Stability of Metronidazole and Its Complexes with Silver(I) Salts Under Various Stress Conditions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Antiseptics and Disinfectants for the Treatment Of
Verstraelen et al. BMC Infectious Diseases 2012, 12:148 http://www.biomedcentral.com/1471-2334/12/148 RESEARCH ARTICLE Open Access Antiseptics and disinfectants for the treatment of bacterial vaginosis: A systematic review Hans Verstraelen1*, Rita Verhelst2, Kristien Roelens1 and Marleen Temmerman1,2 Abstract Background: The study objective was to assess the available data on efficacy and tolerability of antiseptics and disinfectants in treating bacterial vaginosis (BV). Methods: A systematic search was conducted by consulting PubMed (1966-2010), CINAHL (1982-2010), IPA (1970- 2010), and the Cochrane CENTRAL databases. Clinical trials were searched for by the generic names of all antiseptics and disinfectants listed in the Anatomical Therapeutic Chemical (ATC) Classification System under the code D08A. Clinical trials were considered eligible if the efficacy of antiseptics and disinfectants in the treatment of BV was assessed in comparison to placebo or standard antibiotic treatment with metronidazole or clindamycin and if diagnosis of BV relied on standard criteria such as Amsel’s and Nugent’s criteria. Results: A total of 262 articles were found, of which 15 reports on clinical trials were assessed. Of these, four randomised controlled trials (RCTs) were withheld from analysis. Reasons for exclusion were primarily the lack of standard criteria to diagnose BV or to assess cure, and control treatment not involving placebo or standard antibiotic treatment. Risk of bias for the included studies was assessed with the Cochrane Collaboration’s tool for assessing risk of bias. Three studies showed non-inferiority of chlorhexidine and polyhexamethylene biguanide compared to metronidazole or clindamycin. One RCT found that a single vaginal douche with hydrogen peroxide was slightly, though significantly less effective than a single oral dose of metronidazole. -

Identification of Candidate Agents Active Against N. Ceranae Infection in Honey Bees: Establishment of a Medium Throughput Screening Assay Based on N
RESEARCH ARTICLE Identification of Candidate Agents Active against N. ceranae Infection in Honey Bees: Establishment of a Medium Throughput Screening Assay Based on N. ceranae Infected Cultured Cells Sebastian Gisder, Elke Genersch* Institute for Bee Research, Department of Molecular Microbiology and Bee Diseases, Hohen Neuendorf, Germany * [email protected] Abstract OPEN ACCESS Many flowering plants in both natural ecosytems and agriculture are dependent on insect Citation: Gisder S, Genersch E (2015) Identification of Candidate Agents Active against N. ceranae pollination for fruit set and seed production. Managed honey bees (Apis mellifera) and wild Infection in Honey Bees: Establishment of a Medium bees are key pollinators providing this indispensable eco- and agrosystem service. Like all Throughput Screening Assay Based on N. ceranae other organisms, bees are attacked by numerous pathogens and parasites. Nosema apis is Infected Cultured Cells. PLoS ONE 10(2): e0117200. a honey bee pathogenic microsporidium which is widely distributed in honey bee popula- doi:10.1371/journal.pone.0117200 tions without causing much harm. Its congener Nosema ceranae was originally described Academic Editor: Wolfgang Blenau, Goethe as pathogen of the Eastern honey bee (Apis cerana) but jumped host from A. cerana to A. University Frankfurt, GERMANY mellifera about 20 years ago and spilled over from A. mellifera to Bombus spp. quite recent- Received: October 8, 2014 ly. N. ceranae is now considered a deadly emerging parasite of both Western honey bees Accepted: December 20, 2014 and bumblebees. Hence, novel and sustainable treatment strategies against N. ceranae are Published: February 6, 2015 urgently needed to protect honey and wild bees. -

4. Antibacterial/Steroid Combination Therapy in Infected Eczema
