Facilitator's Guide of Urban Communities Children And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

BHABHA ATOMIC RESEARCH CENTRE Monthly Report On
BHABHA ATOMIC RESEARCH CENTRE Monthly Report on Implementation of RTI for the period 01.10.2011 to 31.12.2011 Name of the Unit: BARC, Trombay, Mumbai Applications received / Processed during the period: Oct to Dec. 2011. Sr. Request Party Subject Date of ** Mode of Action taken Remarks No. No. (Brief description of query) receipt Amount Payment Recd. (`) 1 09-889 Dr. Vishvas M. Kulkarni, Plant Cell Inf.on applications submitted to the 02.9.11 - - Information Culture Technology Section, Institutional Bio-Safety Committee provided on NABTD, BARC, Mumbai - 85 of BARC. 12.10.2011. 2 09-897 Shri V.R.G. Prakash, 1/75, Raja Radiation effect on installation of 14.9.11 - - Information Industrial Estate P.K. Road, mobile ground station & antenna on provided on Mulund, Mumbai-400080. terrace. 11.10.2011. 3 09-899 Shri Ashok Kumar, SO/D, CHSS facility for dependents 15.9.11 - - Information HUL&ESS, RLG Bldg.,BARC, provided on Trombay, Mumbai-400085. 10.10.2011. 4 09-900 Shri Sunil K. Sahu, SO/C, TPD, 3- Criteria for availing CHSS. 15..9.11 - - Information 10-H, Mod.Labs, BARC, Trombay, provided on Mumbai-400085. 14.10.2011. 5 09-902 Shri N.M. Gandhi, RB&HSD/BMG, Action taken on representation to 15..9.11 - - Information BARC, Trombay, Mumbai- Director, BARC. provided on 400085. 07.10.2011. 6 09-904 Shri Suresh G.Gholap, Bank account details of BARC 19..9.11 -* - Information *Fee in the form of Court Spl.Recovery employee. provided on Fee Stamp, not Officer,Yashomandir Co- 17.10.2011. -

Maharashtra State Boatd of Sec & H.Sec Education Pune
MAHARASHTRA STATE BOATD OF SEC & H.SEC EDUCATION PUNE - 4 Page : 1 schoolwise performance of Fresh Regular candidates MARCH-2020 Division : MUMBAI Candidates passed School No. Name of the School Candidates Candidates Total Pass Registerd Appeared Pass UDISE No. Distin- Grade Grade Pass Percent ction I II Grade 16.01.001 SAKHARAM SHETH VIDYALAYA, KALYAN,THANE 185 185 22 57 52 29 160 86.48 27210508002 16.01.002 VIDYANIKETAN,PAL PYUJO MANPADA, DOMBIVLI-E, THANE 226 226 198 28 0 0 226 100.00 27210507603 16.01.003 ST.TERESA CONVENT 175 175 132 41 2 0 175 100.00 27210507403 H.SCHOOL,KOLEGAON,DOMBIVLI,THANE 16.01.004 VIVIDLAXI VIDYA, GOLAVALI, 46 46 2 7 13 11 33 71.73 27210508504 DOMBIVLI-E,KALYAN,THANE 16.01.005 SHANKESHWAR MADHYAMIK VID.DOMBIVALI,KALYAN, THANE 33 33 11 11 11 0 33 100.00 27210507115 16.01.006 RAYATE VIBHAG HIGH SCHOOL, RAYATE, KALYAN, THANE 151 151 37 60 36 10 143 94.70 27210501802 16.01.007 SHRI SAI KRUPA LATE.M.S.PISAL VID.JAMBHUL,KULGAON 30 30 12 9 2 6 29 96.66 27210504702 16.01.008 MARALESHWAR VIDYALAYA, MHARAL, KALYAN, DIST.THANE 152 152 56 48 39 4 147 96.71 27210506307 16.01.009 JAGRUTI VIDYALAYA, DAHAGOAN VAVHOLI,KALYAN,THANE 68 68 20 26 20 1 67 98.52 27210500502 16.01.010 MADHYAMIK VIDYALAYA, KUNDE MAMNOLI, KALYAN, THANE 53 53 14 29 9 1 53 100.00 27210505802 16.01.011 SMT.G.L.BELKADE MADHYA.VIDYALAYA,KHADAVALI,THANE 37 36 2 9 13 5 29 80.55 27210503705 16.01.012 GANGA GORJESHWER VIDYA MANDIR, FALEGAON, KALYAN 45 45 12 14 16 3 45 100.00 27210503403 16.01.013 KAKADPADA VIBHAG VIDYALAYA, VEHALE, KALYAN, THANE 50 50 17 13 -

