Radiation Therapy Coding
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Role of Combined Therapy in the Treatment of Retinopathy and Optic Neuropathy Due to Radiotherapy in the Uveal Melanoma
Published online: 2020-01-16 THIEME Original Article 1 The Role of Combined Therapy in the Treatment of Retinopathy and Optic Neuropathy Due to Radiotherapy in the Uveal Melanoma Yasemin Benderli Cihan1 1Department of Radiation Oncology, Kayseri Education and Address for correspondence Yasemin Benderli Cihan, MD, Department Research Hospital, Kayseri, Turkey of Radiation Oncology, Kayseri Education and Research Hospital, Sanayi District, Ataturk Boulevard, Hastane Street, No 78, 38010 Kocasinan, Kayseri, Turkey (e-mail: [email protected]). Asian J Oncol 2020;6:1–2 Abstract Introduction Uveal melanoma has a relatively low incidence. Transpupillary thermo- therapy (TTT), hypofractioned stereotactic radiotherapy (RT), stereotactic radiosur- gery, plaque brachytherapy, charged particle radiation therapy, local tumor resection, enucleation, and exantation are applied in the treatment. Methods The importance given to radiotherapy has increased to get more satisfac- tory results while treating the patient. However, it is the treatment of radiation reti- nopathy and optic neuropathy from complications. Results Radiation retinopathy and optic neuropathy are the most important compli- Keywords cations related to radiotherapy in the treatment of uveal melanoma. In recent years, ► uveal melanoma many studies have been performed on the treatment of radiation retinopathy and ► radiotherapy optic neuropathy. ► retinopathy Conclusion The consecutive use of triamcinolone in combination with anti-VEGF ► optic neuropathy supports that it may be a future therapeutic agent in the treatment of complications. Introduction was found to be 81.6%.2 The 2-, 5-, and 10-year metastasis rates were reported to be 10%, 25%, and 34%, respectively, regardless Uveal melanoma is the most common primary intraocular of tumor size.3 tumor in adults. -
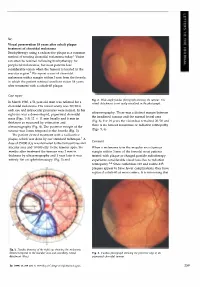
Case Report Comment
Sir, Visual preservation 18 years after cobalt plaque treatment of choroidal melanoma Brachytherapy using a radioactive plaque is a common method of treating choroidal melanoma today.l Vision can often be retained following brachytherapy for peripheral melanomas, but most patients lose considerable vision when the tumour is located in the macular region.2 We report a case of choroidal melanoma with a margin within 3 mm from the foveola in which the patient retained excellent vision 18 years after treatment with a cobalt-60 plaque. Case report Fig. 2. Wide-angle fundus photograph showing the tumour. The In March 1980, a 51-year-old man was referred for a retinal detachment is not easily visualised in the photograph. choroidal melanoma. His visual acuity was 20/20 in each eye and intraocular pressures were normal. In his ultrasonography. There was a distinct margin between right eye was a dome-shaped, pigmented choroidal the irradiated tumour and the normal foveal area mass (Figs. 1-3) 12 X 11 mm basally and 6 mm in (Fig. 6). For 18 years the vision has remained 20/20 and thickness as measured by estimation and there is no tumour recurrence or radiation retinopathy ultrasonography (Fig. 4). The posterior margin of the (Figs. 5, 6). tumour was 3 mm temporal to the foveola (Fig. 3). The patient elected treatment with a radioactive plaque, which was done by our standard technique. 1 A Comment dose of 35 000 cGy was delivered to the tumour base and macular area and 10 000 cGy to the tumour apex. Six When a melanoma is in the macular area (tumour months after treatment the tumour was 2 mm in margin within 3 mm of the foveola) most patients thickness by ultrasonography and 1 year later it was treated with plaque or charged particle radiotherapy entirely flat on ophthalmoscopy (Fig. -