Acta Derm Venereol 2008; Suppl 216: 28–34 4. Antibacterial/steroid combination therapy in infected eczema Anthony C. CHU Infection with Staphylococcus aureus is common in all present, the use of anti-staphylococcal agents with top- forms of eczema. Production of superantigens by S. aureus ical corticosteroids has been shown to produce greater increases skin inflammation in eczema; antibacterial clinical improvement than topical corticosteroids alone treatment is thus pivotal. Poor patient compliance is a (6, 7). These findings are in keeping with the demon- major cause of treatment failure; combination prepara- stration that S. aureus can be isolated from more than tions that contain an antibacterial and a topical steroid 90% of atopic eczema skin lesions (8); in one study, it and that work quickly can improve compliance and thus was isolated from 100% of lesional skin and 79% of treatment outcome. Fusidic acid has advantages over normal skin in patients with atopic eczema (9). other available topical antibacterial agents – neomycin, We observed similar rates of infection in a prospective gentamicin, clioquinol, chlortetracycline, and the anti- audit at the Hammersmith Hospital, in which all new fungal agent miconazole. The clinical efficacy, antibac- patients referred with atopic eczema were evaluated. In terial activity and cosmetic acceptability of fusidic acid/ a 2-month period, 30 patients were referred (22 children corticosteroid combinations are similar to or better than and 8 adults). The reason given by the primary health those of comparator combinations. Fusidic acid/steroid physician for referral in 29 was failure to respond to combinations work quickly with observable improvement prescribed treatment, and one patient was referred be- within the first week. -

Diloxanide Furoate Drug Information, Professional 11/11/20 16:08
Diloxanide Furoate Drug Information, Professional 11/11/20 16:08 Diloxanide (Systemic) VA CLASSIFICATION Primary: AP109 Commonly used brand name(s): Entamide; Furamide. Note: For a listing of dosage forms and brand names by country availability, see Dosage Forms section(s). *Not commercially available in the U.S. †Not commercially available in Canada. Category: Antiprotozoal (systemic)— Indications Note: Because diloxanide is not commercially available in the U.S. or Canada, the bracketed information and the use of the superscript 1 in this monograph reflect the lack of labeled (approved) indications for this medication in these countries. Accepted [Amebiasis, intestinal (treatment)]1—Diloxanide is used alone as a primary agent in the treatment of asymptomatic (cyst passers) intestinal amebiasis caused by Entamoeba histolytica {01} {02} {03} {04} {05} {07} {08} {09} {10} {11} {12} {13} {14} {23} This medication may also be used concurrently, or sequentially, with other agents such as the nitroimidazoles in the treatment of invasive or extraintestinal forms of amebiasis. {03} {09} {11} {12} {14} {20} {24} https://www.drugs.com/mmx/diloxanide-furoate.html Página 1 de 9 Diloxanide Furoate Drug Information, Professional 11/11/20 16:08 Unaccepted Diloxanide alone is not effective in the treatment of invasive or extraintestinal amebiasis. {04} {07} {11} {13} 1 Not included in Canadian product labeling. Pharmacology/Pharmacokinetics Physicochemical characteristics: Source— Diloxanide furoate is the ester of 2-furoic acid and diloxanide, a dichloroacetamide derivative. {09} {13} The furoate ester is more active than the parent compound, diloxanide {13} Molecular weight— Diloxanide: 234.08 {15} Diloxanide furoate: 328.2 {16} Mechanism of action/Effect: Luminal amebicide. -
Clioquinol: Summary Report
Clioquinol: Summary Report Item Type Report Authors Gianturco, Stephanie L.; Pavlech, Laura L.; Storm, Kathena D.; Yoon, SeJeong; Yuen, Melissa V.; Mattingly, Ashlee N. Publication Date 2020-01 Keywords Clioquinol; Compounding; Food, Drug, and Cosmetic Act, Section 503B; Food and Drug Administration; Outsourcing facility; Drug compounding; Legislation, Drug; United States Food and Drug Administration Rights Attribution-NoDerivatives 4.0 International Download date 24/09/2021 22:12:31 Item License http://creativecommons.org/licenses/by-nd/4.0/ Link to Item http://hdl.handle.net/10713/12091 Summary Report Clioquinol Prepared for: Food and Drug Administration Clinical use of bulk drug substances nominated for inclusion on the 503B Bulks List Grant number: 2U01FD005946 Prepared by: University of Maryland Center of Excellence in Regulatory Science and Innovation (M-CERSI) University of Maryland School of Pharmacy January 2020 This report was supported by the Food and Drug Administration (FDA) of the U.S. Department of Health and Human Services (HHS) as part of a financial assistance award (U01FD005946) totaling $2,342,364, with 100 percent funded by the FDA/HHS. The contents are those of the authors and do not necessarily represent the official views of, nor an endorsement by, the FDA/HHS or the U.S. Government. 1 Table of Contents REVIEW OF NOMINATIONS ................................................................................................... 4 METHODOLOGY ................................................................................................................... -

