Timely Care Provided
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Northern Rivers Social Profile
Northern Rivers Social Profile PROJECT PARTNER Level 3 Rous Water Building 218 Molesworth St PO Box 146 LISMORE NSW 2480 tel: 02 6622 4011 fax: 02 6621 4609 email: [email protected] web: www.rdanorthernrivers.org.au Chief Executive Officer: Katrina Luckie This paper was prepared by Jamie Seaton, Geof Webb and Katrina Luckie of RDA – Northern Rivers with input and support from staff of RDA-NR and the Northern Rivers Social Development Council, particularly Trish Evans and Meaghan Vosz. RDA-NR acknowledges and appreciates the efforts made by stakeholders across our region to contribute to the development of the Social Profile. Cover photo Liina Flynn © NRSDC 2013 We respectfully acknowledge the Aboriginal peoples of the Northern Rivers – including the peoples of the Bundjalung, Yaegl and Gumbainggirr nations – as the traditional custodians and guardians of these lands and waters now known as the Northern Rivers and we pay our respects to their Elders past and present. Disclaimer This material is made available by RDA – Northern Rivers on the understanding that users exercise their own skill and care with respect to its use. Any representation, statement, opinion or advice expressed or implied in this publication is made in good faith. RDA – Northern Rivers is not liable to any person or entity taking or not taking action in respect of any representation, statement, opinion or advice referred to above. This report was produced by RDA – Northern Rivers and does not necessarily represent the views of the Australian or New South Wales Governments, their officers, employees or agents. Regional Development Australia Committees are: Table of Contents INTRODUCTION .................................................................................................................. -

Lamington National Park Management Plan 2011
South East Queensland Bioregion Prepared by: Planning Services Unit Department of Environment and Resource Management © State of Queensland (Department of Environment and Resource Management) 2011 Copyright protects this publication. Except for purposes permitted by the Copyright Act 1968, reproduction by whatever means is prohibited without the prior written permission of the Department of Environment and Resource Management. Enquiries should be addressed to Department of Environment and Resource Management, GPO Box 2454, Brisbane Qld 4001. Disclaimer This document has been prepared with all due diligence and care, based on the best available information at the time of publication. The department holds no responsibility for any errors or omissions within this document. Any decisions made by other parties based on this document are solely the responsibility of those parties. Information contained in this document is from a number of sources and, as such, does not necessarily represent government or departmental policy. This management plan has been prepared in accordance with the Nature Conservation Act 1992. This management plan does not intend to affect, diminish or extinguish native title or associated rights. Note that implementing some management strategies might need to be phased in according to resource availability. For information on protected area management plans, visit <www.derm.qld.gov.au>. If you need to access this document in a language other than English, please call the Translating and Interpreting Service (TIS National) on 131 450 and ask them to telephone Library Services on +61 7 3224 8412. This publication can be made available in alternative formats (including large print and audiotape) on request for people with a vision impairment. -

Weekly Markets Continued Byron Bay Artisan Market Caldera Farmers
Weekly Markets Weekly Markets continued 1st Weekend of the Month Continued Lismore Produce Market Byron Bay Artisan Market Make It Bake It Grow It Market Magellan St (between Carrington & Molesworth St, Lismore CBD) Railway Park, Johnson St Byron Bay Summerland House Farm, 253 Wardell Road, Alstonville 02 6622 5141 02 6685 6807 (Tess Cullen) 0417 547 555 Every Thursday 3.30pm - 7pm w: byronmarkets.com.au/artisan.html w:makeitbakeitgrowit.com.au from October - Easter only, Saturdays 4pm - 9pm 1st Sunday 9am - 1pm Lismore Organic Market Lismore Showground, Caldera Farmers Market Kyogle Bazaar 02 6636 4307 Murwillumbah Showground Kyogle CBD w: tropo.org.au 02 6684 7834 0416 956 744 Every Tuesday 7.30am - 11am w: calderafarmersmarket.com.au 1st & 3rd Saturdays 8am - 4pm Every Wednesday 7am - 11am Lismore Farmers Market 2nd Weekend of the Month Lismore Showground, Nth Lismore Mullumbimby Farmers Market The Channon Craft Market 02 6621 3460 Mullumbimby Showground, 51 Main Arm Rd, Mullumbimby Coronation Park, The Channon Every Saturday 8am - 11am 02 6684 5390 02 6688 6433 w: mullumfarmersmarket.org.au w: thechannonmarket.org.au Nimbin Farmers Market Every Friday 7am - 11am e: [email protected] Next to The Green Bank, Cullen St, Nimbin 2nd Sunday 9am - 3pm 02 6689 1512 (Jason) Uki Produce Market Every Wednesday 3pm - 6pm Uki Hall, Uki Alstonville Market 02 6679 5438 Apex Pavilion, Alstonville Showground (undercover) Alstonville Farmers Market Every Saturday 8am - 12pm 02 6628 1568 Bugden Ln, opp Federal Hotel, behind Quattro, Alstonville -

