Surgical Anatomy of Mandibular Third Molar
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Course of the Maxillary Artery Through the Loop Of
Anomalous course of maxillary artery Rev Arg de Anat Clin; 2013, 5 (3): 235-239 __________________________________________________________________________________________ Case Report COURSE OF THE MAXILLARY ARTERY THROUGH THE LOOP OF THE AURICULOTEMPORAL NERVE Kavya Bhat, Sampath Madhyastha*, Balakrishnan R Department of Anatomy, Kasturba Medical College, Bejai Campus, Mangalore, Manipal University, India RESUMEN INTRODUCTION Las variaciones en el curso de la arteria maxilar se describen a menudo, con sus relaciones con el Maxillary artery is one of the larger terminal músculo pterigoideo lateral. En el presente caso branches of the external carotid artery, arises informamos una variación exclusiva en el curso de la behind the neck of the mandible, within the arteria maxilar que no fue publicada antes. En un substance of the parotid gland. It then crosses cadáver masculino de 75 años arteria maxilar derecho the infratemporal fossa to enter the pterygo- estaba pasando por el bucle del nervio auriculo- palatine fossa through pterygo-maxillary fissure. temporal. La arteria meníngea media provenía de la The course of the artery is divided into three arteria maxilar con un bucle del nervio auriculo- temporal. La arteria maxilar pasaba profunda con parts by the lateral pterygoid muscle. The first respecto al nervio dentario inferior pero superficial al (mandibular) part runs horizontally, parallel to nervio lingual. El conocimiento de estas variaciones es and slightly below the auriculo-temporal nerve. importante para el cirujano y también serviría para This part of the artery runs superficial (lateral) to explicar la posible participación de estas variaciones the lower head of lateral pterygoid muscle. The en la etiología del dolor mandibular. -

Accidental Displacement of Mandibular Third Molar Root Into the Submandibular Space: a Case Report
Case Report ERA’S JOURNAL OF MEDICAL RESEARCH VOL.6 NO.1 ACCIDENTAL DISPLACEMENT OF MANDIBULAR THIRD MOLAR ROOT INTO THE SUBMANDIBULAR SPACE: A CASE REPORT Mayur Vilas Limbhore, Viren S Patil, Shandilya Ramanojam, Vrushika Mahajan, Pallavi Rathi, Kisna Tadas Department of Oral and Maxillofacial surgery Bharati Vidyapeeth Dental College, Katraj, Pune, Maharashtra, India-411030 Received on : 01-04-2018 Accpected on : 10-04-2018 ABSTRACT Address for correspondence Accidental displacement of an impacted third molar, either a crown, Dr. Mayur Vilas Limbhore root piece, or the entire tooth, is a rare complication that occurs Department of Oral and Maxillofacial Surgery during surgical removal. The most common sites of dislodgment of an impacted mandibular third molar root are the submandibular, Bharati Vidyapeth Dental College, sublingual and pterygomandibular spaces. Removal of a displaced Katraj, Pune, Maharashtra, India-411030 root from these spaces may be complex due to poor visualization Email: [email protected] and limited access. A thorough evaluation of all significant risk Contact no: +91-8552887325 factors must be performed in advance to prevent complications. This case report reveals the management of accidental displaced mandibular third molar root into the submandibular space. An 39 years-old male patient underwent a third mandibular molar extraction. Accidentally, the mandibular right third molar distal root was displaced into the submandibular space, making necessary a second surgical step. After 2 days awaiting an asymptomatic health status, the second surgical step was successfully performed using multislice CBCT as preoperative imaging guide. The present case report highlights the clinical usefulness of CBCT in proper treatment of the patient. -
Anatomical Overview
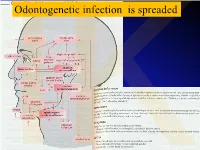
IKOdontogenetic infection is spreaded Možné projevy zlomenin a zánětů IKPossible signs of fractures or inflammations Submandibular space lies between the bellies of the digastric muscles, mandible, mylohyoid muscle and hyoglossus and styloglossus muscles IK IK IK IK IK Submandibulární absces Submandibular abscess IK Sběhlý submandibulární absces Submandibular abscess is getting down IK Submental space lies between the mylohyoid muscles and the investing layer of deep cervical fascia superficially IK IK Spatium peritonsillare IK IK Absces v peritonsilární krajině Abscess in peritonsilar region IK Fasciae Neck fasciae cervicales Demarcate spaces • fasciae – Superficial (investing): • f. nuchae, f. pectoralis, f. deltoidea • invests m. sternocleidomastoideus + trapezius • f. supra/infrahyoidea – pretrachealis (middle neck f.) • form Δ, invests infrahyoid mm. • vagina carotica (carotic sheet) – Prevertebral (deep cervical f.) • Covers scaleni mm. IK• Alar fascia Fascie Fascia cervicalis superficialis cervicales Fascia cervicalis media Fascia cervicalis profunda prevertebralis IKsuperficialis pretrachealis Neck spaces - extent • paravisceral space – Continuation of parafaryngeal space – Nervous and vascular neck bundle • retrovisceral space – Between oesophagus and prevertebral f. – Previsceral space – mezi l. pretrachealis a orgány – v. thyroidea inf./plx. thyroideus impar • Suprasternal space – Between spf. F. and pretracheal one IK– arcus venosus juguli 1 – sp. suprasternale suprasternal Spatia colli 2 – sp. pretracheale pretracheal 3 – -

