Appendix H Pediatric Quality Indicators Appendices
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Premature Ovarian Insufficiency
biomedicines Review Premature Ovarian Insufficiency: Procreative Management and Preventive Strategies Jennifer J. Chae-Kim 1 and Larisa Gavrilova-Jordan 2,* 1 Department of Obstetrics and Gynecology, East Carolina University, Greenville, NC 27834, USA; [email protected] 2 Department of Obstetrics and Gynecology, Augusta University, Augusta, GA 30912, USA * Correspondence: [email protected]; Tel.: +1-706-721-3832 Received: 30 November 2018; Accepted: 24 December 2018; Published: 28 December 2018 Abstract: Premature ovarian insufficiency (POI) is the loss of normal hormonal and reproductive function of ovaries in women before age 40 as the result of premature depletion of oocytes. The incidence of POI increases with age in reproductive-aged women, and it is highest in women by the age of 40 years. Reproductive function and the ability to have children is a defining factor in quality of life for many women. There are several methods of fertility preservation available to women with POI. Procreative management and preventive strategies for women with or at risk for POI are reviewed. Keywords: premature ovarian insufficiency; in vitro fertilization; donor oocyte; fertility preservation 1. Introduction Premature ovarian insufficiency (POI) is the loss of normal hormonal and reproductive function of ovaries in women before age 40 as the result of premature depletion of oocytes. POI is characterized by elevated gonadotrophin levels, hypoestrogenism, and amenorrhea, occurring years before the average age of menopause. Previously referred to as ovarian failure or early menopause, POI is now understood to be a condition that encompasses a range of impaired ovarian function, with clinical implications overlapping but not synonymous to that of physiologic menopause. -

Primary Cutaneous Nocardiosis: a Case Study and Review
Study Primary cutaneous nocardiosis: A case study and review Arun C. Inamadar, Aparna Palit Department of Dermatology, Venereology & Leprosy, BLDEA’s SBMP Medical College, Hospital & Research Centre, Bijapur, India. Address for correspondence: Dr. Arun C. Inamadar, Professor & Head, Department of Dermatology, Venereology & Leprosy, BLDEA’s SBMP Medical College, Hospital & Research Centre, Bijapur - 586103, India. E-mail: [email protected]. ABSTRACT Background: Primary cutaneous nocardiosis is an uncommon entity. It usually occurs among immunocompetent but occupationally predisposed individuals. Aim: To study clinical profile of patients with primary cutaneous nocardiosis in a tertiary care hospital and to review the literature. Methods: The records of 10 cases of primary cutaneous nocardiosis were analyzed for clinical pattern, site of involvement with cultural study and response to treatment. Results: All the patients were agricultural workers (nine male) except one housewife. The commonest clinical type was mycetoma. Unusual sites like the scalp and back were involved in two cases. Culture was positive in six cases with N. brasiliensis being commonest organism. N. nova which was previously unreported cause of lymphocutaneous nocardiosis, was noted in one patient, who had associated HIV infection. All the patients responded to cotrimaxazole. Conclusion: Mycetoma is the commonest form of primary cutaneous nocardiosis and responds well to cotrimoxazole. KEY WORDS: Primary cutaneous nocardiosis, Mycetoma, Lymphocutaneous nocardiosis INTRODUCTION infection is prevalent. Many of the large series on nocardial infections mention the incidence of Cutaneous nocardiosis presents either as a part of cutaneous nocardiosis without specifying whether the disseminated infection or as a primary infection infection is primary or secondary. Indian reports of resulting from inoculation. -

Granulomatous Diseases: Disease: Tuberculosis Leprosy Buruli Ulcer
Granulomatous diseases: Disease: Tuberculosis Leprosy Buruli ulcer MOTT diseases Actinomycosis Nocardiosis Etiology Mycobacterium M. leprae M. ulcerans M. kansasii Actinomyces israelii Nocardia asteroides tuberculosis M. scrofulaceum M. africanum M. avium- M. bovis intracellulare M. marinum Reservoir Humans (M. tuberculosis, HUMANS only Environment Environment HUMANS only Environment M. africanum*) (uncertain) Animals (M. bovis) Infects animals Transmission Air-borne route Air-borne route Uncertain: Air-borne NONE Air-borne route to humans Food-borne route Direct contact traumatic Traumatic inoculation endogenous infection Traumatic (M. bovis) inoculation, Habitat: oral cavity, inoculation insect bite? intestines, female genital tract Clinical Tuberculosis (TB): Leprosy=Hansen’s Disseminating Lung disease Abscesses in the skin Broncho-pulmonary picture pulmonary and/or disease skin ulcers Cervical lymphadenitis adjacent to mucosal surfaces (lung abscesses) extra-pulmonary Tuberculoid leprosy Disseminated (cervicofacial actinomycosis), Cutaneous infections (disseminated: kidneys, Lepromatous leprosy infection in the lungs (pulmonary) or such as: mycetoma, bones, spleen, meninges) Skin infections in the abdominal cavity lymphocutaneous (peritonitis, abscesses in infections, ulcerative appendix and ileocecal lesions, abscesses, regions) cellulitis; Dissemination: brain abscesses Distribution All over the world India, Brazil, Tropical disease All over the world All humans Tropical disease * Africa Indonesia, Africa (e.g. Africa, Asia, (e.g. -