Here for Acon Northern Rivers
HERE FOR ACON NORTHERN RIVERS This guide can be shared online and printed. To add or edit a listing please contact ACON Northern Rivers NORTHERN RIVERS LOCAL LGBTI SOCIAL AND SUPPORT GROUPS AllSorts LGBTIQ and Gender Tropical Fruits Inc. Trans and Gender Diverse Diverse Youth Group on the 6622 6440 | www.tropicalfruits.org.au Social Group, Lismore Tweed Facebook - The Tropical Fruits Inc Mal Ph: 0422 397 754 Tammie Ph: 07 5589 1800 | 0439 947 566. Social events and support for LGBTIQ and friends [email protected] Meets monthly for LGBTI & gender diverse A monthly casual get-together for transgender, young people aged16 to 24 years in the Tweed Queer Beers Brunswick Heads gender diverse, gender non-conforming or gender questioning people, sistergirls and Compass Tweed/Southern Facebook - queer-beers brotherboys Gold Coast LGBTIQAP+ Youth Mixed -Gender, monthly social in the beer garden at the Brunswick Heads Hotel Men’s Lounge, Lismore Network Queer Beers Lismore Russell Ph: 0481 117 121 Claire Ph: 07 5589 8700 [email protected] [email protected] Facebook - queerbeerslismore A group of gay and bisexual men who meet at Compass is a youth-driven network of Good company, food, drinks & beats on the the Tropical Fruit Bowl in South Lismore on the community members and service providers 4th Sunday of every month, 4-8pm for the second Friday of each month uniting to provide safety, support, acceptance LGBTIQ community at the Northern Rivers Hotel and celebration for LGBTIQAP+ young people North Lismore Gay Tennis in Mullumbimby in the Tweed Shire and Southern Gold Coast Lismore Lads Club Lunch Contact ACON Northern Rivers Fresh Fruits LGBTIQ 6622 1555 | [email protected] Facebook - lismorelad’sclub Social Group A long running social tennis group that meets A monthly social get together of gay guys Wednesday nights, 6pm at the Mullumbimby 6625 0200 living with or affected by HIV, and our friends Tennis Courts and supporters. -