STI/PUB/1153 Vol. 2
STANDARDS AND CODES OF PRACTICE IN MEDICAL RADIATION DOSIMETRY VOLUME 2 ALL BLANK PAGES HAVE BEEN RETAINED INTENTIONALLY IN THIS WEB VERSION. BLANK PROCEEDINGS SERIES STANDARDS AND CODES OF PRACTICE IN MEDICAL RADIATION DOSIMETRY PROCEEDINGS OF AN INTERNATIONAL SYMPOSIUM HELD IN VIENNA, AUSTRIA, 25–28 NOVEMBER 2002, ORGANIZED BY THE INTERNATIONAL ATOMIC ENERGY AGENCY, CO-SPONSORED BY THE EUROPEAN COMMISSION (DIRECTORATE-GENERAL ENVIRONMENT), THE EUROPEAN SOCIETY FOR THERAPEUTIC RADIOLOGY AND ONCOLOGY, THE INTERNATIONAL ORGANIZATION FOR MEDICAL PHYSICS AND THE PAN AMERICAN HEALTH ORGANIZATION, AND IN CO-OPERATION WITH THE AMERICAN ASSOCIATION OF PHYSICISTS IN MEDICINE, THE EUROPEAN FEDERATION OF ORGANISATIONS FOR MEDICAL PHYSICS, THE INTERNATIONAL COMMISSION ON RADIATION UNITS AND MEASUREMENTS, THE INTERNATIONAL SOCIETY FOR RADIATION ONCOLOGY AND THE WORLD HEALTH ORGANIZATION In two volumes VOLUME 2 INTERNATIONAL ATOMIC ENERGY AGENCY VIENNA, 2003 Permission to reproduce or translate the information contained in this publication may be obtained by writing to the International Atomic Energy Agency,Wagramer Strasse 5, P.O. Box 100,A-1400 Vienna,Austria. © IAEA, 2003 IAEA Library Cataloguing in Publication Data International Symposium on Standards and Codes of Practice in Medical Radiation Dosimetry (2002 : Vienna, Austria) Standards and codes of practice in medical radiation dosimetry : proceedings of an international symposium held in Vienna, Austria, 25–28 November 2002 / organized by the International Atomic Energy Agency ; co-sponsored by the European Commission, Directorate- General Environment...[et al.]. In 2 vols. — Vienna: The Agency, 2003. 2 v. ; 24 cm. — (Proceedings series, ISSN 0074–1884) Contents : v. 2. STI/PUB/1153 ISBN 92–0–111403–6 Includes bibliographical references. 1. -
Intercomparison Procedures in the Dosmetry of And
INTERCOMPARISON PROCEDURES DOSMETRE TH N I F YO HIGH-ENERGY X-RAY AND ELECTRON BEAMS REPOR ADVISORN A F TO Y GROUP MEETING ORGANIZED BY THE INTERNATIONAL ATOMIC ENERGY AGENCY AND HELD IN VIENNA 2-6 APRIL 1979 A TECHNICAL DOCUMENT ISSUEE TH Y DB INTERNATIONAL ATOMIC ENERGY AGENCY, VIENNA, 1981 The IAEA does not maintain stocks of reports in this series. However, microfiche copies of these reports can be obtained from IN IS Microfiche Clearinghouse International Atomic Energy Agency Wagramerstrasse5 0 10 P.Ox Bo . A-1400 Vienna, Austria on prepayment of Austrian Schillings 25.50 or against one IAEA microfiche service coupon to the value of US S2.00. CONTENTS REPORT AND RECOMMENDATIONS OF THE ADVISORY GROUP Repor recommendationd an t Advisore th f so y Group..................7 . APPENDI . I XIAEA/WH O postal dose intercomparison (TLD) for high energy X-ray therapy. Instruction sheet................7 1 . APPENDI . XII IAEA/WH O postal dose intercomparison (TLD) for high energy X-ray therapy. Data sheet........................ 21 EXPERIENCE WITH AND THE NEED FOR DOSE INTERCOMPARISONS The IAEA/WHO thermoluminescent dosimetry intercomparison used for the improvemen clinicaf o t l dosimetry ............................7 2 . N.T. Racoveanu A surve f clinicallo y y applied dosimetry (Summary e reporth n o t IAEA/WHO postal dose intercomparison of cobalt-60 telecurie units with TLD) ........................................................3 3 . Seelenta. W g Dose intercomparison programm Regionae th f o e l Reference Centre of Argentina ...................................................... 45 R. Gonzalez, M.S. de Fernandez Gianotti Experience in intercomparison at an SSDL for orthovoltage and high energy beams ................................................. 51 G. -

Radiation Dose in Radiotherapy from Prescription to Delivery