Retained Surgical Items Evidence Table
Guideline for Prevention of Retained Surgical Items Evidence Table CITATION CONCLUSION(S) SAMPLE SIZE REFERENCE # POPULATION COMPARISON EVIDENCE TYPE INTERVENTIONS CONSENSUS SCORE OUTCOME MEASURE 1 Wilson C. Foreign bodies left in the Case series of foreign bodies left in the abdomen. Cases VC Literature n/a n/a n/a n/a Retained abdomen after laparotomy. Trans Am found through publication, interviews, and the author's own Review, Clinician sponges Gynecol Soc. 1884;9:94-117. experience. Experience, and Case Report 2 The Joint Commission. Preventing The Joint Commission recommends that facilities develop IVB Consensus n/a n/a n/a n/a n/a unintended retained foreign objects. effective processes and procedures for preventing Sentinel Event Alert. October 17, unintended retained foreign objects. Their recommendations 2013;51. include a standardized and highly reliable counting system; http://www.jointcommission.org/sea_i development of policies and procedures; practices for ssue_51/. Accessed November 10, counting, wound opening, and closing procedures; 2015. performance of intraoperative radiographs; use of effective communication to include briefings and debriefings; documentation of counts; and assistive technologies (ie, RF tags, RFID, radiopaque, bar coding). Also, the hospital should define a process for conducting RCA for sentinel events, such as URFO. Page 1 of 60 Guideline for Prevention of Retained Surgical Items Evidence Table CITATION CONCLUSION(S) SAMPLE SIZE REFERENCE # POPULATION COMPARISON EVIDENCE TYPE INTERVENTIONS CONSENSUS SCORE OUTCOME MEASURE 3 Moffatt-Bruce SD, Cook CH, Steinberg 7 elevated risk factors for RSI in pooled data in case-control IIIA Systematic USA hospitals, n/a n/a 3 studies: Estimated SM, Stawicki SP. -

