Department of Botany University of Peshawar, Peshawar Pakistan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Carmona Retusa Carmona Boraginaceae
Carmona retusa Carmona Boraginaceae Forest Starr, Kim Starr, and Lloyd Loope United States Geological Survey--Biological Resources Division Haleakala Field Station, Maui, Hawai'i January, 2003 OVERVIEW Carmona retusa is a popular ornamental plant cultivated in Hawai'i as a hedge or specimen plant. On Maui, C. retusa is observed in residential plantings, mostly in low elevation neighborhoods, such as Kahului, Wailuku, Lahaina, Paia, Haiku, and Kihei. Seedlings and naturalized plants are also commonly observed in landscaping areas and wild semi-wild areas nearby plantings. In one area in Waiehu, C. retusa forms a dense shrubby understory in a kiawe (Prosopis pallida) forest. This plant is fairly widespread on Maui and is probably beyond the eradication stage. Future efforts should be aimed at monitoring, preventing infestations in natural areas, and educating the public about harmful plants that spread beyond the confines of the garden. TAXONOMY Family: Boraginaceae (Heliotrope family) (Lorence et al. 1995, Wagner et al. 1999). Latin name: Carmona retusa (Vahl) Masamune (Lorence et al. 1995, Wagner et al. 1999). Synonyms: C. microphylla (Lam.) Don; Ehretia microphylla Lam.; Ehretia buxifolia Roxb.; Cordia retusa Vahl (Lorence et al. 1995; Bailey and Bailey 1976; GRIN 2001). Common names: Carmona, Philippine tea (Bailey and Bailey 1976), Fukien tea (Caine and Zane 2001). Taxonomic notes: The genus Carmona, also commonly known as Ehretia, is comprised of about 50 species of evergreen or deciduous shrubs and trees of tropical and subtropical regions of both the New and Old World (Bailey and Bailey 1976). Related species in Hawai'i: Neal (1965) lists Ehretia acuminata R. -

Proceedings Amurga Co
PROCEEDINGS OF THE AMURGA INTERNATIONAL CONFERENCES ON ISLAND BIODIVERSITY 2011 PROCEEDINGS OF THE AMURGA INTERNATIONAL CONFERENCES ON ISLAND BIODIVERSITY 2011 Coordination: Juli Caujapé-Castells Funded and edited by: Fundación Canaria Amurga Maspalomas Colaboration: Faro Media Cover design & layout: Estudio Creativo Javier Ojeda © Fundación Canaria Amurga Maspalomas Gran Canaria, December 2013 ISBN: 978-84-616-7394-0 How to cite this volume: Caujapé-Castells J, Nieto Feliner G, Fernández Palacios JM (eds.) (2013) Proceedings of the Amurga international conferences on island biodiversity 2011. Fundación Canaria Amurga-Maspalomas, Las Palmas de Gran Canaria, Spain. All rights reserved. Any unauthorized reprint or use of this material is prohibited. No part of this book may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system without express written permission from the author / publisher. SCIENTIFIC EDITORS Juli Caujapé-Castells Jardín Botánico Canario “Viera y Clavijo” - Unidad Asociada CSIC Consejería de Medio Ambiente y Emergencias, Cabildo de Gran Canaria Gonzalo Nieto Feliner Real Jardín Botánico de Madrid-CSIC José María Fernández Palacios Universidad de La Laguna SCIENTIFIC COMMITTEE Juli Caujapé-Castells, Gonzalo Nieto Feliner, David Bramwell, Águedo Marrero Rodríguez, Julia Pérez de Paz, Bernardo Navarro-Valdivielso, Ruth Jaén-Molina, Rosa Febles Hernández, Pablo Vargas. Isabel Sanmartín. ORGANIZING COMMITTEE Pedro -