Effect of 8-Hydroxyquinoline and Derivatives on Human Neuroblastoma SH-SY5Y Cells Under High Glucose
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Crossref Effect of 8-hydroxyquinoline and derivatives on human neuroblastoma SH-SY5Y cells under high glucose Wilasinee Suwanjang1, Supaluk Prachayasittikul2 and Virapong Prachayasittikul3 1 Center for Research and Innovation, Faculty of Medical Technology, Mahidol University, Bangkok, Thailand 2 Center of Data Mining and Biomedical Informatics, Faculty of Medical Technology, Mahidol University, Bangkok, Thailand 3 Department of Clinical Microbiology and Applied Technology, Faculty of Medical Technology, Mahidol University, Bangkok, Thailand ABSTRACT 8-Hydroxyquinoline and derivatives exhibit multifunctional properties, including antioxidant, antineurodegenerative, anticancer, anti-inflammatory and antidiabetic activities. In biological systems, elevation of intracellular calcium can cause calpain activation, leading to cell death. Here, the effect of 8-hydroxyquinoline and derivatives (5-chloro-7-iodo-8-hydroxyquinoline or clioquinol and 8-hydroxy-5-nitroquinoline or nitroxoline) on calpain-dependent (calpain-calpastatin) pathways in human neu- roblastoma (SH-SY5Y) cells was investigated. 8-Hydroxyquinoline and derivatives ameliorated high glucose toxicity in SH-SY5Y cells. The investigated compounds, particularly clioquinol, attenuated the increased expression of calpain, even under high- glucose conditions. 8-Hydroxyquinoline and derivatives thus adversely affected the promotion of neuronal cell death by high glucose via the calpain-calpastatin -

Are Blastocystis Species Clinically Relevant to Humans?
Are Blastocystis species clinically relevant to humans? Robyn Anne Nagel MB, BS, FRACP A thesis submitted for the degree of Doctor of Philosophy at the University of Queensland in 2015 School of Veterinary Science Title page Culture of human faecal specimen Blastocystis organisms, vacuolated and granular forms, Photographed RAN: x40 magnification, polarised light ii Abstract Blastocystis spp. are the most common enteric parasites found in human stool and yet, the life cycle of the organism is unknown and the clinical relevance uncertain. Robust cysts transmit infection, and many animals carry the parasite. Infection in humans has been linked to Irritable bowel syndrome (IBS). Although Blastocystis carriage is much higher in IBS patients, studies have not been able to confirm Blastocystis spp. are the direct cause of symptoms. Moreover, eradication is often unsuccessful. A number of approaches were utilised in order to investigate the clinical relevance of Blastocystis spp. in human IBS patients. Deconvolutional microscopy with time-lapse imaging and fluorescent spectroscopy of xenic cultures of Blastocystis spp. from IBS patients and healthy individuals was performed. Green autofluorescence (GAF), most prominently in the 557/576 emission spectra, was observed in the vacuolated, granular, amoebic and cystic Blastocystis forms. This first report of GAF in Blastocystis showed that a Blastocystis-specific fluorescein-conjugated antibody could be partially distinguished from GAF. Surface pores of 1m in diameter were observed cyclically opening and closing over 24 hours and may have nutritional or motility functions. Vacuolated forms, extruded a viscous material slowly over 12 hours, a process likely involving osmoregulation. Tear- shaped granules were observed exiting from the surface of an amoebic form but their identity and function could not be elucidated. -

Recurrent Amebic Liver Abscesses Over a 16-Year Period: a Case Report