17110-Disseminated-Nocardiosis-A-Case-Report.Pdf
Open Access Case Report DOI: 10.7759/cureus.5294 Disseminated Nocardiosis: A Case Report Ines M. Leite 1 , Frederico Trigueiros 1 , André M. Martins 1 , Marina Fonseca 1 , Tiago Marques 2 1. Serviço De Medicina 2, Hospital De Santa Maria, Lisboa, PRT 2. Serviço De Doenças Infecciosas, Hospital De Santa Maria, Lisboa, PRT Corresponding author: Ines M. Leite, [email protected] Abstract Disseminated nocardiosis is a rare infection associated with underlying immunosuppression, and patients usually have some identifiable risk factor affecting cellular immunity. Due to advances in taxonomy and microbiology identification methods, infections by Nocardia species are more frequent, making the discussion of its approach and choice of antibiotherapy increasingly relevant. A 77-year-old man presented to the emergency department with marked pain on the right lower limb, weakness, and upper leg edema. He had been diagnosed with organized cryptogenic pneumonia one year before and was chronically immunosuppressed with methylprednisolone 32 mg/day. Blood cultures isolated Nocardia cyriacigeorgica. Computed tomography revealed a gas collection in the region of the right iliacus muscle with involvement of the gluteal and obturator muscles upwardly and on the supragenicular plane inferiorly. Triple therapy with imipenem, amikacin, and cotrimoxazole was started, and the patient was submitted for emergent surgical decompression, fasciotomy, and drainage due to acute compartment syndrome. The patient had a good outcome and was discharged from the hospital after 30 days of intravenous therapy. This case illustrates the severity of Nocardia infection and highlights the need for a meticulous approach in the diagnosis and treatment of these patients. Categories: Internal Medicine, Infectious Disease Keywords: nocardia, nocardia infection, immunosuppression Introduction In the suborder of Corynebacterineae, three genera have strains that may be pathological to humans, with some characteristics similar to Fungi: Mycobacterium, Corynebacterium, and Nocardia. -