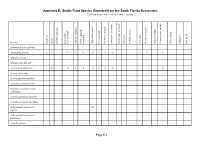
MSRP Appendix E
Appendix E. Exotic Plant Species Reported from the South Florida Ecosystem. Community types are indicated where known Species High Pine Scrub Scrubby high pine Beach dune/ Coastal strand Maritime hammock Mesic temperate hammock Tropical hardwood Pine rocklands Scrubby flatwoods Mesic pine flatwoods Hydric pine flatwoods Dry prairie Cutthroat grass Wet prairie Freshwater marsh Seepage swamp Flowing water swamp Pond swamp Mangrove Salt marsh Abelmoschus esculentus Abrus precatorius X X X X X X X X X X X X Abutilon hirtum Abutilon theophrasti Acacia auriculiformis X X X X X X X X X Acacia retinoides Acacia sphaerocephala Acalypha alopecuroidea Acalypha amentacea ssp. wilkesiana Acanthospermum australe Acanthospermum hispidum Achyranthes aspera var. X aspera Achyranthes aspera var. pubescens Acmella pilosa Page E-1 Species High Pine Scrub Scrubby high pine Beach dune/ Coastal strand Maritime hammock Mesic temperate hammock Tropical hardwood Pine rocklands Scrubby flatwoods Mesic pine flatwoods Hydric pine flatwoods Dry prairie Cutthroat grass Wet prairie Freshwater marsh Seepage swamp Flowing water swamp Pond swamp Mangrove Salt marsh Acrocomia aculeata X Adenanthera pavonina X X Adiantum anceps X Adiantum caudatum Adiantum trapeziforme X Agave americana Agave angustifolia cv. X marginata Agave desmettiana Agave sisalana X X X X X X Agdestis clematidea X Ageratum conyzoides Ageratum houstonianum Aglaonema commutatum var. maculatum Ailanthus altissima Albizia julibrissin Albizia lebbeck X X X X X X X Albizia lebbeckoides Albizia procera Page -

Università Degli Studi Di Milano
UNIVERSITÀ DEGLI STUDI DI MILANO Dottorato in Scienze Farmacologiche Sperimentali e Cliniche XXXII ciclo Dipartimento di Scienze Farmacologiche e Biomolecolari VALIDATION OF PLANTS TRADITIONALLY USED FOR SKIN INFLAMMATION Settore Scientifico Disciplinare BIO/14 Saba KHALILPOUR Tutor: Prof. Mario DELL’AGLI Coordinatore: Prof. Alberico L. CATAPANO A.A. 2018 - 2019 1 TABLE OF CONTENTS TABLE OF CONTENTS .........................................................................................2 LIST OF ABBREVIATIONS ..................................................................................6 LIST OF SYMBOLS ...............................................................................................8 RIASSUNTO ...........................................................................................................9 ABSTRACT ...........................................................................................................12 CHAPTER ONE ....................................................................................................15 