The Production of Medical Isotopes Without Nuclear Reactors Or Uranium Enrichment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Role of Combined Therapy in the Treatment of Retinopathy and Optic Neuropathy Due to Radiotherapy in the Uveal Melanoma
Published online: 2020-01-16 THIEME Original Article 1 The Role of Combined Therapy in the Treatment of Retinopathy and Optic Neuropathy Due to Radiotherapy in the Uveal Melanoma Yasemin Benderli Cihan1 1Department of Radiation Oncology, Kayseri Education and Address for correspondence Yasemin Benderli Cihan, MD, Department Research Hospital, Kayseri, Turkey of Radiation Oncology, Kayseri Education and Research Hospital, Sanayi District, Ataturk Boulevard, Hastane Street, No 78, 38010 Kocasinan, Kayseri, Turkey (e-mail: [email protected]). Asian J Oncol 2020;6:1–2 Abstract Introduction Uveal melanoma has a relatively low incidence. Transpupillary thermo- therapy (TTT), hypofractioned stereotactic radiotherapy (RT), stereotactic radiosur- gery, plaque brachytherapy, charged particle radiation therapy, local tumor resection, enucleation, and exantation are applied in the treatment. Methods The importance given to radiotherapy has increased to get more satisfac- tory results while treating the patient. However, it is the treatment of radiation reti- nopathy and optic neuropathy from complications. Results Radiation retinopathy and optic neuropathy are the most important compli- Keywords cations related to radiotherapy in the treatment of uveal melanoma. In recent years, ► uveal melanoma many studies have been performed on the treatment of radiation retinopathy and ► radiotherapy optic neuropathy. ► retinopathy Conclusion The consecutive use of triamcinolone in combination with anti-VEGF ► optic neuropathy supports that it may be a future therapeutic agent in the treatment of complications. Introduction was found to be 81.6%.2 The 2-, 5-, and 10-year metastasis rates were reported to be 10%, 25%, and 34%, respectively, regardless Uveal melanoma is the most common primary intraocular of tumor size.3 tumor in adults. -

Royal Society of Chemistry Input to the Ad Hoc Nuclear
ROYAL SOCIETY OF CHEMISTRY INPUT TO THE AD HOC NUCLEAR RESEARCH AND DEVELOPMENT ADVISORY BOARD The Royal Society of Chemistry (RSC) was pleased to hear of the instigation of the Ad Hoc Nuclear Research and Development Advisory Board (the Board) following the findings of the House of Lords Science and Technology Committee Inquiry ‘Nuclear Research and Development Capabilities’.1,2 The RSC is the largest organisation in Europe for advancing the chemical sciences. Supported by a network of 47,000 members worldwide and an internationally acclaimed publishing business, its activities span education and training, conferences and science policy, and the promotion of the chemical sciences to the public. This document represents the views of the RSC. The RSC has a duty under its Royal Charter "to serve the public interest" by acting in an independent advisory capacity, and it is in this spirit that this submission is made. To provide input to the Board the RSC has performed a wide consultation with the chemical science community, including members of both our Radiochemistry and Energy Sector Interest Groups and also our Environment Sustainability and Energy Division. September 2012 The Role of Chemistry in a Civil Nuclear Strategy 1 Introduction Chemistry and chemical knowledge is essential in nuclear power generation and nuclear waste management. It is essential that a UK civil nuclear strategy recognises the crucial role that chemistry plays, both in research and innovation and in the development of a strong skills pipeline. As the RSC previously articulated in our response to the House of Lords Inquiry, 3 nuclear power is an important component of our current energy mix. -
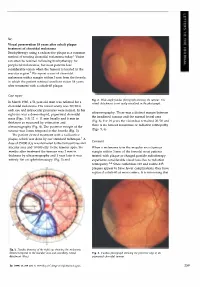
Case Report Comment
Sir, Visual preservation 18 years after cobalt plaque treatment of choroidal melanoma Brachytherapy using a radioactive plaque is a common method of treating choroidal melanoma today.l Vision can often be retained following brachytherapy for peripheral melanomas, but most patients lose considerable vision when the tumour is located in the macular region.2 We report a case of choroidal melanoma with a margin within 3 mm from the foveola in which the patient retained excellent vision 18 years after treatment with a cobalt-60 plaque. Case report Fig. 2. Wide-angle fundus photograph showing the tumour. The In March 1980, a 51-year-old man was referred for a retinal detachment is not easily visualised in the photograph. choroidal melanoma. His visual acuity was 20/20 in each eye and intraocular pressures were normal. In his ultrasonography. There was a distinct margin between right eye was a dome-shaped, pigmented choroidal the irradiated tumour and the normal foveal area mass (Figs. 1-3) 12 X 11 mm basally and 6 mm in (Fig. 6). For 18 years the vision has remained 20/20 and thickness as measured by estimation and there is no tumour recurrence or radiation retinopathy ultrasonography (Fig. 4). The posterior margin of the (Figs. 5, 6). tumour was 3 mm temporal to the foveola (Fig. 3). The patient elected treatment with a radioactive plaque, which was done by our standard technique. 1 A Comment dose of 35 000 cGy was delivered to the tumour base and macular area and 10 000 cGy to the tumour apex. Six When a melanoma is in the macular area (tumour months after treatment the tumour was 2 mm in margin within 3 mm of the foveola) most patients thickness by ultrasonography and 1 year later it was treated with plaque or charged particle radiotherapy entirely flat on ophthalmoscopy (Fig. -