Creemers‑Schild et al. BMC Res Notes (2016) 9:472 DOI 10.1186/s13104-016-2275-0 BMC Research Notes CASE REPORT Open Access Recurrent amebic liver abscesses over a 16‑year period: a case report D. Creemers‑Schild1,2, P. J. J. van Genderen1, L. G. Visser2, J. J. van Hellemond3* and P. J. Wismans1 Abstract Background: Amebic liver abscess is a rare disease in high-income countries. Recurrence of amebic liver abscess is even rarer with only a few previous reports. Here we present a patient who developed three subsequent amebic liver abscesses over a sixteen-year period. Case presentation: A Caucasian male developed recurrent amebic liver abscesses, when aged 23, 27 and 39 years. Only on the first occasion did this coincide with a recent visit to the tropics. The patient received adequate treatment during each episode. Possible explanations are persistent asymptomatic carrier state, cysts passage in his family, re- infection or chance. Conclusion: We describe the unusual case of a healthy male who developed recurrent amebic liver abscesses over a long period despite adequate treatment. Possible pathophysiological explanations are explored. Keywords: Entamoeba histolytica, Amebiasis, Carrier state environment, Immune response, Relapse, Treatment Background times over a period of 16 years, despite adequate combi- Intestinal amebiasis and amebic liver abscess, caused by nation treatment on each occasion. the protozoan Entamoeba histolytica, are rarely reported from high-income countries. It is mostly encountered as Case presentation an imported disease from regions with poor sanitation A previously healthy 23-year old, Caucasian man was levels. Infection occurs through ingestion of E. -
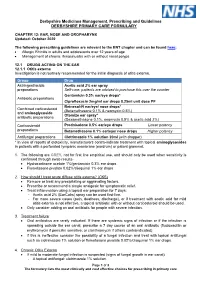
EAR, NOSE and OROPHARYNX Updated: October 2020
Derbyshire Medicines Management, Prescribing and Guidelines DERBYSHIRE PRIMARY CARE FORMULARY CHAPTER 12: EAR, NOSE AND OROPHARYNX Updated: October 2020 The following prescribing guidelines are relevant to the ENT chapter and can be found here: • Allergic Rhinitis in adults and adolescents over 12 years of age • Management of chronic rhinosinusitis with or without nasal polyps 12.1 DRUGS ACTING ON THE EAR 12.1.1 Otitis externa Investigation is not routinely recommended for the initial diagnosis of otitis externa. Group Drug Astringent/acidic Acetic acid 2% ear spray preparations Self-care: patients are advised to purchase this over the counter Gentamicin 0.3% ear/eye drops* Antibiotic preparations Ciprofloxacin 2mg/ml ear drops 0.25ml unit dose PF Betnesol-N ear/eye/ nose drops* Combined corticosteroid (Betamethasone 0.1% & neomycin 0.5%) and aminoglycoside Otomize ear spray* antibiotic preparations (Dexamethasone 0.1%, neomycin 0.5% & acetic acid 2%) Corticosteroid Prednisolone 0.5% ear/eye drops Lower potency preparations Betamethasone 0.1% ear/eye/ nose drops Higher potency Antifungal preparations Clotrimazole 1% solution 20ml (with dropper) * In view of reports of ototoxicity, manufacturers contra-indicate treatment with topical aminoglycosides in patients with a perforated tympanic membrane (eardrum) or patent grommet. 1. The following are GREY, not for first line empirical use, and should only be used when sensitivity is confirmed through swab results- • Hydrocortisone acetate 1%/gentamicin 0.3% ear drops • Flumetasone pivalate 0.02%/clioquinol 1% ear drops 2. How should I treat acute diffuse otitis externa? (CKS) • Remove or treat any precipitating or aggravating factors. • Prescribe or recommend a simple analgesic for symptomatic relief. -

Chemical Modulators of Fibrinogen Production and Their Impact on Venous Thrombosis
Published online: 2020-12-10 Coagulation and Fibrinolysis 433 Chemical Modulators of Fibrinogen Production and Their Impact on Venous Thrombosis Rui Vilar1 Samuel W. Lukowski1,2 Marco Garieri1 Corinne Di Sanza1 Marguerite Neerman-Arbez1,3 Richard J. Fish1 1 Department of Genetic Medicine and Development, University of Address for correspondence Richard J. Fish, Department of Genetic Geneva Faculty of Medicine, Geneva, Switzerland Medicine and Development, Faculty of Medicine, University of 2 Institute for Molecular Bioscience, The University of Queensland, Geneva, 1, rue Michel-Servet, Geneva 1206, Switzerland Saint Lucia, Queensland, Australia (e-mail: [email protected]). 