MARKET GUIDE All Year Round
Markets Vibrant, rhythmic, tantalising and colourful markets abound in the creative groundswell of the Northern Rivers region. Escape to the Northern Rivers of NSW and NORTHERN RIVERS discover stunning natural attractions, gorgeous beaches, quality restaurants and vibrant markets MARKET GUIDE all year round. From handcrafted art and homeware, to delicious, healthy and multicultural foods and unique and vintage fashion, Northern Rivers markets are an ideal place to shop, dine and be entertained while spending time in this beautiful region. There is a Northern Rivers market every weekend, each with their own vibe and array of quality local produce to delight any shopper. Popular as a meeting place for locals and as a day out for families, Northern Rivers markets are an exciting place to be. CONTACT US: p: 6660 0325 e: [email protected] w: www.discoverrichmondvalley.com.au 1st Sunday of the 4th Sunday of the Northern Rivers Market Guide month month Every Friday Byron Bay Community Market Bangalow Market Every Tuesday 1st Saturday of the 4th Saturday of the 8am - 3pm 9am - 3pm month Butler Street Reserve, Byron Bay Bangalow Showgrounds New Brighton Farmers Market Mullumbimby Farmers Market month 7am - 11am 8am - 11am Brunswick Heads Riverside Market Evans Head Riverside Market Lismore Car Boot Market Nimbin Market Mullumbimby Showground, River Street 7.00am - 2pm 7.30am - 1.30pm 7.30am - 2pm 9am -3pm Main Arm Road Memorial Park, Fawcett Street, Ballina Lismore Shopping Square Nimbin Community Centre Lismore Organic Market Club -
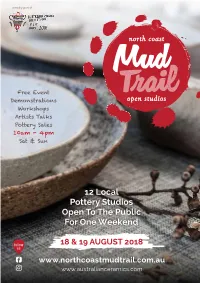
12 Local Pottery Studios Open to the Public for One Weekend
proudly part of Free Event Demonstrations Workshops Artists Talks Pottery Sales 10am - 4pm Sat & Sun 12 Local Pottery Studios Open To The Public For One Weekend follow 18 & 19 AUGUST 2018 us www.northcoastmudtrail.com.au www.australianceramics.com Sasa Scheiner August 2018 Sat 18 & Sun 19 10am to 4pm www.northcoastmudtrail.com.au Welcome! The Northern Rivers is a vibrant creative community that is fast becoming known as a major centre for Ceramic Arts. The region is a hub for traditional and contemporary ceramic artists and potters, some long standing locals, and a growing population of new talents. The diverse works crafted by these artisans are coveted by enthusiasts from all over the world, with pieces by many of the artists in galleries, retail outlets, restaurants, and private collections in America, Asia and Europe. Once a year, as part of The Australian Ceramics Association’s Open Studios, these artists open their spaces to the public for one weekend only, giving the opportunity for visitors to see demonstrations, hear artists’ talks, participate in workshops, learn about their processes, and purchase ceramics directly from the artists themselves. There will be thousands of beautiful pieces made with multiple methods and diverse finishes, as varied as the potters themselves. Whether you are looking for a fun piece of brightly coloured tableware, a decorative masterpiece, or a simple classic, perhaps a woodfired sculpture, or an alternatively fired gem, whatever your taste, there is a work of art perfect for everyone waiting to be discovered. Come along, have some fun, and pick up a piece of local treasure… North Coast Ceramics INC. -

RAIL TRAILS for NSW ABN 43 863 190 337 - a Not for Profit Charity
RAIL TRAILS FOR NSW ABN 43 863 190 337 - A Not for Profit Charity Chairman John Moore OAM RFD ED M. 0403 160 750 [email protected] Deputy Chairman Tim Coen B.Com. M. 0408 691 541 [email protected] Website: railtrailsnsw.com.au facebook: Facebook.com/railtrailsnsw NSW will generate up to $74 million every year create up to 290 jobs revitalise 90+ regional communities by building these tourism assets Submission for the 2020 NSW Budget Rail Trails for NSW August 2020 EXECUTIVE SUMMARY This submission champions 11 high quality tourist trail projects for regional NSW totalling 884 kilometres of safe, scenic, vehicle-free pathway on publicly owned, decades out of service, regional rail corridors. There are no prospects for re-activated train services along any of the nominated routes. Rail Trails for NSW urges the State Government to seek co-contributions from the Australian Government for the projects. The building of these tourist trails will provide: • Fiscal stimulus of up to $3.3 million for feasibility and other pre-construction studies and planning • Fiscal stimulus during the trail construction phase of up to $271,250,000 • Upon completion; o All 14 regional trails will generate additional local visitor spending estimated conservatively at $27 million p.a. building to $74 million p.a. o Steadily create up to 111 jobs building to 297 or more local jobs as visitor numbers grow o facilitate new business and employment opportunities in their host regions o provide community, health and exercise resources for locals o enable social benefits by generating community resilience, hope and optimism o stimulus of up to $2.75 million via marketing and promotion activities These 11 additional rail trails warranting immediate attention (Table 1). -