1. Introduction ...........................................................................................15 1.1 Basic structure and functions of the skin .........................................................15 1.1.1 Epidermis .................................................................................16 1.1.1.1 Keratinocytes ......................................................................18 1.1.1.2 Other cell types ..................................................................19 -

Highly Cytotoxic Kettapeptin, Bhimamycins Possessing Unusual Chromophores and Further New Secondary Metabolites from Terrestrial and Marine Bacteria
Serge Fotso ___________________________________________________ Highly Cytotoxic Kettapeptin, Bhimamycins Possessing Unusual Chromophores and Further New Secondary Metabolites from Terrestrial and Marine Bacteria CH 3 O OH H C O CH 3 OH 3 CH CH CH O 3 3 3 NH HN CH3 N CH HO 3 O O O N O MeO O H CH N 3 O N N OH H3C HN O H3C H3C OH O O O CH3 O N O O CH OH O CH3 HO 3 OH Dissertation Highly Cytotoxic Kettapeptin, Bhimamycins Possessing Unusual Chromophores and Further New Secondary Metabolites from Terrestrial and Marine Bacteria Dissertation zur Erlangung des Doktorgrades der Mathematisch-Naturwissenschaftlichen Fakultäten der Georg-August-Universität zu Göttingen vorgelegt von Serge Fotso aus Yaoundé (Kamerun) Göttingen 2005 D7 Referent: Prof. Dr. H. Laatsch Korreferent: Prof. Dr. A. Zeeck Tag der mündlichen Prüfung: 02.11.2005 Die vorliegende Arbeit wurde in der Zeit von Oktober 2001 bis September 2005 im Institut für Organische Chemie der Georg-August-Universität zu Göttingen unter der Leitung von Herrn Prof. Dr. H. Laatsch angefertigt. Herrn Prof. Dr. H. Laatsch danke ich für die Möglichkeit zur Durchführung dieser Arbeit sowie die ständige Bereitschaft, auftretende Probleme zu diskutieren. Für meine Eltern und meine Verlobte I 1 Introduction...................................................................................................... 1 1.1 New drugs from the Sea............................................................................. 1 2 Aim of the present work................................................................................ -

Godere (Ethiopia), Budongo (Uganda) and Kakamega (Kenya)
EFFECTS OF ANTHROPOGENIC DISTURBANCE ON THE DIVERSITY OF FOLIICOLOUS LICHENS IN TROPICAL RAINFORESTS OF EAST AFRICA: GODERE (ETHIOPIA), BUDONGO (UGANDA) AND KAKAMEGA (KENYA) Dissertation Zur Erlangung des akademischen Grades eines Doktors der Naturwissenschaft Fachbereich 3: Mathematik/Naturwissenschaften Universität Koblenz-Landau Vorgelegt am 23. Mai 2008 von Kumelachew Yeshitela geb. am 11. April 1965 in Äthiopien Referent: Prof. Dr. Eberhard Fischer Korreferent: Prof. Dr. Emanuël Sérusiaux In Memory of my late mother Bekelech Cheru i Table of Contents Abstract……………………………………………………………………………….......