Nuclear Chemistry Card Sort
Nuclear Chemistry Card Sort Submitted by: Annette Gillespie, Ashely Gilomen, Sarah Johnson, and Stephanie Kimberlin Appalachian Regional Commission/Oak Ridge National Laboratory Summer Math-Science-Technology Institute Grade: 9-12 Lesson Duration: 45-60 minutes Materials Needed: • Media for Venn Diagram (e.g., poster board, white board, butcher paper, electronic devices) • One copy of the list of nuclear chemistry concepts/nuclear chemistry concept cards provided in this lesson plan • Envelope for storing cut-up list/cards Background Information: Students should be able to describe the basic structure of an atom and have a basic understanding of nuclear notation. Lesson Objective: Students will be able to • Describe the basic principles of nuclear chemistry. • Discern between diagrams and representations of nuclear equations and processes. • Use context clues to correctly categorize nuclear events. Instructional Process: All informative resources should be made available to the students so they can categorize the concepts (e.g., notes, text books, Internet). This lesson is best suited as an introduction activity for the beginning of the nuclear chemistry unit and/or as a review activity at the end of the nuclear chemistry unit. Students should be organized into groups of 3-4 to complete this activity. Each student group should create and label a three-circle Venn diagram on the teacher-designated media. (Refer to the examples provided in figure 1 and at the end of this lesson plan.) Each group should receive one copy of the list of nuclear chemistry concepts/nuclear chemistry concept cards, which they will cut up into individual cards. Once students have their diagrams drawn and cards cut out, they should place the nuclear chemistry concepts cards into one of three categories on the diagram: fission, fusion, or nuclear decay. -
Unit 1 – Atomic Structure and Nuclear Chemistry Introduction to the Atom
Unit 1 – Atomic Structure and Nuclear Chemistry Introduction to the atom Modern Atomic Theory All matter is composed of atoms Atoms cannot be subdivided, created, or destroyed in ordinary chemical reactions. However, these changes CAN occur in nuclear reactions! Every atom has different properties from other atoms Ex: grinding down a gold ring Modern Atomic Theory Wait, it’s “only” a theory? Why are we learning it then? •A theory is a powerful term in science Theory -A set of tested hypotheses that gives an overall explanation of some natural phenomenon. Ex: Cell theory & Evolutionary theory We can now see atoms …sort of In 1981 a STM (Scanning Tunneling Microscope) was created. - We can see them and manipulate them. The Kanji characters for "atom." This image was formed by using the tiny tip of an STM to pick up individual atoms of iron and place them on a copper (111) surface. Nanotechnology is coming Atoms can be moved and molded to make various devices such as molecular motors Structure of the Atom Accessing Prior Knowledge 1. Based on your previous science classes, draw a generic atom and label where you’d find the nucleus, protons, neutrons, & electrons. 2. For a common beryllium atom, what is the: a) # protons? b) # neutrons? c) # electrons? Structure of an Atom Electrons (in electron cloud) 1/2000th the mass of P+ & N Nucleus (protons + neutrons) Particle Charge Mass Location Purpose # Electron -1 0 Electron Behavior of cloud element Proton +1 1 Nucleus Identity of element Neutron 0 1 Nucleus Stability of nucleus Charges in an Atom The atom is generally neutral because: # of negative electrons = # of positive protons The nucleus is positively charged because: Contains positive protons (and neutrons which don’t have a charge). -

