The Raynaud Syndrome MARTIN BIRNSTINGL
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Documentationand Coding Tips: Peripheral Vascular Disease
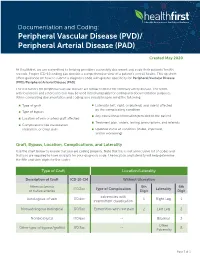
Documentation and Coding: Peripheral Vascular Disease (PVD)/ Peripheral Arterial Disease (PAD) Created May 2020 At Healthfirst, we are committed to helping providers accurately document and code their patients’ health records. Proper ICD-10 coding can provide a comprehensive view of a patient’s overall health. This tip sheet offers guidance on how to submit a diagnosis code with greater specificity for Peripheral Vascular Disease (PVD)/Peripheral Arterial Disease (PAD). The risk factors for peripheral vascular disease are similar to those for coronary artery disease. The terms arteriosclerosis and atherosclerosis may be used interchangeably for coding and documentation purposes. When completing documentation and coding, you should keep in mind the following: Type of graft Laterality (left, right, or bilateral) and side(s) affected by the complicating condition Type of bypass Any educational information provided to the patient Location of vein or artery graft affected Treatment plan, orders, testing, prescriptions, and referrals Complications like claudication, ulceration, or chest pain Updated status of condition (stable, improved, and/or worsening) Graft, Bypass, Location, Complications, and Laterality Use the chart below to ensure that you are coding properly. Note that this is not an inclusive list of codes and that you are required to have six digits for your diagnosis code. The location and laterality will help determine the fifth and sixth digits for the codes. Type of Graft Location/Laterality Description of Graft ICD-10-CM Without -

Raynaud's Phenomenon and Erythromelalgia
Temperature-associated vascular disorders: Raynaud’s phenomenon and erythromelalgia. INTRODUCTION We are too much accustomed to attribute to a single cause that which is the product of several, and the majority of our controversies come from that. Baron Justus von Leibig (1803-73) Superficially, Raynaud's phenomenon, a disease associated with cold, and erythromelalgia, a warmth related disorder, could be considered the antithesis of each other. However, both these microcirculatory disorders, first described in the second half of the nineteenth century, have many features in common and, indeed, may share the same etiology, that is microvascular ischemia. The complicated structure that is the microcirculation can produce a variety of responses to a single noxious stimulus with sensations of cold and heat at opposite ends of the spectrum. In this chapter Raynaud's phenomenon and erythromelalgia -are compared and contrasted so that the correct diagnosis of 'these conditions and appropriate remedy can be selected by the clinician. Raynaud's Phenomenon Maurice Raynaud first defined the syndrome which bears his name 133 years ago.1 He described episodic digital ischemia provoked by cold and emotion. It is classically manifest by pallor of the affected part followed by cyanosis and rubor. Vasospasm in the digital vessels leads to the pallor (Fig. 22.1). The subsequent static venous blood leads to the development of cyanosis. The rubor is caused by hyperemia after the return of blood flow. Raynaud's phenomenon (RP) can be a benign condition but, if severe, can cause digital ulceration and gangrene. It is nine times more common in women than in men and has an overall prevalence in the population of approximately 10%, although it may affect as many as 20-30% of women in the younger age groups.2 There is also a familial predisposition which is more marked if the age of onset is less than 30 years.3 Until recently little was known about the true etiology and the extent of the disorder. -