ICD10 Diagnoses FY2018 AHD.Com
ICD10 Diagnoses FY2018 AHD.com A020 Salmonella enteritis A5217 General paresis B372 Candidiasis of skin and nail A040 Enteropathogenic Escherichia coli A523 Neurosyphilis, unspecified B373 Candidiasis of vulva and vagina infection A528 Late syphilis, latent B3741 Candidal cystitis and urethritis A044 Other intestinal Escherichia coli A530 Latent syphilis, unspecified as early or B3749 Other urogenital candidiasis infections late B376 Candidal endocarditis A045 Campylobacter enteritis A539 Syphilis, unspecified B377 Candidal sepsis A046 Enteritis due to Yersinia enterocolitica A599 Trichomoniasis, unspecified B3781 Candidal esophagitis A047 Enterocolitis due to Clostridium difficile A6000 Herpesviral infection of urogenital B3789 Other sites of candidiasis A048 Other specified bacterial intestinal system, unspecified B379 Candidiasis, unspecified infections A6002 Herpesviral infection of other male B380 Acute pulmonary coccidioidomycosis A049 Bacterial intestinal infection, genital organs B381 Chronic pulmonary coccidioidomycosis unspecified A630 Anogenital (venereal) warts B382 Pulmonary coccidioidomycosis, A059 Bacterial foodborne intoxication, A6920 Lyme disease, unspecified unspecified unspecified A7740 Ehrlichiosis, unspecified B387 Disseminated coccidioidomycosis A080 Rotaviral enteritis A7749 Other ehrlichiosis B389 Coccidioidomycosis, unspecified A0811 Acute gastroenteropathy due to A879 Viral meningitis, unspecified B399 Histoplasmosis, unspecified Norwalk agent A938 Other specified arthropod-borne viral B440 Invasive pulmonary -
Womens Health Requisition Forms
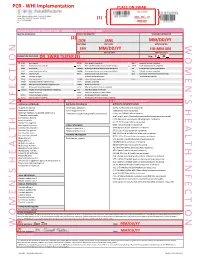
PCR - WHI Implementation PLACE ON SWAB 10854 Midwest Industrial Blvd. St. Louis, MO 63132 MM DD YY Phone: (314) 200-3040 | Fax (314) 200-3042 (1) CLIA ID #26D0953866 JANE DOE v3 PCR MOLECULAR REQUISITION - WOMEN'S HEALTH INFECTION PRACTICE INFORMATION PATIENT INFORMATION *SPECIMEN INFORMATION (2) DOE JANE MM/DD/YY LAST NAME FIRST NAME DATE COLLECTED W O M E ' N S H E A L T H I F N E C T I O N SSN MM/DD/YY HH:MM AM SSN DATE OF BIRTH TIME COLLECTED REQUESTING PHYSICIAN: DR. SWAB TESTER (3) Sex: F X M (4) Diagnosis Codes X N76.0 Acute vaginitis B37.49 Other urogenital candidiasis A54.9 Gonococcal infection, unspecified N76.1 Subacute and chronic vaginitis N89.8 Other specified noninflammatory disorders of vagina A59.00 Urogenital trichomoniasis, unspecified N76.2 Acute vulvitis O99.820 Streptococcus B carrier state complicating pregnancy A64 Unspecified sexually transmitted disease N76.3 Subacute and chronic vulvitis O99.824 Streptococcus B carrier state complicating childbirth A74.9 Chlamydial infection, unspecified N76.4 Abscess of vulva B95.1 Streptococcus, group B, as the cause Z11.3 Screening for infections with a predmoninantly N76.5 Ulceration of vagina of diseases classified elsewhere sexual mode of trasmission N76.6 Ulceration of vulva Z22.330 Carrier of group B streptococcus Other: N76.81 Mucositis(ulcerative) of vagina and vulva N70.91 Salpingitis, unspecified N76.89 Other specified inflammation of vagina and vulva N70.92 Oophoritis, unspecified N95.2 Post menopausal atrophic vaginitis N71.9 Inflammatory disease of uterus, unspecified -

Menstrual Disorders Susan Hayden Gray, MD* Practice Gap 1
Article genital system disorders Menstrual Disorders Susan Hayden Gray, MD* Practice Gap 1. Dysmenorrhea, amenorrhea, and abnormal vaginal bleeding affect the majority of Author Disclosure adolescent females, impacting quality of life and school attendance. Patient-centered Dr Gray has disclosed adolescent care should include searching for, assessing, and managing menstrual concerns. no financial 2. Polycystic ovary syndrome (PCOS) is the most common endocrinopathy in young relationships relevant adult women, and pediatricians should recognize, monitor, educate, and manage their to this article. This patients who fit the medical profile for PCOS based on any/all of the three sets of commentary does diagnostic criteria. contain a discussion of an unapproved/ Objectives After reading this article, readers should be able to: investigative use of a commercial product/ 1. Define primary and secondary amenorrhea and list the differential diagnosis for each. device. 2. Recognize the importance of a sensitive urine pregnancy test early in the evaluation of menstrual disorders, regardless of stated sexual history. 3. Know that polycystic ovary syndrome is a common cause of secondary amenorrhea in adolescents and may present with oligomenorrhea or abnormal uterine bleeding. 4. Recognize that eating disordered behaviors are a common cause of secondary amenorrhea and irregular bleeding, and treatment of the eating disordered behavior is the best recommendation to ensure resumption of regular menses and long-term bone health. 5. Know the differential diagnosis of abnormal uterine bleeding and describe the preferred treatment, recognizing the central importance of iron replacement. 6. Understand the prevalence of primary dysmenorrhea and its role in causing recurrent school absence in young women, and describe its evaluation and management. -