Discussion Paper V7
NORTHERN RIVERS REGIONAL AFFORDABLE HOUSING STRATEGY BACKGROUND DISCUSSION, RECOMMENDATIONS & STRATEGY SUPPORT Authors Social Habitat September 2012 TABLE OF CONTENTS Page GLOSSARY OF TERMS 4 PART A – BACKGROUND DISCUSSION 5 1 INTRODUCTION 5 2 DEFINING AFFORDABLE HOUSING AND HOUSING STRESS 6 2.1 National Affordable Housing Summit Group 6 2.2 Commonwealth Government 6 2.3 State Government 7 2.4 Local Government 7 2.5 Strategy 8 3 REVIEW OF LOCAL HOUSING STRATEGIES 9 3.1 Overview 9 3.2 Ballina Shire Council 9 3.3 Byron Shire Council 10 3.4 Clarence Valley Council 10 3.5 Lismore City Council 11 3.6 Tweed Shire Council 12 4 RESEARCH OTHER STRATEGIES 13 4.1 Overview 13 4.2 Sunshine Coast Affordable Living Strategy 2010-2020 13 4.3 Affordable Housing Strategy 2010-2020 (WA Government) 13 5 CONSULTATION AND OUTCOMES 14 5.1 Overview – consultation plan and storyboard 14 5.2 Consultation with Councils 14 5.2.1 Meetings with Councils 14 5.2.2 Survey of Councils 14 5.3 Consultation with Steering Committee 14 5.4 Consultation with Community Housing 14 5.5 Other consultations 15 6 REVIEW OF STATISTICAL DATA 16 6.1 Overview 16 6.2 Northern Rivers region 16 6.3 Ballina Shire Council 17 6.4 Byron Shire Council 18 6.5 Clarence Valley Council 19 6.6 Kyogle Council 20 6.7 Lismore City Council 21 6.8 Richmond Valley Council 22 6.9 Tweed Shire Council 23 6.10 Dept. of Housing Rent and Sales Report 24 7 LAND USE PLANNING REVIEW 7.1 Review of changes to the NSW planning system 25 7.2 Review of State Environmental Planning Policies 29 7.3 Review of Local Environmental -

630 Bus Time Schedule & Line Route
630 bus time schedule & line map 630 Murwillumbah to Nimbin (Loop Service) View In Website Mode The 630 bus line Murwillumbah to Nimbin (Loop Service) has one route. For regular weekdays, their operation hours are: (1) Murwillumbah: 7:35 AM - 2:20 PM Use the Moovit App to ƒnd the closest 630 bus station near you and ƒnd out when is the next 630 bus arriving. Direction: Murwillumbah 630 bus Time Schedule 16 stops Murwillumbah Route Timetable: VIEW LINE SCHEDULE Sunday Not Operational Monday 7:35 AM - 2:20 PM Brisbane St opp Sunnyside Mall Knox Park Footpath, Murwillumbah Tuesday 7:35 AM - 2:20 PM Kyogle Rd opp Mt Warning Rd Wednesday 7:35 AM - 2:20 PM Kyogle Rd opp Uki Public School Thursday 7:35 AM - 2:20 PM 1464 Kyogle Road, Uki Friday 7:35 AM - 2:20 PM Kyogle Rd opp Ted Brown Cl Saturday Not Operational 2759 Kyogle Road, Mount Burrell Kyogle Rd opp Mount Burrell Store Kyogle Rd at Stringybark Rd 630 bus Info Direction: Murwillumbah Nimbin Rd opp Blue Knob Hall Stops: 16 715 Blue Knob Road, Blue Knob Trip Duration: 135 min Line Summary: Brisbane St opp Sunnyside Mall, Nimbin Central School Kyogle Rd opp Mt Warning Rd, Kyogle Rd opp Uki Public School, Kyogle Rd opp Ted Brown Cl, Kyogle Cullen St before Thorburn St Rd opp Mount Burrell Store, Kyogle Rd at Stringybark 80 Cullen Street, Nimbin Rd, Nimbin Rd opp Blue Knob Hall, Nimbin Central School, Cullen St before Thorburn St, Blue Knob Hall, Blue Knob Hall, Nimbin Rd Nimbin Rd, Kyogle Rd at Cadell Rd, Mount Burrell 715 Blue Knob Road, Blue Knob Store, Kyogle Rd, Kyogle Rd opp Cooloon St, Kyogle Rd opp Uki Public School, Kyogle Rd after Mt Kyogle Rd at Cadell Rd Warning Rd, Brisbane St opp Sunnyside Mall Mount Burrell Store, Kyogle Rd 3220 Kyogle Road, Mount Burrell Kyogle Rd opp Cooloon St 2 Ted Brown Close, Mount Burrell Kyogle Rd opp Uki Public School 1464 Kyogle Road, Uki Kyogle Rd after Mt Warning Rd 1022 Kyogle Road, Byangum Brisbane St opp Sunnyside Mall Knox Park Footpath, Murwillumbah 630 bus time schedules and route maps are available in an o«ine PDF at moovitapp.com. -