Reg. No Name in Full Residential Address Gender Contact No. Email Id Remarks 9421864344 022 25401313 / 9869262391 Bhaveshwarikar
Reg. No Name in Full Residential Address Gender Contact No. Email id Remarks 10001 SALPHALE VITTHAL AT POST UMARI (MOTHI) TAL.DIST- Male DEFAULTER SHANKARRAO AKOLA NAME REMOVED 444302 AKOLA MAHARASHTRA 10002 JAGGI RAMANJIT KAUR J.S.JAGGI, GOVIND NAGAR, Male DEFAULTER JASWANT SINGH RAJAPETH, NAME REMOVED AMRAVATI MAHARASHTRA 10003 BAVISKAR DILIP VITHALRAO PLOT NO.2-B, SHIVNAGAR, Male DEFAULTER NR.SHARDA CHOWK, BVS STOP, NAME REMOVED SANGAM TALKIES, NAGPUR MAHARASHTRA 10004 SOMANI VINODKUMAR MAIN ROAD, MANWATH Male 9421864344 RENEWAL UP TO 2018 GOPIKISHAN 431505 PARBHANI Maharashtra 10005 KARMALKAR BHAVESHVARI 11, BHARAT SADAN, 2 ND FLOOR, Female 022 25401313 / bhaveshwarikarmalka@gma NOT RENEW RAVINDRA S.V.ROAD, NAUPADA, THANE 9869262391 il.com (WEST) 400602 THANE Maharashtra 10006 NIRMALKAR DEVENDRA AT- MAREGAON, PO / TA- Male 9423652964 RENEWAL UP TO 2018 VIRUPAKSH MAREGAON, 445303 YAVATMAL Maharashtra 10007 PATIL PREMCHANDRA PATIPURA, WARD NO.18, Male DEFAULTER BHALCHANDRA NAME REMOVED 445001 YAVATMAL MAHARASHTRA 10008 KHAN ALIMKHAN SUJATKHAN AT-PO- LADKHED TA- DARWHA Male 9763175228 NOT RENEW 445208 YAVATMAL Maharashtra 10009 DHANGAWHAL PLINTH HOUSE, 4/A, DHARTI Male 9422288171 RENEWAL UP TO 05/06/2018 SUBHASHKUMAR KHANDU COLONY, NR.G.T.P.STOP, DEOPUR AGRA RD. 424005 DHULE Maharashtra 10010 PATIL SURENDRANATH A/P - PALE KHO. TAL - KALWAN Male 02592 248013 / NOT RENEW DHARMARAJ 9423481207 NASIK Maharashtra 10011 DHANGE PARVEZ ABBAS GREEN ACE RESIDENCY, FLT NO Male 9890207717 RENEWAL UP TO 05/06/2018 402, PLOT NO 73/3, 74/3 SEC- 27, SEAWOODS, -

Annual Report : 2016 - 2017
ANNUAL REPORT : 2016 - 2017 Rotary Club of Bombay Midtown facilitated a educational visit to NASEOH for 28 students from Germany under Youth Exchange Programme. Field Placement of students : Name of the Institute Department Number of students Tata Institute of Social Sciences Social Work 2 Tata Institute of Social Sciences Centre for Life Long learning 2 SNDT University Social Work 2 Tilak Maharashtra Vidyapeeth Social Work 6 Swami Vivekanand College, Chembur N.S.S 65 ST. Xaviers' College , Mumbai Social Involvement Program 5 Don Bosco College of Management MBA 4 S.I.E.S College of Management MBA 6 APPRECIATION AND AWARDS NASEOH, during Diwali celebration recognizes Best Child and Best Trainee from each unit whose over all progress has been outstanding. This year the following students received the Best Student appreciations of the year. Name Unit 1. Mst. Aditya Pandya - Falguni Learning Centre (special group) 2. Mst. Vinayak Sangishetty - Falguni Learning Centre (Functional