Cardiac Arrhythmias
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Safety and Efficacy of Ibutilide in Cardioversion of Atrial Flutter And
J Am Board Fam Med: first published as 10.3122/jabfm.2011.01.080096 on 5 January 2011. Downloaded from CLINICAL REVIEW Safety and Efficacy of Ibutilide in Cardioversion of Atrial Flutter and Fibrillation Madhuri Nair, MD, Lekha K. George, MD, and Santhosh K. G. Koshy, MD This article reviews the safety and efficacy of ibutilide for use in patients with atrial fibrillation and flut- ter. Ibutilide, a class III antiarrhythmic agent, is primarily used for conversion of atrial flutter and fi- brillation and is a good alternative to electrical cardioversion. Ibutilide has a conversion rate of up to 75% to 80% in recent-onset atrial fibrillation and flutter; the conversion rate is higher for atrial flutter than for atrial fibrillation. It is also safe in the conversion of chronic atrial fibrillation/flutter among patients receiving oral amiodarone therapy. Ibutilide pretreatment facilitates transthoracic defibrilla- tion and decreases the energy requirement of electrical cardioversion by both monophasic and biphasic shocks. Pretreatment with ibutilide before electrical defibrillation has a conversion rate of 100% com- pared with 72% with no pretreatment. Ibutilide is also safe and efficient in the treatment of atrial fibril- lation in patients who have had cardiac surgery, and in accessory pathway–mediated atrial fibrillation where the conversion rate of ibutilide is as high as 95%. There is up to a 4% risk of torsade de pointes and a 4.9% risk of monomorphic ventricular tachycardia. Hence, close monitoring in an intensive care unit setting is warranted during and at least for 4 hours after drug infusion. The anticoagulation strat- egy is the same as for any other mode of cardioversion.(J Am Board Fam Med 2011;24:86–92.) Keywords: Antiarrhythmics, Arrhythmia, Atrial Fibrillation, Cardiovascular Disorders, Cardioversion, Drug Ther- copyright. -

Emergency Medical Services Program Policies – Procedures – Protocols
Emergency Medical Services Program Policies – Procedures – Protocols Protocols Table of Contents GENERAL PROVISIONS ................................................................................................ 3 DESTINATION DECISION SUMMARY-METRO BAKERSFIELD AREA ........................ 5 DETERMINATION OF DEATH ..................................................................................... 12 101 AIRWAY OBSTRUCTION ...................................................................................... 16 102 ALTERED LEVEL OF CONSCIOUSNESS ............................................................ 18 103 ALLERGIC REACTION/ANAPHYLAXIS ................................................................ 20 104 ASYSTOLE/ PULSELESS ELECTRICAL ACTIVITY ............................................. 22 105 BITES STINGS ENVENOMATION ......................................................................... 24 106 BRADYCARDIA ..................................................................................................... 26 107 BRIEF RESOLVED UNEXPLAINED EVENT ......................................................... 29 108 BURNS ................................................................................................................... 32 109 CHEMPACK ........................................................................................................... 35 110 CHEST PAIN OR ACUTE CORONARY SYNDROME ........................................... 37 111 CHEST TRAUMA .................................................................................................. -