Guideline-Management-Giant-Cell
Arthritis Care & Research Vol. 73, No. 8, August 2021, pp 1071–1087 DOI 10.1002/acr.24632 © 2021 American College of Rheumatology. This article has been contributed to by US Government employees and their work is in the public domain in the USA. 2021 American College of Rheumatology/Vasculitis Foundation Guideline for the Management of Giant Cell Arteritis and Takayasu Arteritis Mehrdad Maz,1 Sharon A. Chung,2 Andy Abril,3 Carol A. Langford,4 Mark Gorelik,5 Gordon Guyatt,6 Amy M. Archer,7 Doyt L. Conn,8 Kathy A. Full,9 Peter C. Grayson,10 Maria F. Ibarra,11 Lisa F. Imundo,5 Susan Kim,2 Peter A. Merkel,12 Rennie L. Rhee,12 Philip Seo,13 John H. Stone,14 Sangeeta Sule,15 Robert P. Sundel,16 Omar I. Vitobaldi,17 Ann Warner,18 Kevin Byram,19 Anisha B. Dua,7 Nedaa Husainat,20 Karen E. James,21 Mohamad A. Kalot,22 Yih Chang Lin,23 Jason M. Springer,1 Marat Turgunbaev,24 Alexandra Villa-Forte, 4 Amy S. Turner,24 and Reem A. Mustafa25 Guidelines and recommendations developed and/or endorsed by the American College of Rheumatology (ACR) are intended to provide guidance for particular patterns of practice and not to dictate the care of a particu- lar patient. The ACR considers adherence to the recommendations within this guideline to be voluntary, with the ultimate determination regarding their application to be made by the physician in light of each patient’s individual circumstances. Guidelines and recommendations are intended to promote beneficial or desirable outcomes but cannot guarantee any specific outcome. -

A 69-Year-Old Woman with Intermittent Claudication and Elevated ESR
756 Self-assessment corner Postgrad Med J: first published as 10.1136/pgmj.74.878.756 on 1 December 1998. Downloaded from A 69-year-old woman with intermittent claudication and elevated ESR M L Amoedo, M P Marco, M D Boquet, S Muray, J M Piulats, M J Panades, J Ramos, E Fernandez A 69-year-old woman was referred to our out-patient clinic because of long-term hypertension and stable chronic renal failure (creatinine 132 ,umol/l), which had been attributed to nephroan- giosclerosis. She presented with a one-year history of anorexia, asthenia and loss of 6 kg ofweight. In addition, she complained of intermittent claudication of the left arm and both legs lasting 2 months. This provoked important functional limitation of the three limbs, and impaired ambula- tion. She did not complain of headache or symptoms suggestive of polymyalgia rheumatica. Her blood pressure was 160/95 mmHg on the right arm and undetectable on the left arm and lower limbs. Both temporal arteries were palpable and not painful. Auscultation of both carotid arteries was normal, without murmurs. Cardiac and pulmonary auscultation were normal. Mur- murs were audible on both subclavian arteries. Neither the humeral nor the radial pulse were detectable on the left upper limb. Murmurs were also audible on both femoral arteries, and nei- ther popliteal nor distal pulses were palpable. Her feet were cold although they had no ischaemic lesions. Funduscopic examination was essentially normal. The most relevant laboratory data were: erythrocyte sedimentation rate (ESR) 120 mm/h, C-reactive protein 4.4 mg/dl (normal range <1.5); antinuclear and antineutrophil cytoplasmic antibodies were negative. -

Crohn's Disease
Harvard-MIT Division of Health Sciences and Technology HST.121: Gastroenterology, Fall 2005 Instructors: Dr. Jonathan Glickman Vascular and Inflammatory Diseases of the Intestines Overview • Vascular disorders – Vascular “malformations” – Vasculitis – Ischemic disease • Inflammatory disorders of specific etiology – Infetious enterocolitis – “Immune-mediated” enteropathy – Diverticular disease • Idiopathic inflammatory bowel disease – Crohn’s disease – Ulcerative colitis Sporadic Vascular Ectasia (Telangiectasia) • Clusters of tortuous thin-walled small vessels lacking muscle or adventitia located in the mucosa and the submucosa • The most common type occurs in cecum or ascending colon of individuals over the age of 50 and is commonly known as “angiodysplasia” • Angiodysplasias account for 40% of all colonic vascular lesions and are the most common cause of lower GI bleeding in individuals over the age of 60 Angiodysplasia Hereditary Vascular Ectasia • Hereditary Hemorrhagic Telangiectasia (HHT) or Osler- Webber-Rendu disease • Systematic disease primarily involving skin and mucous membranes, and often the GI tract • Autosomal dominant disease with positive family history in 80% of cases • After epistaxis which occurs in 80% of individuals, GI bleed is the most frequent presentation and occurs in 10-40% of cases Arteriovenous Malformations (AVM’s) • Irregular meshwork of structurally abnormal medium to large ectatic vessels • Unlike small vessel ectasias, AVM’s can be distributed in all layers of the bowel wall • AVM’s may present anywhere -