Anatomy of Maxillary and Mandibular Local Anesthesia
Anatomy of Mandibular and Maxillary Local Anesthesia Patricia L. Blanton, Ph.D., D.D.S. Professor Emeritus, Department of Anatomy, Baylor College of Dentistry – TAMUS and Private Practice in Periodontics Dallas, Texas Anatomy of Mandibular and Maxillary Local Anesthesia I. Introduction A. The anatomical basis of local anesthesia 1. Infiltration anesthesia 2. Block or trunk anesthesia II. Review of the Trigeminal Nerve (Cranial n. V) – the major sensory nerve of the head A. Ophthalmic Division 1. Course a. Superior orbital fissure – root of orbit – supraorbital foramen 2. Branches – sensory B. Maxillary Division 1. Course a. Foramen rotundum – pterygopalatine fossa – inferior orbital fissure – floor of orbit – infraorbital 2. Branches - sensory a. Zygomatic nerve b. Pterygopalatine nerves [nasal (nasopalatine), orbital, palatal (greater and lesser palatine), pharyngeal] c. Posterior superior alveolar nerves d. Infraorbital nerve (middle superior alveolar nerve, anterior superior nerve) C. Mandibular Division 1. Course a. Foramen ovale – infratemporal fossa – mandibular foramen, Canal -> mental foramen 2. Branches a. Sensory (1) Long buccal nerve (2) Lingual nerve (3) Inferior alveolar nerve -> mental nerve (4) Auriculotemporal nerve b. Motor (1) Pterygoid nerves (2) Temporal nerves (3) Masseteric nerves (4) Nerve to tensor tympani (5) Nerve to tensor veli palatine (6) Nerve to mylohyoid (7) Nerve to anterior belly of digastric c. Both motor and sensory (1) Mylohyoid nerve III. Usual Routes of innervation A. Maxilla 1. Teeth a. Molars – Posterior superior alveolar nerve b. Premolars – Middle superior alveolar nerve c. Incisors and cuspids – Anterior superior alveolar nerve 2. Gingiva a. Facial/buccal – Superior alveolar nerves b. Palatal – Anterior – Nasopalatine nerve; Posterior – Greater palatine nerves B. -

A Guide to Complete Denture Prosthetics
A Guide to Complete Denture Prosthetics VITA shade taking VITA shade communication VITA shade reproduction VITA shade control Date of issue 11.11 VITA shade, VITA made. Foreword The aim of this Complete Denture Prosthetics Guide is to inform on the development and implementation of the fundamental principles for the fabrication of complete dentures. In this manual the reader will find suggestions concerning clnical cases which present in daily practice. Its many features include an introduction to the anatomy of the human masticatory system, explanations of its functions and problems encountered on the path to achieving well functioning complete dentures. The majority of complete denture cases which present in everyday practice can be addressed with the aid of knowledge contained in this instruction manual. Of course a central recommendation is that there be as close as possible collaboration between dentist and dental technician, both with each other and with the patient. This provides the optimum circumstances for an accurate and seamless flow of information. It follows also that to invest the time required to learn and absorb the patient’s dental history as well as follow the procedural chain in the fabrication procedure will always bring the best possible results. Complete dentures are restorations which demand a high degree of knowledge and skill from their creators. Each working step must yield the maximum result, the sum of which means an increased quality of life for the patient. In regard to the choice of occlusal concept is to be used, is a question best answered by the dentist and dental technician working together as a team. -

Adipose Stem Cells from Buccal Fat Pad and Abdominal Adipose Tissue for Bone Tissue Engineering
Adipose Stem Cells from Buccal Fat Pad and Abdominal Adipose Tissue for Bone tissue Engineering Elisabet Farré Guasch Dipòsit Legal: B-25086-2011 ISBN: 978-90-5335-394-3 http://hdl.handle.net/10803/31987 ADVERTIMENT. La consulta d’aquesta tesi queda condicionada a l’acceptació de les següents condicions d'ús: La difusió d’aquesta tesi per mitjà del servei TDX (www.tesisenxarxa.net) ha estat autoritzada pels titulars dels drets de propietat intel·lectual únicament per a usos privats emmarcats en activitats d’investigació i docència. No s’autoritza la seva reproducció amb finalitats de lucre ni la seva difusió i posada a disposició des d’un lloc aliè al servei TDX. No s’autoritza la presentació del seu contingut en una finestra o marc aliè a TDX (framing). Aquesta reserva de drets afecta tant al resum de presentació de la tesi com als seus continguts. En la utilització o cita de parts de la tesi és obligat indicar el nom de la persona autora. ADVERTENCIA. La consulta de esta tesis queda condicionada a la aceptación de las siguientes condiciones de uso: La difusión de esta tesis por medio del servicio TDR (www.tesisenred.net) ha sido autorizada por los titulares de los derechos de propiedad intelectual únicamente para usos privados enmarcados en actividades de investigación y docencia. No se autoriza su reproducción con finalidades de lucro ni su difusión y puesta a disposición desde un sitio ajeno al servicio TDR. No se autoriza la presentación de su contenido en una ventana o marco ajeno a TDR (framing). -