group) 3. Mr. Rohit Dharne - Tailoring 4. Mr. Parikshit Karve - Computer 5 Mr. Akshay Bhor - Bakery & Confectionery 6. Ms. Madhavi Asware - Assembly 7. Mr. Vishal Hande - Ceramic 8. Mr. Mohammed Shafique Shaikh - Welding & Fabrication 9. Mr. Pandurang Pai - Garden 10. Mr. Mohammed Zaid Kasam - Aids & Appliances Felicitation Program As of every year, this year also Rotary Club of Bombay Mid Town felicitated following two computer trainees, who stood 1st in their respective batches during 2015-16, with Cash Awards. 1. Ms. Sneha Dhuri - July'2015 batch 2. Ms. Mahisha Agvane - January'2016 batch AWARENESS & ADVOCACY Open House NASEOH organized various talks for creating awareness among trainees and parents on varied topics during the year as detailed below : 1) Importance of Independence day 2) Different types of BMC and Government schemes for disabled 3) Awareness about Hepatitis B 4) Traffic rules 5) Personal Hygiene 6) Ill-effect of tobacco chewing Distribution of Clothes With initiative and donation from Mr. -

Bus-Shelter-Advertising.Pdf
1 ONE STOP MARKETING 2 What Are You Looking For? AIRLINE/AIRPORT CINEMA DIGITAL NEWSPAPER RADIO TELEVISION MAGAZINE SERVICES OUTDOOR NON TRADITIONAL 3 Bus Shelter @ INR 35,000/- Per Month Bus Shelter @ INR 35,000/- Per Month Powai, Mumbai Suresh Nagar, Mumbai Near L&T, Powai Garden, Powai Military Road Juhu-Versova Link Road ,Bharat Nagar/Petrol Pump Bus Shelter @ INR 35,000/- Per Month Bus Shelter @ INR 35,000/- Per Month Juhu, Mumbai VN Purav Marg, Mumbai Juhu S.Parulekar Marg, Traffic Towrds Juhu Bus Station Marathi Vidnyan Parishad, V. N. Purav Road, Chunabhatti Bus Shelter @ INR 35,000/- Per Month Bus Shelter @ INR 35,000/- Per Month Andheri East, Mumbai Andheri East, Mumbai International Airport Road, Sahar Road, Ambassador Outside Techno Mall, Jogeshwari Link Road, Behram Hotel Bagh 4 Bus Shelter @ INR 35,000/- Per Month Bus Shelter @ INR 35,000/- Per Month Lohar Chawl, Mumbai Lad Wadi, Mumbai Kalbadevi Road ,Princess Street 2 Kalbadevi Road ,Princess Street 1 Bus Shelter @ INR 35,000/- Per Month Bus Shelter @ INR 35,000/- Per Month Savarkar Nagar, Mumbai Mahim Nature park, Mumbai Near L&T, Powai Garden, Powai Military Road Dharavi Depot, Dumping Road, Dharavi Bus Shelter @ INR 35,000/- Per Month Bus Shelter @ INR 35,000/- Per Month Antop Hill, Mumbai Bharat Nagar, Mumbai Antop Hill, Shaikh Misri Road, Antop Hill Juhu-Versova Link Road ,Bharat Nagar/Petrol Pump 5 Bus Shelter @ INR 35,000/- Per Month Bus Shelter @ INR 35,000/- Per Month Wadala, Mumbai Kurla East, Mumbai Wadala Station, Kidwai Marg, Wadala S.T. Depot (Kurla East), S.T. -
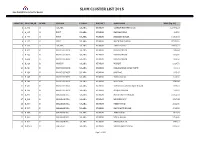
List of Slum Cluster 2015