…...iii Chapter 1. GENERAL INTRODUCTION.................................................................................1 1.1 Tropical Rainforests .........................................................................................................1 1.2 Foliicolous lichens............................................................................................................5 1.3 Objectives .........................................................................................................................8 Chapter 2. GENERAL METHODOLOGY..............................................................................10 2.1 Foliicolous lichen sampling............................................................................................10 2.2 Foliicolous lichen identification.....................................................................................10 2.3 Data Analysis..................................................................................................................12 -
Ecological Report on Magombera Forest
Ecological Report on Magombera Forest Andrew R. Marshall (COMMISSIONED BY WORLD WIDE FUND FOR NATURE TANZANIA PROGRAMME OFFICE) Feb 2008 2 Contents Abbreviations and Acronyms 3 Acknowledgements 4 Executive Summary 5 Background 5 Aim and Objectives 5 Findings 6 Recommendations 7 Introduction 9 Tropical Forests 9 Magombera Location and Habitat 9 Previous Ecological Surveys 10 Management and Conservation History 11 Importance of Monitoring 14 Aim and Objectives 15 Methods 15 Threats 17 Forest Structure 17 Key Species 18 Forest Restoration 20 Results and Discussion 21 Threats 21 Forest Structure 25 Key Species 26 Forest Restoration 36 Recommendations 37 Immediate Priorities 38 Short-Term Priorities 40 Long-Term Priorities 41 References 44 Appendices 49 Appendix 1. Ministry letter of support for the increased conservation of Magombera forest 49 Appendix 2. Datasheets 50 Appendix 3. List of large trees in Magombera Forest plots 55 Appendix 4. Slides used to present ecological findings to villages 58 Appendix 5. Photographs from village workshops 64 3 Abbreviations and Acronyms CEPF Critical Ecosystem Partnership Fund CITES Convention on the International Trade in Endangered Species IUCN International Union for the Conservation of Nature and Natural Resources TAZARA Tanzania-Zambia Railroad UFP Udzungwa Forest Project UMNP Udzungwa Mountains National Park WWF-TPO Worldwide Fund for Nature – Tanzania Programme Office 4 Acknowledgements Thanks to all of the following individuals and institutions: - CEPF for 2007 funds for fieldwork and report -
Avaliação Da Atividade Esquistossomicida in Vitro De Extratos, Metabólito E Óleo Essencial De Artemisia Absinthium L