Annual Report of Institute of Nuclear Chemistry and Technology 1996
PL9702079 ISSN 1425-ZU4A IN/&~PL- 003 INSTITUTE OF NUCLEAR CHEMISTRY AND TECHNOLOGY m DO /? WMEM\ 1996 OF NUCLEI AND TECHNOLOGY 1996 EDITORIAL BOARD Wiktor Smuiek, Ph.D. Ewa Godlewska Sylwester Wojtas © Copyright by the Institute of Nuclear Chemistry and Technology, Warszawa 1997 All rights reserved CONTENTS GENERAL INFORMATION 7 MANAGEMENT OF THE INSTITUTE 9 MANAGING STAFF OF THE INSTITUTE 9 HEADS OF THE INCT DEPARTMENTS 9 PROFESSORS AND SCIENTIFIC COUNCIL 10 PROFESSORS 10 ASSOCIATE PROFESSORS 10 ASSISTANT PROFESSORS (Ph.D.) 11 SCIENTIFIC COUNCIL (1995-1999) 13 HONORARY MEMBERS OF THE INCT SCIENTIFIC COUNCIL (1995-1999) 14 RADIATION CHEMISTRY AND PHYSICS 15 ONE-ELECTRON OXIDATION OF METALLOPORPHYCENES AS STUDIED BY RADIOLYTIC METHODS D M. Guldi, J. Field, J. Grodkowski, P. Neta, E. Vogel 17 IRON-PORPHYRIN CATALYZED REDUCTION OF CO& PHOTOCHEMICAL AND RADIATION CHEMICAL STUDIES J. Grodkowski, D. Behar, P. Neta, P. Hambright 17 RATE CONSTANTS FOR REACTIONS OF ALIPHATIC CARBON-CENTERED RADICALS IN AQUEOUS SOLUTION P. Neta, J. Grodkowski, A.B. Ross 19 TETRABENZOPORPHYRINS: METAL INCORPORATION AND EXCHANGE KINETICS, LIGATIONAL EQUILIBRIA AND PULSE RADIOLYSIS STUDY S. Cromer, P. Hambright, J. Grodkowski, P. Neta 19 REDUCTION AND ALKYLATION OF RHODIUM PORPHYRINS IN ALCOHOL SOLUTIONS. RADIATION CHEMICAL AND PHOTOCHEMICAL STUDIES J. Grodkowski, P. Neta, Y. Abdallach, P. Hambright 20 •OH RADICAL INDUCED OXIDATION OF S-METHYLCYSTEINE AND ITS DERIVATIVES FRAGMENTATION OF a-AMINOALKYL RADICALS D. Pogocki, K. Bobrowski, K.-D. Asmus 21 Trp ' -* iyrO RADICAL TRANSFOMATION IN HEN-EGG WHITE LYSOZYME K. Bobrowski, J. Holcman, J. Poznafiski, K.L. Wierzchowski 24 SENSITIZED PHOTOOXIDATION OF METHIONINE-CONTAINING PEPTIDES IN AQUEOUS SOLUTION K. -

Introduction to Nuclear Chemistry
Nuclear Reactions: Chemistry 5.1 AN INTRODUCTION TO NUCLEAR CHEMISTRY Discovery of Radioactivity Roentgen ● In 1895 Wilhelm Konrad Roentgen discovered X- rays. • Roentgen observed that a vacuum discharge tube enclosed in a thin, black cardboard box had caused a nearby piece of paper coated with the salt barium platinocyanide to phosphorescence. Roentgen ● From this and other experiments he concluded that certain rays, which he called X-rays, were emitted from the discharge tube, penetrated the box, and caused the salt to glow. Becquerel ● Shortly after Roentgen’s discovery, Antoine Henri Becquerel attempted to show a relationship between X-rays and the phosphorescence of uranium salts. • Becquerel wrapped a photographic plate in black paper, sprinkled a sample of a uranium salt on it, and exposed it to sunlight. Becquerel ● When Becquerel attempted to repeat the experiment the sunlight was intermittent. • He took the photographic plate wrapped in black paper with the uranium sample on it, and placed the whole setup in a drawer. Becquerel ● Several days later he developed the film and was amazed to find an intense image of the uranium salt on the plate. • He repeated the experiment in total darkness with the same result. Becquerel ● This proved that the uranium salt emitted rays that affected the photographic plate, and that these rays were not a result of phosphorescence due to exposure to sunlight. • One year later, in 1896, Marie Curie coined the name radioactivity. Radioactivity is the spontaneous emission of particlesElements and/or having rays this fromproperty the nucleusare radioactive of an . atom. Rutherford ● In 1899 Rutherford began to investigate the nature of the rays emitted by uranium. -