IAEA-TECDOC-896 XA9642841 Radiation dose in radiotherapy from prescription to delivery INTERNATIONAL ATOMIC ENERGY AGENCY The originating Section of this publication in the IAEA was: Dosimetry Section International Atomic Energy Agency Wagramerstrasse 5 P.O. Box 100 A-1400 Vienna, Austria RADIATION DOSE IN RADIOTHERAPY FROM PRESCRIPTION TO DELIVERY IAEA, VIENNA, 1996 IAEA-TECDOC-896 ISSN 1011-4289 © IAEA, 1996 Printed by the IAEA in Austria August 1996 The IAEA does not normally maintain stocks of reports in this series. However, microfiche copies of these reports can be obtained from INIS Clearinghouse International Atomic Energy Agency Wagramerstrasse 5 P.O. Box 100 A-1400 Vienna, Austria Orders should be accompanied by prepayment of Austrian Schillings 100, in the form of a cheque or in the form of IAEA microfiche service coupons which may be ordered separately from the INIS Clearinghouse. FOREWORD Cancer incidence is increasing in developed as well as in developing countries. However, since in some advanced countries the cure rate is increasing faster than the cancer incidence rate, the cancer mortality rate is no longer increasing in such countries. The increased cure rate can be attributed to early diagnosis and improved therapy. On the other hand, until recently, in some parts of the world - particularly in developing countries - cancer control and therapy programmes have had relatively low priority. The reason is the great need to control communicable diseases. Today a rapidly increasing number of these diseases are under control. Thus, cancer may be expected to become a prominent problem and this will result in public pressure for higher priorities on cancer care. -

Diagnosis, and Treatment of Retinoblastoma
British3'ournal ofOphthalmology 1993; 77: 805-812 805 PERSPECTIVE Br J Ophthalmol: first published as 10.1136/bjo.77.12.805 on 1 December 1993. Downloaded from Applications ofmonoclonal antibodies in the investigation, diagnosis, and treatment of retinoblastoma John F Tarlton, D L Easty In Europe and North America, retinoblastoma has a reported derived cell lines fused with RB1 competent cells.2' Reversal incidence ranging from 1 in 14 000 to 1 in 36 000 live births'-5 of malignancy has also been reported in cell lines transfected and is the most common ocular malignancy affecting children with functional BR1 gene constructs. Recently, however, and infants. Early diagnosis allows the application of a these results have been challenged by other researchers who number of therapies directed at localised disease, including have found incomplete reversal of malignancy in retino- external beam and plaque radiotherapy, cryotherapy, and blastoma cell lines,22 although such effects may be artefacts photocoagulation, although the principal treatment account- resulting from additional genetic changes having occurred in ing for the high cure rate ofaround 90% is enucleation, which cells adapting to tissue culture environments. The impor- is still carried out in over halfofall cases. The justification for tance of RB1 in malignant transformation has also been such radical therapy is the poor prognosis once the tumour demonstrated by inactivating its product by association with escapes the eye, and the high mortality from metastases.6 virus proteins such as adenovirus EIA,23 SV40 large T In the developing countries ofAfrica and Asia the picture is antigen24 and papillomavirus E7 oncoprotein,2" both by different. -

Chapter 5. Treatment Machines for External Beam Radiotherapy