UNIVERSIDADE FEDERAL DE JUIZ DE FORA FACULDADE DE FARMÁCIA PROGRAMA DE PÓS-GRADUAÇÃO EM CIÊNCIAS FARMACÊUTICAS MESTRADO EM CIÊNCIAS FARMACÊUTICAS Luísa Maria Silveira de Almeida Avaliação da atividade esquistossomicida in vitro de extratos, metabólito e óleo essencial de Artemisia absinthium L. (Asteraceae) Juiz de Fora 2015 Luísa Maria Silveira de Almeida Avaliação da atividade esquistossomicida in vitro de extratos, metabólito e óleo essencial de Artemisia absinthium L. (Asteraceae) Dissertação submetida ao Programa de Pós-graduação em Ciências Farmacêuticas, da Universidade Federal de Juiz de Fora - UFJF, como parte dos requisitos necessários à obtenção do título de Mestre em Ciências Farmacêuticas – Área de concentração: Bioprospecção de Produtos Naturais. Orientador: Prof. Dr. Ademar Alves da Silva Filho Juiz de Fora 2015 Ficha catalográfica elaborada através do programa de geração automática da Biblioteca Universitária da UFJF, com os dados fornecidos pelo(a) autor(a) Almeida, Luísa Maria Silveira de. Avaliação da atividade esquistossomicida in vitro de extratos, metabólito e óleo essencial de Artemisia absinthium L. (Asteraceae) / Luísa Maria Silveira de Almeida. -- 2015. 130 f. : il. Orientador: Ademar Alves da Silva Filho Dissertação (mestrado acadêmico) - Universidade Federal de Juiz de Fora, Faculdade de Farmácia e Bioquímica. Programa de Pós-Graduação em Ciências Farmacêuticas, 2015. 1. Esquistossomose. 2. Produtos Naturais. 3. Artemisia absinthium L.. 4. Esquistossomicida. 5. Flavona. I. Silva Filho, Ademar Alves da, orient. II. Título. Avaliação da atividade esquistossomicida in vitro de extratos, metabólito e óleo de essencial de Artemisia absinthium L. (Asteraceae) Luísa Maria Silveira de Almeida ORIENTADOR: Prof. Dr. Ademar Alves da Silva Filho Dissertação de Mestrado submetida ao Programa de Pós-Graduação em Ciências Farmacêuticas, da Universidade Federal de Juiz de Fora - UFJF, como parte dos requisitos necessários à obtenção do título de Mestre em Ciências Farmacêuticas. -

ETHNOBOTANICAL STUDIES on the FAMILY BORAGINACEAE AMONG TRIBALS in KERALA T. Jose and VT Antony
Vidyabharati International Interdisciplinary Research Journal 12(2) 44 - 4 7 ISSN 2319-4979 ETHNOBOTANICAL STUDIES ON THE FAMILY BORAGINACEAE AMONG TRIBALS IN KERALA T. Jose1 and V.T Antony2 1Centre for Research and Evaluation, Bharathiar University, Coimbatore, TN, India 2Research and Development Centre, S.B. College, Changanacherry, Kottayam, Kerala, India [email protected] ________________________________________________________________________________ ABSTRACT Ethnobotany is the branch of science that embraces the study and evaluation of interdependence among humans and the flora in all facets of life. Currently ethnobotany have stretched out its zone of study into diverse spheres like archaeology, anthropology, economics, ecology, medicine, cultural, religious and many more directions. A significant portion of the human race still depends on the traditional treatment systems for many ailments. The present study is an attempt to grab and document ethnobotanical information’s concerning the family Boraginaceae. 20 tribal groups across the state Kerala have been screened for grasping the ethnobotanical figures. A total of 6 members of the family Boraginaceae are used by the 10 tribal groups across the state of Kerala for treating various ailments. Considering the varied treatment modalities that have been espoused by discrete tribal clutches, the distinct medicinal formulations are practiced. The study have collected and recorded significant ethnobotanical data that will be a footing stone for new research and innovations in drug industry. ________________________________________________________________________________ Keywords: Ethnobotany, Boraginaceae, Kerala, Tribal, Indigenous. Introduction individual family of the order Boraginales J.W. Harshberger (1895) introduced the term among the Asterids. According to George ethnobotany to specify plants utilized by the Benthem and Joseph Dalton Hooker, indigenous populations. -

Forestry Department Food and Agriculture Organization of the United Nations
Forestry Department Food and Agriculture Organization of the United Nations Forest Health & Biosecurity Working Papers Case Studies on the Status of Invasive Woody Plant Species in the Western Indian Ocean 2. The Comoros Archipelago (Union of the Comoros and Mayotte) By P. Vos Forestry Section, Ministry of Environment & Natural Resources, Seychelles May 2004 Forest Resources Development Service Working Paper FBS/4-2E Forest Resources Division FAO, Rome, Italy Disclaimer The FAO Forestry Department Working Papers report on issues and activities related to the conservation, sustainable use and management of forest resources. The purpose of these papers is to provide early information on on-going activities and programmes, and to stimulate discussion. This paper is one of a series of FAO documents on forestry-related health and biosecurity issues. The study was carried out from November 2002 to May 2003, and was financially supported by a special contribution of the FAO-Netherlands Partnership Programme on Agro-Biodiversity. The designations employed and the presentation of material in this publication do not imply the expression of any opinion whatsoever on the part of the Food and Agriculture Organization of the United Nations concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Quantitative information regarding the status of forest resources has been compiled according to sources, methodologies and protocols identified and selected by the author, for assessing the diversity and status of forest resources. For standardized methodologies and assessments on forest resources, please refer to FAO, 2003. State of the World’s Forests 2003; and to FAO, 2001. -

Plant Biodiversity of Zarm-Rood Rural
ﻋﺒﺎس ﻗﻠﯽﭘﻮر و ﻫﻤﮑﺎران داﻧﺸﮕﺎه ﮔﻨﺒﺪ ﮐﺎووس ﻧﺸﺮﯾﻪ "ﺣﻔﺎﻇﺖ زﯾﺴﺖ ﺑﻮم ﮔﯿﺎﻫﺎن" دوره ﭘﻨﺠﻢ، ﺷﻤﺎره دﻫﻢ، ﺑﻬﺎر و ﺗﺎﺑﺴﺘﺎن 96 http://pec.gonbad.ac.ir ﺗﻨﻮع ﮔﯿﺎﻫﯽ دﻫﺴﺘﺎن زارمرود، ﺷﻬﺮﺳﺘﺎن ﻧﮑﺎ (ﻣﺎزﻧﺪران) ﻋﺒﺎس ﻗﻠﯽﭘﻮر1*، ﻧﺴﯿﻢ رﺳﻮﻟﯽ2، ﻣﺠﯿﺪ ﻗﺮﺑﺎﻧﯽ ﻧﻬﻮﺟﯽ3 1داﻧﺸﯿﺎر ﮔﺮوه زﯾﺴﺖﺷﻨﺎﺳﯽ، داﻧﺸﮑﺪه ﻋﻠﻮم، داﻧﺸﮕﺎه ﭘﯿﺎم ﻧﻮر، ﺗﻬﺮان 2 داﻧﺶآﻣﻮﺧﺘﻪ ﮐﺎرﺷﻨﺎﺳﯽارﺷﺪ ﻋﻠﻮم ﮔﯿﺎﻫﯽ، داﻧﺸﮑﺪه ﻋﻠﻮم، داﻧﺸﮕﺎه ﭘﯿﺎم ﻧﻮر، ﺗﻬﺮان 3اﺳﺘﺎدﯾﺎر ﭘﮋوﻫﺶ، ﻣﺮﮐﺰ ﺗﺤﻘﯿﻘﺎت ﮔﯿﺎﻫﺎن داروﯾﯽ، ﭘﮋوﻫﺸﮑﺪه ﮔﯿﺎﻫﺎن داروﯾﯽ ﺟﻬﺎد داﻧﺸﮕﺎﻫﯽ، ﮐﺮج ﺗﺎرﯾﺦ درﯾﺎﻓﺖ: 12/10/1394؛ ﺗﺎرﯾﺦ ﭘﺬﯾﺮش: 1395/12/19 ﭼﮑﯿﺪه1 دﻫﺴﺘﺎن ز ارمرود در ﺑﺨﺶ ﻫﺰارﺟﺮﯾﺐ ﺷﻬﺮﺳﺘﺎن ﻧﮑﺎ (اﺳﺘﺎن ﻣﺎزﻧﺪران)، ﻗﺮار دارد. اﯾﻦ دﻫﺴﺘﺎن ﻣﻨﻄﻘـﻪ اي ﮐﻮﻫﺴﺘﺎﻧﯽ ﺑﺎ ﻣﺴﺎﺣﺘﯽ ﺣﺪود 609 ﮐﯿﻠﻮﻣﺘﺮ ﻣﺮﺑﻊ، در داﻣﻨﻪ ارﺗﻔﺎﻋﯽ 1700 ﺗﺎ 2100 ﻣﺘﺮ از ﺳﻄﺢ درﯾﺎ ﻗـﺮار ﮔﺮﻓﺘـﻪ اﺳﺖ. ﺑﺮاي ﻣﻄﺎﻟﻌﻪ ﻓﻠﻮر ﻣﻨﻄﻘﻪ، ﻧﻤﻮﻧﻪﻫﺎي ﮔﯿﺎﻫﯽ ﻃﯽ ﺳﺎلﻫﺎي 1391 و1392، ﺟﻤﻊآوري و ﺑﺎ اﺳـﺘﻔﺎده از ﻣﻨـﺎﺑﻊ ﻣﻌﺘﺒﺮ ﻓﻠﻮرﺳﺘﯿﮏ ﺷﻨﺎﺳﺎﯾﯽ ﺷﺪﻧﺪ. در ﻣﺠﻤﻮع 172 ﮔﻮﻧﻪ، ﻣﺘﻌﻠﻖ ﺑﻪ 146 ﺟﻨﺲ از 69 ﺗﯿﺮه ﺷﻨﺎﺳﺎﯾﯽ ﺷـﺪ. ﺗ ﯿـ ﺮه Fabaceae ﺑﺎ داﺷﺘﻦ 12 ﺟﻨﺲ و 16 ﮔﻮﻧﻪ از ﺑﺰرﮔﺘﺮﯾﻦ ﺗﯿ ﺮهﻫﺎي ﻣﻨﻄﻘﻪ ﻣﺤﺴﻮب ﻣ ﯽﺷﻮد. از ﻧﻈﺮ ﺷﮑﻞ زﯾﺴـﺘ ﯽ، 37 درﺻﺪ از ﮔﻮﻧﻪﻫﺎ ﻫﻤ ﯽﮐﺮﯾﭙﺘﻮﻓﯿﺖ، 26 درﺻﺪ ﻓﺎﻧﺮوﻓﯿﺖ، 19 درﺻﺪ ﮐﺮﯾﭙﺘﻮﻓﯿﺖ، 17 درﺻﺪ ﺗﺮوﻓﯿﺖ و 1 درﺻﺪ ﮐﺎﻣ ﻪﻓﯿﺖ ﻫﺴﺘﻨﺪ. ﻓﺮاواﻧﯽ ﮔﻮﻧﻪﻫﺎي ﻓﺎﻧﺮوﻓﯿﺖ ﺑﺎ وﺿﻌﯿﺖ ﻃﺒﯿﻌﯽ ﭘﻮﺷﺶ ﮔﯿﺎﻫﯽ ﻣﻨﻄﻘﻪ ﯾﻌﻨﯽ ﻏﻠﺒﻪ رﯾﺨﺘﺎر ﺟﻨﮕﻠﯽ ﻫﻤﺨﻮاﻧﯽ دارد. ﺑﺮ اﺳﺎس ﺗﻮزﯾﻊ ﺟﻐﺮاﻓﯿﺎي ﮔﯿﺎﻫﯽ، 36 درﺻﺪ از ﮔﻮﻧﻪﻫﺎ ﻋﻨﺼﺮ روﯾﺸﯽ ﻧﺎﺣﯿﻪ ارو - ﺳـ ﯿﺒﺮي، Downloaded from pec.gonbad.ac.ir at 6:30 +0330 on Friday October 1st 2021 23 درﺻﺪ از ﮔﻮ ﻧﻪﻫﺎ ﭼﻨﺪ ﻧﺎﺣﯿ ﻪاي، 16 درﺻﺪ ﺑﻪ ﻃﻮر ﻣﺸﺘﺮك ﻋﻨﺼﺮ روﯾﺸﯽ ﻧﺎﺣﯿﻪ ارو - ﺳﯿﺒﺮي و اﯾﺮان- ﺗﻮراﻧﯽ، 14 درﺻﺪ اﯾﺮان – ﺗﻮراﻧﯽ و 2 درﺻﺪ ﺟﻬﺎن وﻃﻨﯽ ﻣ ﯽﺑﺎﺷﻨﺪ. -

Characterisation of a Novel Fruit Type Found in Ehretia (Ehretiaceae, Boraginales)
BLUMEA 49: 145–153 Published on 3 May 2004 doi: 10.3767/000651904X486250 CHARACTERISATION OF A NOVEL FRUIT TYPE FOUND IN EHRETIA (EHRETIACEAE, BORAGINALES) MARC GOTTSCHLING1, 2 & HARTMUT H. HILGER1 SUMMARY Ehretia (Ehretiaceae, Boraginales) has been divided into two major clades, characterised by fruits with four endocarpids (Ehretia I, including species of Ehretia formerly belonging to Rotula) and by fruits with two endocarpids (Ehretia II, plus E. microphylla (= Carmona retusa) with an undivided endocarp), respectively. Both molecular (ITS1) and morphological data support the recognition of an additional clade, Ehretia III (E. longiflora species group). Its representatives are characterised by four endocarpids (as in Ehretia I), but differ in the presence of distinct lamellae on the abaxial surface of each endocarpid (as in Bourreria, also belonging to Ehretiaceae). However, molecular data suggest a close relationship with Ehretia II. At least three species belong to Ehretia III: Chinese E. longiflora, eastern Indian E. wallichiana, and Indonesian E. javanica. Key words: Ehretia longiflora, anatomy, fruit, ITS1, molecular systematics, phylogeny, phylo- geography. INTRODUCTION Ehretiaceae (Boraginales) are pantropical in distribution (with centres of diversity in Central America, Africa, and East Asia) and comprise about 150 species. The plants are usually subshrubs, shrubs, or trees, and otherwise have the typical asterid characters such as tetracyclic, pentamerous flowers with five antesepalous stamens and bicarpel- late gynoecia. Fruit morphology provides a systematically important set of characters in Ehretiaceae (Pitot, 1939a, b; Miller, 1989; Verdcourt, 1991; Gottschling & Hilger, 2001). Most of the species of Ehretiaceae have drupes (otherwise dry nutlets), with either undivided, two-, or four-parted endocarps. The individual parts of the two- and four-parted endocarps are termed endocarpids and enclose two seeds or one seed each, respectively.