2/22/19 1 Chapter 6, Energy from Alternate Sources: Nuclear
2/22/19 Chapter 6, Energy from Alternate Sources: nuclear chemistry and solar power End of the chapter questions 3.5,9,12,13,16,17,20,22,23,27,31,40 Friday, March 25, 2011, 10AM CDT Breach in reactor suspected at Japanese nuke plant TOKYO – A suspected breach in the reactor at the stricken Fukushima nuclear plant could mean more serious radioactive contamination, Japanese officials revealed Friday, as the prime minister called the country's ongoing fight to stabilize the plant "very grave and serious." 1 2/22/19 The Chernobyl disaster On 26 April 1986, reactor # 4 at the Chernobyl Nuclear Power Station, 60 mi north of Kiev, blew up during a routine daily operation. Nearly nine tons of radioactive material - 100 times as much as the Hiroshima bomb - were hurled into the sky. Winds over the following days, mostly blowing north and west, carried fallout into Belarus, Russia, Poland and the Baltic region. The cause was traced to graphite control rods, which caught on fire. Chernobyl-What Happened: April 26, 1986 • While performing a safety test on Reactor #4, technicians allowed a power surge that reached 120 times the rated capacity of the reactor. • The surge (in fact not a nuclear explosion), ripped open the core, including cooling water pipes. The reaction of hot water with the graphite control rods produced hydrogen gas, which combusted violently. • The 4,000 ton concrete covering over the reactor was blown away. Fires broke out in many places in the site. • Fifty different radioactive isotopes were released, with half-lives spanning from two hours to 24,000 years. -

Nuclear Chemistry Why? Nuclear Chemistry Is the Subdiscipline of Chemistry That Is Concerned with Changes in the Nucleus of Elements
Nuclear Chemistry Why? Nuclear chemistry is the subdiscipline of chemistry that is concerned with changes in the nucleus of elements. These changes are the source of radioactivity and nuclear power. Since radioactivity is associated with nuclear power generation, the concomitant disposal of radioactive waste, and some medical procedures, everyone should have a fundamental understanding of radioactivity and nuclear transformations in order to evaluate and discuss these issues intelligently and objectively. Learning Objectives λ Identify how the concentration of radioactive material changes with time. λ Determine nuclear binding energies and the amount of energy released in a nuclear reaction. Success Criteria λ Determine the amount of radioactive material remaining after some period of time. λ Correctly use the relationship between energy and mass to calculate nuclear binding energies and the energy released in nuclear reactions. Resources Chemistry Matter and Change pp. 804-834 Chemistry the Central Science p 831-859 Prerequisites atoms and isotopes New Concepts nuclide, nucleon, radioactivity, α− β− γ−radiation, nuclear reaction equation, daughter nucleus, electron capture, positron, fission, fusion, rate of decay, decay constant, half-life, carbon-14 dating, nuclear binding energy Radioactivity Nucleons two subatomic particles that reside in the nucleus known as protons and neutrons Isotopes Differ in number of neutrons only. They are distinguished by their mass numbers. 233 92U Is Uranium with an atomic mass of 233 and atomic number of 92. The number of neutrons is found by subtraction of the two numbers nuclide applies to a nucleus with a specified number of protons and neutrons. Nuclei that are radioactive are radionuclides and the atoms containing these nuclei are radioisotopes. -