Should I Send My Patient with Previous Giant Cell Arteritis for Imaging of The
Downloaded from ard.bmj.com on January 23, 2013 - Published by group.bmj.com ARD Online First, published on December 22, 2012 as 10.1136/annrheumdis-2012-202145 Clinical and epidemiological research EXTENDED REPORT Should I send my patient with previous giant cell arteritis for imaging of the thoracic aorta? A systematic literature review and meta-analysis Sarah Louise Mackie,1 Elizabeth M A Hensor,1 Ann W Morgan,1 Colin T Pease2 ▸ Additional material is ABSTRACT together has been estimated for the Swedish popula- published online only. To view Objectives To review the literature in order to estimate tion at 0.16 per 1000 person-years in men, and 0.09 please visit the journal online (http://dx.doi.org/10.1136/ how many previously unknown thoracic aortic aneurysms per 1000 person-years in women, with a median annrheumdis-2012-202145). (TAAs) and thoracic aortic dilatations (TADs) might be age at diagnosis of 71 years and 40% overall still detected by systematic, cross-sectional aortic imaging of unruptured at diagnosis.9 Abdominal aortic aneur- 1NIHR-Leeds Musculoskeletal Biomedical Research Unit, patients with giant cell arteritis (GCA). ysm (AAA) is observed in about 5% of men over 65 10 Leeds Institute of Molecular Methods A systematic literature review was performed in ultrasound screening programmes. Medicine, Leeds, West using Ovid Medline, Embase and the Cochrane Library. Patients with GCA appear to have an elevated Yorkshire, UK Studies potentially relevant to TAA/TAD were evaluated incidence of aortic aneurysm, particularly TAA, 2Department of Rheumatology, Leeds Teaching Hospitals NHS by two authors independently for relevance, bias and compared with the general population; the aneur- Trust, Leeds, West Yorkshire, heterogeneity. -

Association Between Multi-Site Atherosclerotic Plaques and Systemic Arteriosclerosis
Association between multi-site atherosclerotic plaques and systemic arteriosclerosis: results from the BEST study (Beijing Vascular Disease Patients Evaluation Study) huan liu Peking University Shougang Hospital https://orcid.org/0000-0001-6223-7677 Jinbo Liu Peking University Shougang Hospital Wei Huang Peking University Shougang Hospital Hongwei Zhao Peking University Shougang Hospital Na zhao Peking University Shougang Hospital Hongyu wang ( [email protected] ) Research Keywords: arteriosclerosis, atherosclerosis, atherosclerotic plaque, carotid femoral artery pulse wave velocity CF-PWV Posted Date: June 8th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-31641/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Version of Record: A version of this preprint was published on August 1st, 2020. See the published version at https://doi.org/10.1186/s12947-020-00212-3. Page 1/18 Abstract Background Arteriosclerosis can be reected in various aspect of the artery, including atherosclerotic plaque formation or stiffening on the arterial wall. Both arteriosclerosis and atherosclerosis are important and closely associated with cardiovascular disease (CVD). The aim of the study was to evaluate the association between systemic arteriosclerosis and multi-site atherosclerotic plaques. Methods The study was designed as an observational cross-sectional study. A total of 1178 participants (mean age 67.4 years; 52.2% male) enrolled into the observational study from 2010 to 2017. Systemic arteriosclerosis was assessed by carotid femoral artery pulse wave velocity (CF-PWV) and multi-site atherosclerotic plaques (MAP, >=2 of the below sites) were reected in the carotid or subclavian artery, abdominal aorta and lower extremities arteries using ultrasound equipment. -