SLUM CLUSTER LIST 2015 Slum Rehabilitation Authority, Mumbai OBJECTID CLUSTER_ID WARD VILLAGE TALUKA DISTRICT SLUM NAME AREA (Sq. M.) 1 A_001 A COLABA COLABA MUMBAI GANESH MURTHI NAGAR 120771.23 2 A_005 A FORT COLABA MUMBAI BANGALIPURA 318.50 3 A_006 A FORT COLABA MUMBAI NARIMAN NAGAR 14315.98 4 A_007 A FORT COLABA MUMBAI MACHIMAR NAGAR 37181.09 5 A_009 A COLABA COLABA MUMBAI GEETA NAGAR 26501.21 6 B_021 B PRINCESS DOCK COLABA MUMBAI DANA BANDAR 939.53 7 B_022 B PRINCESS DOCK COLABA MUMBAI DANA BANDAR 1292.90 8 B_023 B PRINCESS DOCK COLABA MUMBAI DANA BANDAR 318.67 9 B_029 B MANDVI COLABA MUMBAI MANDVI 1324.71 10 B_034 B PRINCESS DOCK COLABA MUMBAI NALABANDAR JOPAD PATTI 600.14 11 B_039 B PRINCESS DOCK COLABA MUMBAI JHOPDAS 908.47 12 B_045 B PRINCESS DOCK COLABA MUMBAI INDRA NAGAR 1026.09 13 B_046 B PRINCESS DOCK COLABA MUMBAI MAZGAON 1541.46 14 B_047 B PRINCESS DOCK COLABA MUMBAI SUBHASHCHANDRA BOSE NAGAR 848.16 15 B_049 B PRINCESS DOCK COLABA MUMBAI MASJID BANDAR 277.27 16 D_001 D MALABAR HILL COLABA MUMBAI MATA PARVATI NAGAR 21352.02 17 D_003 D MALABAR HILL COLABA MUMBAI BRANHDHARY 1597.88 18 D_006 D MALABAR HILL COLABA MUMBAI PREM NAGAR 3211.09 19 D_007 D MALABAR HILL COLABA MUMBAI NAVSHANTI NAGAR 4013.82 20 D_008 D MALABAR HILL COLABA MUMBAI ASHA NAGAR 1899.04 21 D_009 D MALABAR HILL COLABA MUMBAI SIMLA NAGAR 9706.69 22 D_010 D MALABAR HILL COLABA MUMBAI SHIVAJI NAGAR 1841.12 23 D_015A D GIRGAUM COLABA MUMBAI SIDHDHARTH NAGAR 2189.50 Page 1 of 101 SLUM CLUSTER LIST 2015 Slum Rehabilitation Authority, Mumbai OBJECTID CLUSTER_ID WARD VILLAGE TALUKA DISTRICT SLUM NAME AREA (Sq. -

Total List of MCGM and Private Facilities.Xlsx
MUNICIPAL CORPORATION OF GREATER MUMBAI MUNICIPAL DISPENSARIES SR SR WARD NAME OF THE MUNICIPAL DISPENSARY ADDRESS NO NO 1 1 COLABA MUNICIPALMUNICIPAL DISPENSARY 1ST FLOOR, COLOBA MARKET, LALA NIGAM ROAD, COLABA MUMBAI 400 005 SABOO SIDIQUE RD. MUNICIPAL DISPENSARY ( 2 2 SABU SIDDIQ ROAD, MUMBAI (UPGRADED) PALTAN RD.) 3 3 MARUTI LANE MUNICIPAL DISPENSARY MARUTI LANE,MUMBAI A 4 4 S B S ROAD. MUNICIPAL DISPENSARY 308, SHAHID BHAGATSINGH MARG, FORT, MUMBAI - 1. 5 5 HEAD OFFICE MUNICIPAL DISPENSARY HEAD OFFICE BUILDING, 2ND FLOOR, ANNEX BUILDING, MUMBAI - 1, 6 6 HEAD OFFICE AYURVEDIC MUNICIPAL DISPENSARY HEAD OFFICE BUILDING, 2ND FLOOR, ANNEX BUILDING, MUMBAI - 1, 7 1 SVP RD. MUNICIPAL DISPENSARY 259, SARDAR VALLABBHAI PATEL MARG, QUARTERS, A BLOCK, MAUJI RATHOD RD, NOOR BAUG, DONGRI, MUMBAI 400 8 2 WALPAKHADI MUNICIPAL DISPENSARY 009 9B 3 JAIL RD. UNANI MUNICIPAL DISPENSARY 259, SARDAR VALLABBHAI PATEL MARG, 10 4 KOLSA MOHALLA MUNICIPAL DISPENSARY 20, KOLSA STREET, KOLSA MOHALLA UNANI , PAYDHUNI 11 5 JAIL RD MUNICIPAL DISPENSARY 20, KOLSA STREET, KOLSA MOHALLA UNANI , PAYDHUNI CHANDANWADI SCHOOL, GR.FLOOR,CHANDANWADI,76-SHRIKANT PALEKAR 12 1 CHANDAN WADI MUNICIPAL DISPENSARY MARG,MARINELINES,MUM-002 13 2 THAKURDWAR MUNICIPAL DISPENSARY THAKURDWAR NAKA,MARINELINES,MUM-002 C PANJRAPOLE HEALTH POST, RAMA GALLI,2ND CROSS LANE,DUNCAN ROAD 14 3 PANJRAPOLE MUNICIPAL DISPENSARY MUMBAI - 400004 15 4 DUNCAN RD. MUNICIPAL DISPENSARY DUNCAN ROAD, 2ND CROSS GULLY 16 5 GHOGARI MOHALLA MUNICIPAL DISPENSARY HAJI HASAN AHMED BAZAR MARG, GOGRI MOHOLLA 17 1 NANA CHOWK MUNICIPAL DISPENSARY NANA CHOWK, FIRE BRIGADE COMPOUND, BYCULLA 18 2 R. S. NIMKAR MUNICIPAL DISPENSARY R.S NIMKAR MARG, FORAS ROAD, 19 3 R. -