N35.12 Postinfective Urethral Stricture, NEC, Female N35.811 Other
N35.12 Postinfective urethral stricture, NEC, female N35.811 Other urethral stricture, male, meatal N35.812 Other urethral bulbous stricture, male N35.813 Other membranous urethral stricture, male N35.814 Other anterior urethral stricture, male, anterior N35.816 Other urethral stricture, male, overlapping sites N35.819 Other urethral stricture, male, unspecified site N35.82 Other urethral stricture, female N35.911 Unspecified urethral stricture, male, meatal N35.912 Unspecified bulbous urethral stricture, male N35.913 Unspecified membranous urethral stricture, male N35.914 Unspecified anterior urethral stricture, male N35.916 Unspecified urethral stricture, male, overlapping sites N35.919 Unspecified urethral stricture, male, unspecified site N35.92 Unspecified urethral stricture, female N36.0 Urethral fistula N36.1 Urethral diverticulum N36.2 Urethral caruncle N36.41 Hypermobility of urethra N36.42 Intrinsic sphincter deficiency (ISD) N36.43 Combined hypermobility of urethra and intrns sphincter defic N36.44 Muscular disorders of urethra N36.5 Urethral false passage N36.8 Other specified disorders of urethra N36.9 Urethral disorder, unspecified N37 Urethral disorders in diseases classified elsewhere N39.0 Urinary tract infection, site not specified N39.3 Stress incontinence (female) (male) N39.41 Urge incontinence N39.42 Incontinence without sensory awareness N39.43 Post-void dribbling N39.44 Nocturnal enuresis N39.45 Continuous leakage N39.46 Mixed incontinence N39.490 Overflow incontinence N39.491 Coital incontinence N39.492 Postural -

AMENORRHOEA Amenorrhoea Is the Absence of Menses in a Woman of Reproductive Age
AMENORRHOEA Amenorrhoea is the absence of menses in a woman of reproductive age. It can be primary or secondary. Secondary amenorrhoea is absence of periods for at least 3 months if the patient has previously had regular periods, and 6 months if she has previously had oligomenorrhoea. In contrast, oligomenorrhoea describes infrequent periods, with bleeds less than every 6 weeks but at least one bleed in 6 months. Aetiology of amenorrhea in adolescents (from Golden and Carlson) Oestrogen- Oestrogen- Type deficient replete Hypothalamic Eating disorders Immaturity of the HPO axis Exercise-induced amenorrhea Medication-induced amenorrhea Chronic illness Stress-induced amenorrhea Kallmann syndrome Pituitary Hyperprolactinemia Prolactinoma Craniopharyngioma Isolated gonadotropin deficiency Thyroid Hypothyroidism Hyperthyroidism Adrenal Congenital adrenal hyperplasia Cushing syndrome Ovarian Polycystic ovary syndrome Gonadal dysgenesis (Turner syndrome) Premature ovarian failure Ovarian tumour Chemotherapy, irradiation Uterine Pregnancy Androgen insensitivity Uterine adhesions (Asherman syndrome) Mullerian agenesis Cervical agenesis Vaginal Imperforate hymen Transverse vaginal septum Vaginal agenesis The recommendations for those who should be evaluated have recently been changed to those shown below. (adapted from Diaz et al) Indications for evaluation of an adolescent with primary amenorrhea 1. An adolescent who has not had menarche by age 15-16 years 2. An adolescent who has not had menarche and more than three years have elapsed since thelarche 3. An adolescent who has not had a menarche by age 13-14 years and no secondary sexual development 4. An adolescent who has not had menarche by age 14 years and: (i) there is a suspicion of an eating disorder or excessive exercise, or (ii) there are signs of hirsutism, or (iii) there is suspicion of genital outflow obstruction Pregnancy must always be excluded. -

Clinical Practice Guideline for the Management of Anorectal Abscess, Fistula-In-Ano, and Rectovaginal Fistula Jon D
PRACTICE GUIDELINES Clinical Practice Guideline for the Management of Anorectal Abscess, Fistula-in-Ano, and Rectovaginal Fistula Jon D. Vogel, M.D. • Eric K. Johnson, M.D. • Arden M. Morris, M.D. • Ian M. Paquette, M.D. Theodore J. Saclarides, M.D. • Daniel L. Feingold, M.D. • Scott R. Steele, M.D. Prepared on behalf of The Clinical Practice Guidelines Committee of the American Society of Colon and Rectal Surgeons he American Society of Colon and Rectal Sur- and submucosal locations.7–11 Anorectal abscess occurs geons is dedicated to ensuring high-quality pa- more often in males than females, and may occur at any Ttient care by advancing the science, prevention, age, with peak incidence among 20 to 40 year olds.4,8–12 and management of disorders and diseases of the co- In general, the abscess is treated with prompt incision lon, rectum, and anus. The Clinical Practice Guide- and drainage.4,6,10,13 lines Committee is charged with leading international Fistula-in-ano is a tract that connects the perine- efforts in defining quality care for conditions related al skin to the anal canal. In patients with an anorec- to the colon, rectum, and anus by developing clinical tal abscess, 30% to 70% present with a concomitant practice guidelines based on the best available evidence. fistula-in-ano, and, in those who do not, one-third will These guidelines are inclusive, not prescriptive, and are be diagnosed with a fistula in the months to years after intended for the use of all practitioners, health care abscess drainage.2,5,8–10,13–16 Although a perianal abscess workers, and patients who desire information about the is defined by the anatomic space in which it forms, a management of the conditions addressed by the topics fistula-in-ano is classified in terms of its relationship to covered in these guidelines. -