Supplementary Materials
Supplementary Materials Table S1. The significant drug pairs in potential DDIs examined by the two databases. Micromedex Drugs.com List of drugs paired PK-PD Mechanism details 1. Amiodarone— PD Additive QT-interval prolongation Dronedarone 2. Amiodarone— PK CYP3A inhibition by Ketoconazole Ketoconazole 3. Ciprofloxacin— PD Additive QT-interval prolongation Dronedarone 4. Cyclosporine— PK CYP3A inhibition by Cyclosporine Dronedarone 5. Dronedarone— PK CYP3A inhibition by Erythromycin Erythromycin 6. Dronedarone— PD Additive QT-interval prolongation Flecainide 7. Dronedarone— PK CYP3A4 inhibition by Itraconazole Itraconazole 8. Dronedarone— PK Contraindication Major CYP3A inhibition by Ketoconazole Ketoconazole 9. Dronedarone— PD Additive QT-interval prolongation Procainamide PD 10. Dronedarone—Sotalol Additive QT-interval prolongation 11. Felodipine— PK CYP3A inhibition by Itraconazole Itraconazole 12. Felodipine— PK CYP3A inhibition by Ketoconazole Ketoconazole 13. Itraconazole— PK CYP3A inhibition by Itraconazole Nisoldipine 14. Ketoconazole— PK CYP3A inhibition by Ketoconazole Nisoldipine 15. Praziquantel— PK CYP induction by Rifampin Rifampin PD 1. Amikacin—Furosemide Additive or synergistic toxicity 2. Aminophylline— Decreased clearance of PK Ciprofloxacin Theophylline by Ciprofloxacin 3. Aminophylline— PK Decreased hepatic metabolism Mexiletine 4. Amiodarone— PD Additive effects on QT interval Ciprofloxacin 5. Amiodarone—Digoxin PK P-glycoprotein inhibition by Amiodarone 6. Amiodarone— PD, PK Major Major Additive effects on QT Erythromycin prolongation, CYP3A inhibition by Erythromycin 7. Amiodarone— PD, PK Flecainide Antiarrhythmic inhibition by Amiodarone, CYP2D inhibition by Amiodarone 8. Amiodarone— PK CYP3A inhibition by Itraconazole Itraconazole 9. Amiodarone— PD Antiarrhythmic inhibition by Procainamide Amiodarone 10. Amiodarone— PK CYP induction by Rifampin Rifampin PD Additive effects on refractory 11. Amiodarone—Sotalol potential 12. Amiodarone— PK CYP3A inhibition by Verapamil Verapamil 13. -
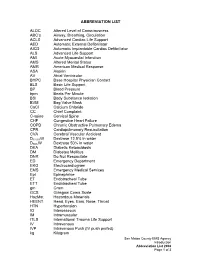
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC's Airway, Breathing, Circulation ACLS Advanced Cardiac Life Suppo
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC’s Airway, Breathing, Circulation ACLS Advanced Cardiac Life Support AED Automatic External Defibrillator AICD Automatic Implantable Cardiac Defibrillator ALS Advanced Life Support AMI Acute Myocardial Infarction AMS Altered Mental Status AMR American Medical Response ASA Aspirin AV Atrial Ventricular BHPC Base Hospital Physician Contact BLS Basic Life Support BP Blood Pressure bpm Beats Per Minute BSI Body Substance Isolation BVM Bag Valve Mask CaCl Calcium Chloride CC Chief Complaint C-spine Cervical Spine CHF Congestive Heart Failure COPD Chronic Obstructive Pulmonary Edema CPR Cardiopulmonary Resuscitation CVA Cerebral Vascular Accident D12.5%W Dextrose 12.5% in water D50%W Dextrose 50% in water DKA Diabetic Ketoacidosis DM Diabetes Mellitus DNR Do Not Resuscitate ED Emergency Department EKG Electrocardiogram EMS Emergency Medical Services Epi Epinephrine ET Endotracheal Tube ETT Endotracheal Tube gm Gram GCS Glasgow Coma Scale HazMat Hazardous Materials HEENT Head, Eyes, Ears, Nose, Throat HTN Hypertension IO Interosseous IM Intramuscular ITLS International Trauma Life Support IV Intravenous IVP Intravenous Push (IV push prefed) kg Kilogram San Mateo County EMS Agency Introduction Abbreviation List 2008 Page 1 of 3 J Joule LOC Loss of Consciousness Max Maximum mcg Microgram meds Medication mEq Milliequivalent min Minute mg Milligram MI Myocardial Infarction mL Milliliter MVC Motor Vehicle Collision NPA Nasopharyngeal Airway NPO Nothing Per Mouth NS Normal Saline NT Nasal Tube NTG Nitroglycerine NS Normal Saline O2 Oxygen OB Obstetrical OD Overdose OPA Oropharyngeal Airway OPQRST Onset, Provoked, Quality, Region and Radiation, Severity, Time OTC Over the Counter PAC Premature Atrial Contraction PALS Pediatric Advanced Life Support PEA Pulseless Electrical Activity PHTLS Prehospital Trauma Life Support PID Pelvic Inflammatory Disease PO By Mouth Pt. -