Curium Chemistry's Curious Conundrum Mark Jensen, Department of Chemistry and Nuclear Science and Engineering Program, Colorad
Curium Chemistry’s Curious Conundrum Mark Jensen, Department of Chemistry and Nuclear Science and Engineering Program, Colorado School of Mines. Wednesday, September 9 2015 4pm Hill Hall 202 Abstract. The separation of curium from americium is a potential component of advanced, transmutation- based nuclear fuel cycles because it greatly simplifies fuel re-fabrication. However, separating curium from americium is among the most difficult separations in the periodic table. Chemical separations of americium from curium have typically relied either on chromatography to amplify the small chemical differences between Am(III) and Cm(III) through repeated separation, or on accessing the higher oxidation states of Am to affect a separation of Am from Cm(III). We are exploring a third way to separate Am from Cm. Using sterically constrained complexes to amplify the small thermodynamic differences normally observed between Am(III) and Cm(III) complexes, we can separate these ions efficiently based on their slightly different ionic radii. Sterically constrained aqueous complexes that are size-matched to the larger Am(III) cation preferentially hold back americium in the aqueous phase while allowing extraction of the smaller Cm(III) cation. Improvements in the system hold promise for cleanly separating americium from both curium and lanthanide fission products in a single process. Biography. Mark Jensen is the Jerry and Tina Grandey University Chair in Nuclear Science and Engineering, Professor of Chemistry, and Director of the Nuclear Science and Engineering Program at the Colorado School of Mines. He earned a Ph.D. in inorganic and nuclear chemistry from the Florida State University studying the environmental chemistry of radioactive waste. -

Actinide Overview
2 Meet the Presenter… Alena Paulenova Dr. Alena Paulenova is Associate Professor in the Department of Nuclear Engineering and Director of the Laboratory of Transuranic Elements at the OSU Radiation Center. She is also Adjunct Professor at the Department of Chemistry at Oregon State University , a Joint Research faculty with Idaho National Laboratory, Division of Aqueous Separations and Radiochemistry and a member of the INEST Fuel Cycle Core Committee. She received her Ph.D. in Physical Chemistry in 1985 from the Moscow/Kharkov State University. Until 1999, she was a faculty member at the Department of Nuclear Chemistry and Radioecology of Comenius University in Bratislava, then a visiting scientist at Clemson University and Washington State University in Pullman. In 2003 she joined the faculty at OSU as a Coordinator of the Radiochemistry Program at OSU Radiation Center to bring her experience to the task of helping to educate a new generation of radiochemists: http://oregonstate.edu/~paulenoa/. Her research interest has focused on application of radioanalytical and spectroscopic methods to speciation of radionuclides in aqueous and organic solutions and development of separation methods for spent nuclear fuel cycle processing, decontamination and waste minimization. The main efforts of her research group are fundamental studies of the kinetics and thermodynamics of the complexation of metals, primary actinides and fission products, with organic and inorganic ligands and interactions with redox active species, and the effects of radiolysis and hydrolysis in these systems. Contact: (+1) 541-737-7070 E-mail: [email protected]. An Overview of Actinide Chemistry Alena Paulenova National Analytical Management Program (NAMP) U.S. -

Diagnosis, and Treatment of Retinoblastoma
British3'ournal ofOphthalmology 1993; 77: 805-812 805 PERSPECTIVE Br J Ophthalmol: first published as 10.1136/bjo.77.12.805 on 1 December 1993. Downloaded from Applications ofmonoclonal antibodies in the investigation, diagnosis, and treatment of retinoblastoma John F Tarlton, D L Easty In Europe and North America, retinoblastoma has a reported derived cell lines fused with RB1 competent cells.2' Reversal incidence ranging from 1 in 14 000 to 1 in 36 000 live births'-5 of malignancy has also been reported in cell lines transfected and is the most common ocular malignancy affecting children with functional BR1 gene constructs. Recently, however, and infants. Early diagnosis allows the application of a these results have been challenged by other researchers who number of therapies directed at localised disease, including have found incomplete reversal of malignancy in retino- external beam and plaque radiotherapy, cryotherapy, and blastoma cell lines,22 although such effects may be artefacts photocoagulation, although the principal treatment account- resulting from additional genetic changes having occurred in ing for the high cure rate ofaround 90% is enucleation, which cells adapting to tissue culture environments. The impor- is still carried out in over halfofall cases. The justification for tance of RB1 in malignant transformation has also been such radical therapy is the poor prognosis once the tumour demonstrated by inactivating its product by association with escapes the eye, and the high mortality from metastases.6 virus proteins such as adenovirus EIA,23 SV40 large T In the developing countries ofAfrica and Asia the picture is antigen24 and papillomavirus E7 oncoprotein,2" both by different.