O. Bilokon, Yuliia V. Popelo, Nataliia M. Lokhmatova, Olha B. Dolenko, Nataliia M. Korotych UKRAINIAN MEDICAL STOMATOLOGICAL ACADEMY, POLTAVA, UKRAINE ABSTRACT The aim: The study of the presence of disorders in the ante- and postnatal periods of development of children from 2 months to 15 years with chronic parenchimatic parotitis, which may affect its course. Materials and methods: It has been examined and treated 88 children, aged from 2 months to 15 years with chronic parenchimatic parotitis, and their mothers were interviewed, who indicated the pathological course of pregnancy, childbirth and indicated the type of breastfeeding babbies. The scope of the survey included general, additional methods, consultations by related specialists and statistical processing of results. Results: 88 children with the exacerbation of chronic parenchimatic parotitis were examined (42 – (47%) with active course and 46 – (53%) with inactive). The exacerbation occurred on the background of acute infectious processes or coincided with the exacerbation of one of the chronic diseases. The first manifestations occurred in spring (55%) and autumn (36%) periods, 44% of children were hospitalized with other diagnoses. The presence of pathological conditions during pregnancy and birth defects in their mothers were recorded more often 3,5 and 3,3 times, respectively, compared with control. 70% of children received mixed and artificial feeding and were more likely to become ill. Conclusions: The severity of clinical manifestations of inflammation and disorders of the general condition depended on the activity of the course of chronic parenchimatic parotitis and were more pronounced when active. -

Oral Complications of ICU Patients with COVID-19: Case-Series and Review of Two Hundred Ten Cases
Journal of Clinical Medicine Review Oral Complications of ICU Patients with COVID-19: Case-Series and Review of Two Hundred Ten Cases Barbora Hocková 1,2,†, Abanoub Riad 3,4,*,† , Jozef Valky 5, Zuzana Šulajová 5, Adam Stebel 1, Rastislav Slávik 1, Zuzana Beˇcková 6,7, Andrea Pokorná 3,8 , Jitka Klugarová 3,4 and Miloslav Klugar 3,4 1 Department of Maxillofacial Surgery, F. D. Roosevelt University Hospital, 975 17 Banska Bystrica, Slovakia; [email protected] (B.H.); [email protected] (A.S.); [email protected] (R.S.) 2 Department of Prosthetic Dentistry, Faculty of Medicine and Dentistry, Palacky University, 775 15 Olomouc, Czech Republic 3 Czech National Centre for Evidence-Based Healthcare and Knowledge Translation (Cochrane Czech Republic, Czech EBHC: JBI Centre of Excellence, Masaryk University GRADE Centre), Institute of Biostatistics and Analyses, Faculty of Medicine, Masaryk University, 625 00 Brno, Czech Republic; [email protected] (A.P.); [email protected] (J.K.); [email protected] (M.K.) 4 Department of Public Health, Faculty of Medicine, Masaryk University, 625 00 Brno, Czech Republic 5 Department of Anaesthesiology, F. D. Roosevelt University Hospital, 975 17 Banska Bystrica, Slovakia; [email protected] (J.V.); [email protected] (Z.Š.) 6 Department of Clinical Microbiology, F. D. Roosevelt University Hospital, 975 17 Banska Bystrica, Slovakia; [email protected] 7 St. Elizabeth University of Health and Social Work, 812 50 Bratislava, Slovakia 8 Department of Nursing and Midwifery, Faculty of Medicine, Masaryk University, 625 00 Brno, Czech Republic * Correspondence: [email protected]; Tel.: +420-721-046-024 † These authors contributed equally to this work.