Keeping up with the Pace of Antiarrhythmic Drugs ANNMARIE PALATNIK, APN,BC, MSN Coordinator of Continuing Education • Virtua Health • Marlton, N.J
D rug File Keeping up with the pace of antiarrhythmic drugs ANNMARIE PALATNIK, APN,BC, MSN Coordinator of Continuing Education • Virtua Health • Marlton, N.J. HAVE YOU NOTICED how challenging it is to Conducting impulses keep pace with the The conduction system of the heart, shown below, begins with the heart’s natural pacemaker, the changing beat of phar- sinoatrial (SA) node. When an impulse leaves the SA node, it travels through the atria along macology? Just as you Bachmann’s bundle and the internodal pathways on its way to the atrioventricular (AV) node. After learn the latest drugs the impulse passes through the AV node, it travels to the ventricles, first down the bundle of His, and classifications, new then along the bundle branches and, finally, down the Purkinje fibers. classes are developed and new drugs added to Bachmann’s bundle classes. Even drugs that have been on the mar- ket a long time can have dosing and indica- SA node tion changes. Antiarrhythmic Internodal tracts drugs, which restore Posterior (Thorel’s) normal rhythm and Middle (Wenckebach’s) conduction to the heart, Anterior are no exception. In this AV node article, I’ll bring you up-to-date on the Bundle of His antiarrhythmics now Right bundle branch available. Left bundle branch Class assignments Most antiarrhythmic drugs used to slow a rapid heart rate are classified according to the Vaughn Williams classification system Purkinje fibers (see Classifying Anti- arrhythmics the Vaughn Williams way). These drugs fall Class I into four general groups in this classification system Sodium channel blockers stop the flow of sodium into with each group having several subgroups. -

Pharmaceuticals As Environmental Contaminants
PharmaceuticalsPharmaceuticals asas EnvironmentalEnvironmental Contaminants:Contaminants: anan OverviewOverview ofof thethe ScienceScience Christian G. Daughton, Ph.D. Chief, Environmental Chemistry Branch Environmental Sciences Division National Exposure Research Laboratory Office of Research and Development Environmental Protection Agency Las Vegas, Nevada 89119 [email protected] Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada Why and how do drugs contaminate the environment? What might it all mean? How do we prevent it? Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada This talk presents only a cursory overview of some of the many science issues surrounding the topic of pharmaceuticals as environmental contaminants Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada A Clarification We sometimes loosely (but incorrectly) refer to drugs, medicines, medications, or pharmaceuticals as being the substances that contaminant the environment. The actual environmental contaminants, however, are the active pharmaceutical ingredients – APIs. These terms are all often used interchangeably Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada Office of Research and Development Available: http://www.epa.gov/nerlesd1/chemistry/pharma/image/drawing.pdfNational -

FIRST AID QUICK SHEET- Airway and Breathing
FIRST AID QUICK SHEET Airway and Breathing After you have checked to make sure the scene is safe and put on gloves to protect yourself (Danger) and checked if the patient is responsive (Response), if you find the patient is not responding, you should think: ABC. First check for an Airway and Breathing. Instructions for the A and B steps of the DR. ABC acronym for first aid priorities are below: How to Adjust Someone’s Airway (A): 1. Gently swipe the mouth with one finger to ensure that no objects are blocking the airway. 2. Place two fingers under the casualties chin and one hand on the forehead. 3. Gently lift the chin with two fingers, removing the tongue from the back of the throat. 4. If transport is delayed, roll the casualty onto their side in the recovery position to allow fluids to drain from the mouth Note: If someone is able to speak, their airway is open. Breathing (B): 1. Always remember to look, listen, and feel when checking for breathing. 2. LOOK to see the chest rise and fall. 3. LISTEN to hear breath sounds. 4. Place one hand on the stomach and FEEL for breathing movement and FEEL beneath the nose for air movement. After you have secured an airway and checked for breathing, you may move on to check for bleeding in the C (circulation) step of DR. ABC. *Please be safe and practice first aid at your own risk. LFR International is not liable for injuries resulting from any first aid attempts. . -
Basic Trauma Overview - ABC
Basic Trauma Overview - ABC Dale Dangleben, MD, FACS 1 2 Team 3 Extended Team 4 Team Leader Decrease chaos / optimize care. – Remains calm – Maintains control and provides direction – Stays decisive – Sees the big picture (situational awareness) – Is open to other team members input – Directs resuscitation – Makes early decision to transfer the patients that exceed the local capabilities 5 Team Members − Know your roles in the trauma team − Remain calm − Be responsive to team leader −Voice suggestions or concerns 6 Responsibilities – Perform the Primary and secondary survey – Verbalize patient care – Report completed tasks 7 Responsibilities – Monitors the patient – Manual BP – Obtains IV access – Administers medications – Dresses wounds – Performs or assists in resuscitative procedures 8 Responsibilities Records data Ensures documentation accompanies patient upon transfer Assists team members as needed 9 Responsibilities – Obtains needed supplies – Coordinates communication with local and external resources – Assists team members as needed 10 Responsibilities • Place Oxygen on patient • Manage airway • Hold C spine • Manage ventilator if • Manage rapid infuser line patient intubated where indicated • Assists team members as needed 11 Organization of trauma resuscitation area – Basic adult and pediatric equipment for: • Airway management (cart) • IV access with warm fluids • Chest tube insertion • Hemorrhage control (tourniquets, pelvic binders) • Immobilization • Medications • Pediatric length/weight based tape (Broselow Tape) – Warming -