Anatomy of the Pterygomandibular Space — Clinical Implication and Review
FOLIA MEDICA CRACOVIENSIA 79 Vol. LIII, 1, 2013: 79–85 PL ISSN 0015-5616 MARCIN LIPSKI1, WERONIKA LIPSKA2, SYLWIA MOTYL3, Tomasz Gładysz4, TOMASZ ISKRA1 ANATOMY OF THE PTERYGOMANDIBULAR SPACE — CLINICAL IMPLICATION AND REVIEW Abstract: A i m: The aim of this study was to present review of the pterygomandibular space with some referrals to clinical practice, specially to the methods of lower teeth anesthesia. C o n c l u s i o n s: Pterygomandibular space is a clinically important region which is commonly missing in anatomical textbooks. More attention should be paid to it both from theoretical and practical point of view, especially in teaching the students of first year of dental studies. Key words: pterygomandibular space, Gow-Gates anesthesia, inferior alveolar nerve. INTRODUCTION Numerous cranial regions have been subjects of various anatomical and anthro- pological studies [1, 2]. Most of them indicate necessity of undertaking of such studies first of all because of clinical importance [3–5]. Inferior alveolar nerve blocs, one of the most common procedures in dentistry requires deep anatomical knowledge of the pterygomandibular space [6, 7]. This space is a narrow gap, which contains mostly loose areolar tissue. It communi- cates however through the mandibular foramen with the mandibular canal, which is traversed by inferior alveolar nerve, artery and comitant vein (IANAV). Many of the structures placed in this space are of certain importance for local anesthesia. Khoury at al. [8, 9] mention here the following: inferior alveolar nerve, artery and vein, lingual nerve, nerve to mylohyoid and the sphenomandibular ligament. The space contains mostly loose areolar tissue. -

Morfofunctional Structure of the Skull
N.L. Svintsytska V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 Ministry of Public Health of Ukraine Public Institution «Central Methodological Office for Higher Medical Education of MPH of Ukraine» Higher State Educational Establishment of Ukraine «Ukranian Medical Stomatological Academy» N.L. Svintsytska, V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 2 LBC 28.706 UDC 611.714/716 S 24 «Recommended by the Ministry of Health of Ukraine as textbook for English- speaking students of higher educational institutions of the MPH of Ukraine» (minutes of the meeting of the Commission for the organization of training and methodical literature for the persons enrolled in higher medical (pharmaceutical) educational establishments of postgraduate education MPH of Ukraine, from 02.06.2016 №2). Letter of the MPH of Ukraine of 11.07.2016 № 08.01-30/17321 Composed by: N.L. Svintsytska, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor V.H. Hryn, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor This textbook is intended for undergraduate, postgraduate students and continuing education of health care professionals in a variety of clinical disciplines (medicine, pediatrics, dentistry) as it includes the basic concepts of human anatomy of the skull in adults and newborns. Rewiewed by: O.M. Slobodian, Head of the Department of Anatomy, Topographic Anatomy and Operative Surgery of Higher State Educational Establishment of Ukraine «Bukovinian State Medical University», Doctor of Medical Sciences, Professor M.V. -

The Mandibular Nerve - Vc Or VIII by Prof
The Mandibular Nerve - Vc or VIII by Prof. Dr. Imran Qureshi The Mandibular nerve is the third and largest division of the trigeminal nerve. It is a mixed nerve. Its sensory root emerges from the posterior region of the semilunar ganglion and is joined by the motor root of the trigeminal nerve. These two nerve bundles leave the cranial cavity through the foramen ovale and unite immediately to form the trunk of the mixed mandibular nerve that passes into the infratemporal fossa. Here, it runs anterior to the middle meningeal artery and is sandwiched between the superior head of the lateral pterygoid and tensor veli palatini muscles. After a short course during which a meningeal branch to the dura mater, and the nerve to part of the medial pterygoid muscle (and the tensor tympani and tensor veli palatini muscles) are given off, the mandibular trunk divides into a smaller anterior and a larger posterior division. The anterior division receives most of the fibres from the motor root and distributes them to the other muscles of mastication i.e. the lateral pterygoid, medial pterygoid, temporalis and masseter muscles. The nerve to masseter and two deep temporal nerves (anterior and posterior) pass laterally above the medial pterygoid. The nerve to the masseter continues outward through the mandibular notch, while the deep temporal nerves turn upward deep to temporalis for its supply. The sensory fibres that it receives are distributed as the buccal nerve. The 1 | P a g e buccal nerve passes between the medial and lateral pterygoids and passes downward and forward to emerge from under cover of the masseter with the buccal artery. -