352 Bus Time Schedule & Line Route
352 bus time schedule & line map 352 Trombay - Rani Laxmibai Chowk (Sion) View In Website Mode The 352 bus line (Trombay - Rani Laxmibai Chowk (Sion)) has 2 routes. For regular weekdays, their operation hours are: (1) Rani Laxmibai Chowk (Sion): 12:00 AM - 11:43 PM (2) Trombay: 12:04 AM - 11:48 PM Use the Moovit App to ƒnd the closest 352 bus station near you and ƒnd out when is the next 352 bus arriving. Direction: Rani Laxmibai Chowk (Sion) 352 bus Time Schedule 27 stops Rani Laxmibai Chowk (Sion) Route Timetable: VIEW LINE SCHEDULE Sunday 12:00 AM - 11:43 PM Monday 12:00 AM - 11:43 PM Trombay Tuesday 12:00 AM - 11:43 PM Dhobi Ghat (Trombay) Wednesday 12:00 AM - 11:43 PM Cheeta Camp Thursday 12:00 AM - 11:43 PM Narmadeshwar Mandir Friday 12:00 AM - 11:43 PM Mandala Saturday 12:00 AM - 11:43 PM B.A.R.C School No.6 Mankhurd Station Road (S) 352 bus Info Childrens Home Direction: Rani Laxmibai Chowk (Sion) Stops: 27 Trip Duration: 27 min Anushakti Nagar Line Summary: Trombay, Dhobi Ghat (Trombay), V.N. Purav Marg, Mumbai Cheeta Camp, Narmadeshwar Mandir, Mandala, B.A.R.C School No.6, Mankhurd Station Road (S), Raj Kapoor Chowk / Bhabha Hospital Childrens Home, Anushakti Nagar, Raj Kapoor Chowk / Bhabha Hospital, Telecom Factory, Telecom Factory Punjabwadi, Deonar Depot, R.K.Studio, Maitri Park, Deonar Govandi Road, Mumbai R.B.I Colony (Chembur), Acharya Garden/ Diamond Garden, Acharya Garden / Diamond Garden, Sandu Punjabwadi Wadi, Chembur Naka / Swami Vivekanand Chowk, Kumbhar Wada, Umarshi Bappa Chowk, Deonar Depot Priyadarshani Chuna -

@MEMORANDUM to the GOVERNMENT of £INDIA Arising from an Amnesty International Visit to India 5-15 January 1994
@MEMORANDUM TO THE GOVERNMENT OF £INDIA arising from an Amnesty International visit to India 5-15 January 1994 INTRODUCTION In January 1994, Amnesty International carried out its first research visit to an Indian state - Maharashtra - for 14 years. The visit, by Professor Rod Morgan, Dean of the Faculty of Law, Bristol University, and Yvonne Terlingen, of the Asia Department of Amnesty International's International Secretariat, was to Bombay and took place from 8 -15 January 1994. The visit was an important step which substantially furthered the dialogue initiated in November 1992 when an Amnesty International delegation discussed its human rights concerns, for the first time in many years, directly with the Indian Government in Delhi. Having reaffirmed its commitment to protect human rights and repeatedly and publicly condemned custodial violence, which has remained one of Amnesty International's core human rights concerns in India, the government eventually permitted Amnesty International to see the situation on the ground in one Indian state and to talk freely to officials and others. Before visiting Bombay, the Amnesty International delegation met the Minister for Home Affairs and