Procainamide in the Treatment of Myotonia in Myotonic Dystrophy
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.45.5.461 on 1 May 1982. Downloaded from Journal ofNeurology, Neurosurgery, and Psychiatry 1982;45:461-463 Short report A comparative study of disopyramide and procainamide in the treatment of myotonia in myotonic dystrophy MICHAEL FINLAY From the Department ofNeurology, Royal Hallamshire Hospital, Sheffield SUMMARY Ten patients with myotonic dystrophy were allocated at random to treatment with disopyramide and procainamide in a cross-over trial. Disopyramide was found to be at least as effective as procainamide in the relief of myotonia; and two patients who could not tolerate procainamide both tolerated disopyramide. Myotonic dystrophy was first described by Steinert' trophy for between 4 and 21 years were included in the women and the clinical features have been reviewed by trial. There were seven men and three aged be- Protected by copyright. Thomasen2 and others. There have been many tween 31 and 59 years. All complained of weakness of their attempts to elucidate the underlying pathophysi- hands and the majority had noticed difficulty in relaxation of grip. Eight had also experienced impairment of gait. All ology. The basic abnormality has been ascribed to exhibited bilateral ptosis, weakness and wasting of the hypersensitivity of the muscle membrane,3 increased masseters, temporalis, facial and stemomastoid muscles membrane fluidity4 and impairment of normal and wasting and weakness of the forearms and hands. The neurotropic influences exerted by motor neurones seven men had similar distal wasting and weakness of the on muscle fibres.5 6 Quinine, steroids and pro- legs but in two women the lower limbs were symptomati- cainamide have all been used for treatment of the cally normal; in the other woman, there was proximal myotonia with variable success. -

Abdominal Pain 02/02/2021
Medical Control Board Approved Protocols ABDOMINAL PAIN 02/02/2021 Follow Assessment, General Procedures Protocol EMR • Assess and support ABCs • Position of comfort • Supine if: • Trauma • Hypotension • Syncope • NPO • Monitor vital signs • Oxygen indicated for: • Unstable vitals • Severity of pain • Suspected GI bleed EMT • 12-lead – See CARDIAC-ECG/12 Lead Procedure A-EMT • IV – NS with standard tubing • Titrate fluid to patient’s needs – See Shock Protocol EMT-I/ • Cardiac monitoring PARAMEDIC • Pain management – See Acute Pain Management Protocol 199 March, 2021 Medical Control Board Approved Protocols This page intentionally left blank 200 March, 2021 Medical Control Board Approved Protocols ACUTE ADRENAL INSUFFICIENCY PROTOCOL 02/02/2021 Follow Assessment, General Procedures Protocol • Acute adrenal insufficiency (crisis) can occur in the following settings: - During neonatal period (undiagnosed adrenal insufficiency) - In patients with known, pre-existing adrenal insufficiency (e.g., Addison’s disease) - In patients who are chronically steroid dependent (i.e., taking steroids daily, long- term, for any number of medical conditions) - Adrenal crisis can be triggered by any acute stressor (e.g., trauma or illness), as well as by abrupt cessation of steroid use (for any reason). • Signs/symptoms of adrenal crisis: Altered mental status, seizures; generalized weakness, hypotension, hypoglycemia, hyperkalemia. • Notify hospital you are transporting known/suspected adrenal crisis patient • Emergency transport for: ALOC, hypotension, hypoglycemia, suspected hyperkalemia. Acute adrenal crisis is an immediately life-threatening emergency, and must be treated aggressively EMR • PMH, Take thorough history of patient’s steroid use/dependence. Determine if the patient is on oral hydrocortisone. • Assess and support ABC’s • Oxygen therapy, as needed • Monitor vitals EMT • Check blood glucose • If blood glucose is <60: administer glucose solution orally if the patient is awake and able to protect own airway • Obtain 12 lead ECG; if time permitted. -