The Buccal Fat Pad: Importance and Function
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 15, Issue 6 Ver. XIII (June. 2016), PP 79-81 www.iosrjournals.org The Buccal Fat Pad: Importance And Function Ulduz Zamani Ahari1, Hosein Eslami2, Parisa Falsafi*2, Aila Bahramian2, Saleh Maleki1 1. Post Graduate Student Of Oral Medicine, Dental Faculty, Tabriz University Of Medical Science, Tabriz, Iran. 2.Department Of Oral Medicine, Dental Faculty, Tabriz University Of Medical Science, Tabriz, Iran. ●Corresponding Author Email:[email protected] Abstract: The buccal fat is an important anatomic structure intimately related to the masticatory muscles, facial nerve , and parotid duct.while anatomically complex , an understanding of its boundaries will allow the surgeon to safely manipulate this structure in reconstructive and aesthetic procedures . Technically, the buccal fat pad is easily accessed and moblized . It is does not cause any noticeable defect in the cheek or mouth, and it can be performed in a very short time and without causing complication for the patient. The pedicled BFP graft is more resistant to infection than other kinds of free graft and will result in very success. The buccal fat pad has a satisfactory vascular supply , This property of graft and other properties will allow for the closure of defects that cannot be repaired by conventional procedures. The buccal fat pad exposed through an intraoral and buccal incision , has several clinical application including aesthetic improvement , close of oroantral and Oroantral defects reconstruction of surgical defects and palatal cleft defects and palatal cleft defects , reconstruction of maxilla and palatal defects. -

PERFORATION of INFERIOR ALVEOLAR NERVE by MAXILLARY ARTERY Prakash Billakanti Babu, Ramachandra Bhat K, Vanishree S Nayak
Inferior alveolar nerve Rev Arg de Anat Clin; 2011, 3 (3): 124-129 __________________________________________________________________________________________ Case report PERFORATION OF INFERIOR ALVEOLAR NERVE BY MAXILLARY ARTERY Prakash Billakanti Babu, Ramachandra Bhat K, Vanishree S Nayak Kasturba Medical College, Manipal University, Manipal, Karnataka, India RESUMEN La fosa infratemporal es un área anatómica inferior alveolar nerve originated from the clínicamente importante para la administración de mandibular nerve by two roots and the first part agentes anestésicos locales en odontología y cirugía of the maxillary artery was incorporated between maxilofacial. Fueron estudiadas variaciones en la them. An embryologic origin of this variation and anatomía del nervio alveolar inferior y la arteria maxilar its clinical implications is discussed. Because the en la disección infratemporal. Durante la disección rutinaria de la cabeza en el cadáver de un varón maxillary artery runs between the two roots of the adulto, fue observada una variación excepcional en el inferior alveolar nerve, and the nerve was fixed origen del nervio alveolar inferior y su relación con las between the foramen ovale and mandibular estructuras circundantes. El nervio alveolar inferior se foramen, neurovascular entrapment may cause originaba en el nervio mandibular por dos raíces y la pain numbness or headache and may interfere primera parte de la arteria maxilar estaba incorporada with the injection of local anesthetics into the entre ambas. El origen embriológico de esta variación infratemporal fossa. Anatomical variations in this y sus implicaciones clínicas es debatido. Dado que la region should be kept in mind, particularly in arteria maxilar transcurría entre las dos raíces del cases of failed treatment of trigeminal neuralgia.