the Minister of State for Home Affairs, as well as the Home Secretary and other officials in Delhi, from 5 - 8 January 1994 to discuss the organization's continuing human rights concerns. These concerns included: the need to strengthen safeguards for people in custody; the apparent rise, despite the government's official condemnation of such practices, of the numbers of people dying in police custody in Delhi, apparently as a result of torture or ill-treatment; and the fate or whereabouts of hundreds of people reported to have "disappeared" in recent years in the states of Jammu and Kashmir and Punjab (described in an Amnesty International report released in December 1993)1. -

1 List of Fino Payments Bank Branches & CSP Points Closed With
List of Fino Payments Bank Branches & CSP Points Closed with Destination Branches Source Destination Sr Branch Branch No. Type Code Source Branch Name State District Code Destination Branch Name State District Madhya 1 CSP 144651 Ashoknagar - Mungaoli Madhya Pradesh Ashoknagar 144624 Asoknagar Pradesh Ashoknagar Madhya 2 CSP 144630 Bistan Madhya Pradesh Khargone 144641 Khargone Pradesh Khargone Madhya 3 CSP 144645 Maheshwar Madhya Pradesh Khargone 144641 Khargone Pradesh Khargone 4 CSP 144718 chandur Bazar Maharashtra Amravati 144730 Amrawati Maharashtra Amravati 5 CSP 144704 Daryapur Maharashtra Akola 144730 Amrawati Maharashtra Amravati 6 CSP 144720 Achalpur Maharashtra Amravati 144730 Amrawati Maharashtra Amravati 7 CSP 144719 Murtijapur Maharashtra Akola 144730 Amrawati Maharashtra Amravati 8 CSP 144726 Walgaon Maharashtra Amravati 144730 Amrawati Maharashtra Amravati 9 CSP 144708 Chandur Railway Maharashtra Amravati 144703 Warud Maharashtra Amravati 10 CSP 144724 Tivsa Maharashtra Amravati 144703 Warud Maharashtra Amravati 11 CSP 144728 Kalmeshwar Maharashtra Nagpur 144713 Ramtek Maharashtra Nagpur 12 CSP 144725 Morshi Maharashtra Amravati 144703 Warud Maharashtra Amravati 13 CSP 144717 Saoner Maharashtra Nagpur 144713 Ramtek Maharashtra Nagpur 14 CSP 144714 Ner Maharashtra Yevatmal 144721 Yavatmal Maharashtra Yevatmal 15 CSP 144706 Hinganghat Maharashtra Wardha 144705 Wardha Maharashtra Wardha 16 CSP 144711 Ralegaon Maharashtra Yevatmal 144721 Yavatmal Maharashtra Yevatmal 17 CSP 144701 Arni Maharashtra Yevatmal 144721 Yavatmal -

1. Councillors & Officers List
Yeejleer³e je<ì^ieerle HetCe& peveieCeceve-DeefOevee³ekeÀ pe³e ns Yeejle-Yeei³eefJeOeelee ~ Hebpeeye, efmebOeg, iegpejele, cejeþe, NATIONAL ANTHEM OF INDIA êeefJe[, GlkeÀue, yebie, efJebO³e, efncee®eue, ³ecegvee, iebiee, Full Version G®íue peueeqOelejbie leJe MegYe veeces peeies, leJe MegYe DeeeqMe<e ceeies, Jana-gana-mana-adhinayaka jaya he ieens leJe pe³eieeLee, Bharat-bhagya-vidhata peveieCe cebieueoe³ekeÀ pe³e ns, Punjab-Sindhu-Gujarata-Maratha Yeejle-Yeei³eefJeOeelee ~ Dravida-Utkala-Banga pe³e ns, pe³e ns, pe³e ns, pe³e pe³e pe³e, pe³e ns ~~ Vindhya-Himachala-Yamuna-Ganga mebef#eHle Uchchala-jaladhi-taranga peveieCeceve-DeefOevee³ekeÀ pe³e ns Tava Shubha name jage, tava subha asisa mage Yeejle-Yeei³eefJeOeelee ~ Gahe tava jaya-gatha pe³e ns, pe³e ns, pe³e ns, Jana-gana-mangala-dayaka jaya he pe³e pe³e pe³e, pe³e ns ~~ Bharat-bhagya-vidhata Jaya he, jaya he, jaya he, Jaya jaya jaya jaya he. Short version Jana-gana-mana-adhinayaka jaya he Bharat-bhagya-vidhata Jaya he, Jaya he, jaya he jaya jaya jaya, jaya he, PERSONAL MEMORANDUM Name ............................................................................................................................................................................ Office Address .................................................................................................................... ................................................................................................................................................ .................................................... .............................................................................................. -
Master of Philosphy 2015-16 Anil Kumar
MASTER OF PHILOSPHY 2015-16 ANIL KUMAR Contact No: 8879728350 Email: [email protected] Skype: Career Objective I am looking forward to pursue a career in the field of research. I am seeking to deliver my research, analytical, as well as presentation skills that will benefit in volume, growth, brand, and profits. Academic Qualifications Course Board/ University Subjects Year Percentage/ CGPA International Institute for Population M.Phil Population Studies 2016 Result awaited Sciences, Mumbai Maharashtra. International Institute for Population M.A Population Studies 2013 61.16 Sciences, Mumbai Maharashtra. Tata Institute of Social Sciences, Social work and B.A 2011 63.71 Tuljapur Maharashtra. Rural development HSC DAV Jawahar Vidya Mandir, Shyamli Arts 2006 62 Ranchi SSC DAV Jawahar Vidya Mandir, Shyamli Arts 2004 56.5 Ranchi Professional Experience/Internships Organisation: TISS, Place of Work: Mumbai Designation: Program Manager June 2013-July 2015 Job responsibilities To conduct research based studies (Baseline survey, Impact assessment and Evaluation studies) Partnership and client management (MoU and Legal) Proposal Evaluation and NGO Empanelment. Project Implementation Research Experience Topic of dissertation (M.Phil): Gender based power relation in Indian Households-A Study to analyze the autonomy of women through socio-cultural factors. Topic of dissertation (M.A/M.Sc.): Utilization of Maternal Health care services in EAG states of India. Topic of Dissertation (BA in Social Work) Social work and childhood Poverty, Social work Seminar. Topic of Dissertation (B.A in Social Work) Rural Development and Displacement, Rural Development Seminar. Academic Achievements Medals Awards: UGC NET, In Population Sciences June 2012. Fellowships Scholarships If any Papers Published Conferences/Seminars/Workshops Quality of health Care in India in the Existing System: Revisiting the Judith Bruce Framework, Evidence from NFHS-3.