Triage and Scenario
Triage and Scenario By Bryan Lewis Triage Triage: Is a rapid approach to prioritizing a large number of patients Incident Casualty Collection Triage Site Point Officer/Treatment/Transport S imple T riage A nd R apid T reatment Triage ● Triage should be performed RAPIDLY ● Utilize START Triage to determine priority ● 30–60 seconds per patient ● Affix tag on left upper arm or leg – Triage 1. Scene Safety BSI and Identify number of patients, and types of injuries, communicate to EMS 2. Clear the “walking wounded” with verbal instruction: If you can hear me and you can move, walk to… (Use a PA System if Possible) 3. Direct patients to the casualty collection point (CCP) or treatment area for detailed assessment and medical care Green Minor Manager/Triage Officer will be the area to control patients and manage area 4. Green tag will be issued at the CCP These patients may be classified as MINOR START Triage Now use START to assess and categorize the remaining patients… USE Color System START-Triage Now categorize the patients by assessing each patient’s RPMs… ✓Respirations ✓Pulse ✓Mental Status START—RPM RESPIRATIONS Is the patient breathing? Yes Adult – respirations > 30 = Red/Immediate Pediatric – respirations < 15 or > 45 = Red/Immediate Adult – respirations < 30 = check pulse Pediatric – respirations > 15 and < 45 = check pulse START—RPM RESPIRATIONS Is the Patient Breathing? No Reposition the airway… Respirations begin = IMMEDIATE/RED If patient doesn’t breath . ▪ Adult – deceased = BLACK ▪ Pediatric: Pulse Present – give 5 rescue breaths -

Paramedic Update
PARAMEDIC UPDATE 2020 AGENDA Protocol format New medications Base contact requirements Against Medical Advice Pediatric King Airway Protocol changes New Policies Determination of death Online Certifications- Image trend NEW PROTOCOL FORMAT Public safety, EMT, and Public safety personal can Adults and Pediatric are on Paramedic protocols are in only perform skills in the top the same page. one document. canary yellow section Anything listed in the yellow EMT’s can perform any skills Paramedics will start with ALS section is a standing in the green BLS section the BLS section (BLS before order. Base contact must be located below the public ALS!) and move down into attempted for anything in the safety area. the ALS section as needed. red “base hospital contact required” section. NEW PROTOCOL FORMAT Adults Pediatrics (13 years and under) Public Safety First Aid Procedures: Only Public Safety First Aid Procedures: Only • Remove nearby objects to prevent injury to Patient. Place • Remove nearby objects to prevent injury to Patient. Place patient in recovery position on left side patient in recovery position on left side • Give Oxygen if available • Give Oxygen if available • Request Fire/EMS • Request Fire/EMS • Public safety will start here BLS Procedures: EMT’s and Paramedics start here BLS Procedures: EMT’s and Paramedics start here • Support ABC’s • Support ABC’s • Give Oxygen only if Spo2 < 94% or if in Respiratory Distress • Give Oxygen only if Spo2 <94% or if in Respiratory Distress • Blood Glucose Check, if hypoglycemic enter appropriate • Blood Glucose check, if hypoglycemic enter appropriate protocol protocol • EMT and Paramedic start here • If Focal seizure, place patient in position of comfort, rapid • If Focal seizure, place patient in position of comfort, rapid transport or ALS Rendezvous transport or ALS Rendezvous • If full body tonic/clonic seizure, prepare to support • If full body tonic/clonic seizure, prepare to support respirations, provide cooling measures if febrile respirations.