Arterial Manifestations in Young People
Arterial Manifestations in Young People Ann Marie Kupinski, PhD RVT RDMS FSVU North Country Vascular Diagnostics, Inc, & Albany Medical College, Albany, NY Objectives Describe arterial pathology encountered in young people Discuss criteria used to diagnose nonatherosclerotic disease entities Present cases which illustrate ultrasound findings of arterial disease in young people Arterial Disease in Young People • Approx. 90% of PAD and extracranial arterial disease is due to atherosclerosis • Nonatherosclerotic diseases can include: • Inflammatory diseases • Non-inflammatory diseases (FMD) • Congenital abnormalities • Acquired diseases • Injuries Testing Options • Ultrasound – Useful with large vessel disease – Giant Cell, Takayasu’s, Radiation arteritis – Injury/Trauma • Physiologic testing (PVR, PPG, pressures) – Useful with small vessel disease Buerger’s Disease (Thromboangiitis obliterans) Vasospastic Disease Fibromuscular dysplasia FMD Noninflammatory Nonatherosclerotic Young individuals (mean onset 48 yrs) Women (3:1) Affects small to medium- sized arteries Intima, media or adventitia FMD Distribution Renal 60-75% Cerebrovascular 25-30% Visceral 9% Extremity Arteries 5% Has also been observed in coronary arteries, pulmonary arteries and the aorta 28% of patients have at least two vascular beds involved Intimal fibroplasia Smooth focal stenosis with a concentric band Long smooth tubular stenosis Poloskey, et al. Circulation 2012;125 Medial fibroplasia Alternating areas of thinned media and thickened fibromuscular -

Survival After Aortic Dissection in Giant Cell Arteritis
332 Letters to the editor pressure or hypotensive episodes were technique and rating scale for abnormalities of the thorax, without intravenous contrast seen in scleroderma and related disorders. recorded during the trial. Among the side Arthritis Rheum 1981; 24: 1159-65. medium (because of asthma), showed a effects, mild flushing (35%) and headache 9 Ferri C, La Civita L, Zignego A et al. Plasma normal mediastinum but a small rim of L, Ann Rheum Dis: first published as 10.1136/ard.55.5.332 on 1 May 1996. Downloaded from (24%) were the most frequent in isradipine levels of endothelin-I in mixed cryoglobulin- pleural fluid on the left. aemia patients. Br J Rheumatol 1994; 33: recipients. 689-90. At follow up, the patient complained of This study has demonstrated the favour- 10 Yanagisawa M, Kurihara H, Kimura S, et al. A right thigh claudication. Radiofemoral delay able effects of isradipine on patients with novel potent vasoconstrictor peptide pro- was noted. CT of the abdomen showed Raynaud's phenomenon; moreover, it is the duced by vascular endothelial cells. Nature internal displacement ofcalcified atheroma in 1988; 332: 411-5. first to demonstrate a significant reduction 11 Levin E R. Endothelins [review]. N Engl J Med the aorta, suggesting aortic dissection. Mag- in plasma concentrations of ET-1 during 1995; 333: 356-63. netic resonance imaging (MRI) confirmed calcium antagonist treatment. The most this as distal to the origin of the left sub- usual manifestations of Raynaud's phenom- clavian artery, extending to the aortic bifur- enon are pain and numbness in the fingers, cation. -

Prehypertension Increases the Risk for Renal Arteriosclerosis in Autopsies: the Hisayama Study
JASN Express. Published on June 20, 2007 as doi: 10.1681/ASN.2007010067 CLINICAL EPIDEMIOLOGY www.jasn.org Prehypertension Increases the Risk for Renal Arteriosclerosis in Autopsies: The Hisayama Study Toshiharu Ninomiya,* Michiaki Kubo,* Yasufumi Doi,† Koji Yonemoto,* Yumihiro Tanizaki,* Kazuhiko Tsuruya,† Katsuo Sueishi,‡ Masazumi Tsuneyoshi,§ Mitsuo Iida,† and Yutaka Kiyohara* Departments of *Environmental Medicine, †Medicine and Clinical Science, ‡Pathophysiological and Experimental Pathology, and §Anatomic Pathology, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan ABSTRACT Information regarding the association between prehypertension BP level and renal arteriosclerosis is limited. In 652 consecutive population-based autopsy samples without hypertension treatment before death, the relationship between the severity of renal arteriosclerosis and BP levels classified according to the criteria of the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure was examined. The age- and gender-adjusted frequencies of renal arteriosclerosis linearly increased with elevating BP levels; both hypertensive and prehypertensive subjects had significantly higher frequencies of renal arteriosclerosis than subjects with normal BP (normal 11.9%; prehypertension 28.5%; stage 1 hypertension 32.9%; stage 2 hypertension 58.2%; all P Ͻ 0.01 versus normal). In a logistic regression model, prehypertension was significantly associated with renal arteriosclerosis after adjustment for other cardiovascular risk factors (prehyper- tension multivariate-adjusted odds ratio [mOR] 5.99 [95% confidence interval (CI) 2.20 to 15.97]; stage 1 hypertension mOR 6.99 [95% CI 2.61 to 18.72]; stage 2 hypertension mOR 22.21 [95% CI 8.35 to 59.08]). This significant association was observed for all renal arterial sizes. -

Thrombosis in Vasculitis: from Pathogenesis to Treatment
Emmi et al. Thrombosis Journal (2015) 13:15 DOI 10.1186/s12959-015-0047-z REVIEW Open Access Thrombosis in vasculitis: from pathogenesis to treatment Giacomo Emmi1*†, Elena Silvestri1†, Danilo Squatrito1, Amedeo Amedei1,2, Elena Niccolai1, Mario Milco D’Elios1,2, Chiara Della Bella1, Alessia Grassi1, Matteo Becatti3, Claudia Fiorillo3, Lorenzo Emmi2, Augusto Vaglio4 and Domenico Prisco1,2 Abstract In recent years, the relationship between inflammation and thrombosis has been deeply investigated and it is now clear that immune and coagulation systems are functionally interconnected. Inflammation-induced thrombosis is by now considered a feature not only of autoimmune rheumatic diseases, but also of systemic vasculitides such as Behçet’s syndrome, ANCA-associated vasculitis or giant cells arteritis, especially during active disease. These findings have important consequences in terms of management and treatment. Indeed, Behçet’syndrome requires immunosuppressive agents for vascular involvement rather than anticoagulation or antiplatelet therapy, and it is conceivable that also in ANCA-associated vasculitis or large vessel-vasculitis an aggressive anti-inflammatory treatment during active disease could reduce the risk of thrombotic events in early stages. In this review we discuss thrombosis in vasculitides, especially in Behçet’s syndrome, ANCA-associated vasculitis and large-vessel vasculitis, and provide pathogenetic and clinical clues for the different specialists involved in the care of these patients. Keywords: Inflammation-induced thrombosis, Thrombo-embolic disease, Deep vein thrombosis, ANCA associated vasculitis, Large vessel vasculitis, Behçet syndrome Introduction immunosuppressive treatment rather than anticoagulation The relationship between inflammation and thrombosis is for venous or arterial involvement [8], and perhaps one not a recent concept [1], but it has been largely investigated might speculate that also in AAV or LVV an aggressive only in recent years [2]. -
Layne14cv14.Pdf
IN THE UNITED STATES DISTRICT COURT FOR THE WESTERN DISTRICT OF VIRGINIA Harrisonburg Division CARLA R. LAYNE, ) Plaintiff, ) ) Civil Action No. 5:14cv00014 v. ) ) By: Joel C. Hoppe CAROLYN W. COLVIN, ) United States Magistrate Judge Acting Commissioner, ) Social Security Administration, ) Defendant. ) REPORT AND RECOMMENDATION Plaintiff Carla R. Layne asks this Court to review the Commissioner of Social Security’s (“Commissioner”) final decision denying her applications for disability insurance benefits (“DIB”) and supplemental security income (“SSI”) under Titles II and XVI of the Social Security Act, 42 U.S.C. §§ 401–422, 1381–1383f. This Court has authority to decide Layne’s case under 42 U.S.C. §§ 405(g) and 1383(c)(3), and her case is before me by referral under 28 U.S.C. § 636(b)(1)(B). Having considered the administrative record, the parties’ briefs and oral arguments, and the applicable law, I find that substantial evidence supports the Commissioner’s final decision that Layne is not disabled. I. Standard of Review The Social Security Act authorizes this Court to review the Commissioner’s final decision that a person is not entitled to disability benefits. See 42 U.S.C. § 405(g); Hines v. Barnhart, 453 F.3d 559, 561 (4th Cir. 2006). The Court’s role, however, is limited—it may not “reweigh conflicting evidence, make credibility determinations, or substitute [its] judgment” for that of agency officials. Hancock v. Astrue, 667 F.3d 470, 472 (4th Cir. 2012). Instead, the Court asks only whether the Administrative Law Judge (“ALJ”) applied the correct legal standards and 1 whether substantial evidence supports the ALJ’s factual findings.