Sydney - Brisbane Land Transport
University of Wollongong Research Online Faculty of Engineering and Information Faculty of Informatics - Papers (Archive) Sciences 1-1-2007 Sydney - Brisbane Land Transport Philip G. Laird University of Wollongong, [email protected] Follow this and additional works at: https://ro.uow.edu.au/infopapers Part of the Physical Sciences and Mathematics Commons Recommended Citation Laird, Philip G.: Sydney - Brisbane Land Transport 2007, 1-14. https://ro.uow.edu.au/infopapers/760 Research Online is the open access institutional repository for the University of Wollongong. For further information contact the UOW Library: [email protected] Sydney - Brisbane Land Transport Abstract This paper shall commence with reference to the draft AusLink Sydney - Brisbane corridor strategy. Section 2 will outline the upgrading of the Pacific Highway, Section 3 will examine the existing Sydney - Brisbane railway whilst Section 4 will outline some 2009 - 2014 corridor upgrade options with particular attention to external costs and energy use as opposed to intercity supply chain costs. The conclusions are given in Section 5. The current population of the coastal regions of the Sydney - Brisbane corridor exceeds 8 million. As shown by Table I, the population is expected to be approaching 11 million by 2031. The draft strategy notes that Brisbane and South East Queensland will become Australia's second largest conurbation by 2026. Keywords land, transport, brisbane, sydney Disciplines Physical Sciences and Mathematics Publication Details Laird, P. G. (2007). Sydney - Brisbane Land Transport. Australasian Transport Research Forum (pp. 1-14). Online www.patrec.org - PATREC/ATRF. This conference paper is available at Research Online: https://ro.uow.edu.au/infopapers/760 Sydney - Brisbane land transport Sydney - Brisbane Land Transport Philip Laird University of Wollongong, NSW, Australia 1 Introduction This paper shall commence with reference to the draft AusLink Sydney - Brisbane corridor strategy. -

Police Close in on Prime Cudgen Land
THE TWEED Volume 2 #43 Thursday, July 8, 2010 Page Advertising and news enquiries: 10 Phone: (02) 6672 2280 [email protected] [email protected] www.tweedecho.com.au LOCAL & INDEPENDENT Police close in on prime Cudgen land Ken Sapwell exhibition until July 14, is expected to trigger a swag of objections from The NSW Police Force is seeking to community and environmental exploit a loophole in planning laws groups who have been involved in a to establish a new police station on long-running battle to save the red- protected farm land at Cudgen. soil plateau from development. The move is the first serious chal- It’s also being watched closely by lenge to the Cudgen plateau’s unique other emergency service agencies who agricultural status since the Anglican have been searching for a flood-free Church lost a court battle to build a site to consolidate their operations in school on another nearby parcel of a so-called super-centre close to the prime farming land about 12 years ago geographic centre of the shire. (see panel, page 2). Former long-serving Mayor Max Senior police say the station is an Boyd, who was part of a 10-man study Karen Oliver as Eliza Doolittle in her Ascot finery.Photo supplied emergency facility which can be built team which resulted in the govern- on the site without the consent of ment classifying the plateau as agri- Tweed council or the government if cultural land of State significance, says Karen’s Directed by respected Gold Coast erful voices on the Tweed Coast, they can convince them that no other he’s confident the government will show producer Tracey Kriz and co- this production is a nice piece of suitable sites are available. -

Agenda of Lismore City Council
Council An Ordinary Meeting of Lismore City Council will be held at the Council Chambers on Tuesday, 9 February 2021 at 6pm Members of Council are requested to attend. Lismore City Council acknowledges the people of the Bundjalung nation, traditional custodians of the land on which we work. Shelley Oldham General Manager 4 February 2021 Agenda 1. Opening of Meeting 2. Acknowledgement of Country 3. Local Government – Pause for personal reflection 4. Apologies and Leave of Absence 5. Confirmation of Minutes of Previous Meeting Lismore City Council held 8 December, 2020 ................................................................................ 147 Lismore City Council held 8 December, 2020 ................................................................................ 164 6. Disclosure of Interest 7. Public Access Session on Agenda Items 8. Mayoral Minute(s) and Condolence Motions 9. Notice of Rescission Motions 10. Notice of Motions 10.1 Parking in the Lismore Base Hospital Precinct ....................................................................... 5 10.2 Parking in the Lismore Base Hospital Precinct ....................................................................... 7 10.3 72 Riverbank Road Monaltrie ................................................................................................. 9 10.4 Access Protocols .................................................................................................................. 11 11. Questions for Next Meeting 12. Altering Order of Business (Consideration of altering