3 iGE3, Institute of Genetics and Genomics in Geneva, Geneva, Switzerland Thromb Haemost 2021;121:433–448. Abstract Thrombosis is a leading cause of morbidity and mortality. Fibrinogen, the soluble substrate for fibrin-based clotting, has a central role in haemostasis and thrombosis and its plasma concentration correlates with cardiovascular disease event risk and a prothrombotic state in experimental models. We aimed to identify chemical entities capable of changing fibrinogen production and test their impact on experimental thrombosis. A total of 1,280 bioactive compounds were screened for their ability to alter fibrinogen production by hepatocyte-derived cancer cells and a selected panel was tested in zebrafish larvae. Anthralin and all-trans retinoic acid (RA) were identified as fibrinogen-lowering and fibrinogen-increasing moieties, respectively. In zebrafish larvae, anthralin prolonged laser-induced venous occlusion times and reduced thrombocyte accumulation at injury sites. RA had opposite effects. Treatment with RA, a nuclear receptor ligand, increased fibrinogen mRNA levels. Using an antisense morpholino oligonucleotide to deplete zebra- fish fibrinogen, we correlated a shortening of laser-induced venous thrombosis times with RA treatment and fibrinogen protein levels. -
![Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set](https://docslib.b-cdn.net/cover/8870/ehealth-dsi-ehdsi-v2-2-2-or-ehealth-dsi-master-value-set-1028870.webp)
Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set
MTC eHealth DSI [eHDSI v2.2.2-OR] eHealth DSI – Master Value Set Catalogue Responsible : eHDSI Solution Provider PublishDate : Wed Nov 08 16:16:10 CET 2017 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 1 of 490 MTC Table of Contents epSOSActiveIngredient 4 epSOSAdministrativeGender 148 epSOSAdverseEventType 149 epSOSAllergenNoDrugs 150 epSOSBloodGroup 155 epSOSBloodPressure 156 epSOSCodeNoMedication 157 epSOSCodeProb 158 epSOSConfidentiality 159 epSOSCountry 160 epSOSDisplayLabel 167 epSOSDocumentCode 170 epSOSDoseForm 171 epSOSHealthcareProfessionalRoles 184 epSOSIllnessesandDisorders 186 epSOSLanguage 448 epSOSMedicalDevices 458 epSOSNullFavor 461 epSOSPackage 462 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 2 of 490 MTC epSOSPersonalRelationship 464 epSOSPregnancyInformation 466 epSOSProcedures 467 epSOSReactionAllergy 470 epSOSResolutionOutcome 472 epSOSRoleClass 473 epSOSRouteofAdministration 474 epSOSSections 477 epSOSSeverity 478 epSOSSocialHistory 479 epSOSStatusCode 480 epSOSSubstitutionCode 481 epSOSTelecomAddress 482 epSOSTimingEvent 483 epSOSUnits 484 epSOSUnknownInformation 487 epSOSVaccine 488 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 3 of 490 MTC epSOSActiveIngredient epSOSActiveIngredient Value Set ID 1.3.6.1.4.1.12559.11.10.1.3.1.42.24 TRANSLATIONS Code System ID Code System Version Concept Code Description (FSN) 2.16.840.1.113883.6.73 2017-01 A ALIMENTARY TRACT AND METABOLISM 2.16.840.1.113883.6.73 2017-01 -

Chromatographic Methods for Simultaneous Determination of Diiodohydroxyquinoline and Metronidazole in Their Binary Mixture
Chromatographic methods for simultaneous determination of diiodohydroxyquinoline and Metronidazole in their binary mixture Nouruddin Wageih Ali1*, Mohammed Gamal1 and Mohammed Abdelkawy2 1Pharmaceutical Analytical Chemistry Department, Faculty of Pharmacy, Beni-Suef University, Alshaheed Shehata Ahmed Hegazy St., Beni-Suef Egypt 2Pharmaceutical Analytical Chemistry Department, Faculty of Pharmacy, Cairo University, Kasr El-Aini St., Cairo, Egypt Abstract: Two chromatographic methods were developed for analysis ofdiiodohydroxyquinoline (DIHQ) and metronidazole (MTN). In the first method, diiodohydroxyquinoline and metronidazole were separated on TLC silica gel 60F254 plate using chloroform: acetone: glacial acetic acid (7.5: 2.5: 0.1, by volume) as mobile phase. The obtained bands were then scanned at 254 nm. The second method is a RP-HPLC method in which diiodohydroxyquinoline and metronidazole were separated on a reversed-phase C18 column using water : methanol (60 :40, V/V, PH=3.6 )as mobile phase at a flow rate of 0.7 mL.min-1 and UV detection at 220 nm. The mentioned methods were successfully used for determination of diiodohydroxyquinoline and metronidazole in pure form and in their pharmaceutical formulation. Keywords: TLC-spectrodensitometry, RP-HPLC, diiodohydroxyquinoline and metronidazole. INTRODUCTION (Argekaret al., 1996), GC (Wang et al., 2001), atomic absorption spectrometry (Nejem et al., 2008), iodometric Metronidazole (MTN) is 2-methyl-5-nitroimidazole-1- titration (Soliman, 1975) and non aqueous titration ethanol (Merck, 2006). It is a 5-nitroimidazole derivative (Kavarana, 1959; Paranjothy and Banerjee., 1973). with activity against anaerobic bacteria and protozoa. MTN is an amoebicide at whole sites of infection with Few methods have been mentioned for analysis of DIHQ Entamoeba histolytica.