Infection and Infertility
Chapter 1 Infection and Infertility Rutvij Dalal Additional information is available at the end of the chapter http://dx.doi.org/10.5772/64168 Abstract About 1/3rd of all women diagnosed with subfertility have a tubo-peritoneal factor contri‐ buting to their condition. Most of these alterations in tubo-ovarian function come from post-inflammatory damage inflicted after a pelvic or sexually transmitted infection. Sal‐ pingitis occurs in an estimated 15% of reproductive-age women, and 2.5% of all women become infertile as a result of salpingitis by age 35. Predominant organisms today include those from the Chamydia species and the infection causes minimal to no symptoms – leading to chronic infection and consequently more damage. Again, a large proportion of patients suffering from pelvic infection contributing to their subfertility are undiagnosed to be having an infection. Chronic inflammation of the cervix and endometrium, altera‐ tions in reproductive tract secretions, induction of immune mediators that interfere with gamete or embryo physiology, and structural disorders such as intrauterine synechiae all contribute to female infertility. Infection is also a major factor in male subfertility, second only to abnormal semen parameters. Epididymal or ductal obstruction, testicular damage from orchitis, development of anti-sperm antibodies, etc are all possible mechanisms by which infection can affect male fertility. Keywords: Infertility, Infection, pelvic inflammatory disease, salpingitis, epididymo-or‐ chitis, antisperm antibodies 1. Introduction The association between infection and infertility has been long known. Of all causes of female Infertility, tubal or peritoneal factors amount to about 30-40. The infections that lead to asymptomatic infections are more damaging as lack of symptoms prevents a patient from seeking timely medical intervention and consequently chronic damage to pelvic organs. -

Clinical Characteristics and Incidence of Perianal Diseases in Patients with Ulcerative Colitis
Annals of Original Article Coloproctology Ann Coloproctol 2018;34(3):138-143 pISSN 2287-9714 eISSN 2287-9722 https://doi.org/10.3393/ac.2017.06.08 www.coloproctol.org Clinical Characteristics and Incidence of Perianal Diseases in Patients With Ulcerative Colitis Yong Sung Choi1, Do Sun Kim2, Doo Han Lee2, Jae Bum Lee2, Eun Jung Lee2, Seong Dae Lee2, Kee Ho Song2, Hyung Joong Jung2 Departments of 1Gastroenterology and 2Surgery, Daehang Hospital, Seoul, Korea Purpose: While perianal disease (PAD) is a characteristic of patients with Crohn disease, it has been overlooked in pa- tients with ulcerative colitis (UC). Thus, our study aimed to analyze the incidence and the clinical features of PAD in pa- tients with UC. Methods: We reviewed the data on 944 patients with an initial diagnosis of UC from October 2003 to October 2015. PAD was categorized as hemorrhoids, anal fissures, abscesses, and fistulae after anoscopic examination by experienced proctol- ogists. Data on patients’ demographics, incidence and types of PAD, medications, surgical therapies, and clinical course were analyzed. Results: The median follow-up period was 58 months (range, 12–142 months). Of the 944 UC patients, the cumulative in- cidence rates of PAD were 8.1% and 16.0% at 5 and 10 years, respectively. The incidence rates of bleeding hemorrhoids, anal fissures, abscesses, and fistulae at 10 years were 6.7%, 5.3%, 2.6%, and 3.4%, respectively. The cumulative incidence rates of perianal sepsis (abscess or fistula) were 2.2% and 4.5% at 5 and 10 years, respectively. In the multivariate analyses, male sex (risk ratio [RR], 4.6; 95% confidence interval [CI], 1.7–12.5) and extensive disease (RR, 4.2; 95% CI, 1.6–10.9) were significantly associated with the development of perianal sepsis.