Review of Radiation Oncology Physics: A Handbook for Teachers and Students CHAPTER 5. TREATMENT MACHINES FOR EXTERNAL BEAM RADIOTHERAPY ERVIN B. PODGORSAK Department of Medical Physics McGill University Health Centre Montréal, Québec, Canada 5.1. INTRODUCTION Since the inception of radiotherapy soon after the discovery of x-rays by Roentgen in 1895, the technology of x-ray production has first been aimed toward ever higher photon and electron beam energies and intensities, and more recently toward computerization and intensity-modulated beam delivery. During the first 50 years of radiotherapy, the techno- logical progress has been relatively slow and mainly based on x-ray tubes, Van de Graaff generators and betatrons. The invention of the cobalt-60 teletherapy unit by H.E. Johns in Canada in the early 1950s provided a tremendous boost in the quest for higher photon energies, and placed the cobalt unit into the forefront of radiotherapy for a number of years. The concurrently developed medical linear accelerators (linacs), however, soon eclipsed the cobalt unit, moved through five increasingly sophisticated generations, and became the most widely used radiation source in modern radiotherapy. With its compact and efficient design, the linac offers excellent versatility for use in radiotherapy through isocentric mounting and provides either electron or megavoltage x-ray therapy with a wide range of energies. In addition to linacs, electron and x-ray radiotherapy is also carried out with other types of accelerators, such as betatrons and microtrons. More exotic particles, such as protons, neutrons, heavy ions, and negative π mesons, all produced by special accelerators, are also sometimes used for radiotherapy; however, most of the contemporary radiotherapy is carried out with linacs or teletherapy cobalt units. -
Book of Extended Synopses
International Symposium on Standards, Applications and Quality Assurance in Medical Radiation Dosimetry (IDOS 2019) 18–21 June 2019 Vienna, Austria Book of Extended Synopses Organized by the CN-273 TABLE OF CONTENTS ORAL PRESENTATIONS Small Field Dosimetry Implementation of the International Code of Practice on Dosimetry of Small Static Fields used in External Beam Radiotherapy (TRS-483) ........................................................... 11 Detector Choice for Depth Dose Curves Including the Build-Up Region of Small MV Photon Fields .................................................................................................................. 15 Output Correction Factors for Eight Ionization Chambers in Small Static Photon Fields ........................................................................................................................................ 17 Reference Dosimetry of a New Biology-Guided Radiotherapy (BgRT) System Following the IAEA TRS-483 CoP ................................................................................................. 20 Uncertainty Contributors in the Dosimetry of Small Static Fields................................. 23 Small Field Photon Beams Audit Pilot Study: Preliminary Results .............................. 25 On the Implementation of the Plan Class-Specific Reference Field Concept Using Multidimensional Clustering of Plan Features ............................................................... 27 Computational Dosimetry Determination of Wair in High-Energy Clinical Electron -

Radiotherapy of Conjunctival Melanoma: Role and Challenges of Brachytherapy, Photon-Beam and Protontherapy
applied sciences Review Radiotherapy of Conjunctival Melanoma: Role and Challenges of Brachytherapy, Photon-Beam and Protontherapy Corrado Spatola 1,2, Rocco Luca Emanuele Liardo 2, Roberto Milazzotto 2 , Luigi Raffaele 2, Vincenzo Salamone 2, Antonio Basile 1,2, Pietro Valerio Foti 1,2, Stefano Palmucci 1,2 , Giuseppe Antonio Pablo Cirrone 3, Giacomo Cuttone 3, Andrea Russo 4 , Teresio Avitabile 4, Michele Reibaldi 5 , Antonio Longo 4, Giuseppe Broggi 1 , Vincenza Bonfiglio 6, Rosario Caltabiano 1 , Stefano Pergolizzi 7 and Floriana Arena 7,* 1 Dipartimento di Scienze Mediche, Chirurgiche e Tecnologie Avanzate “G.F. Ingrassia”, Università di Catania, 95125 Catania, Italy; [email protected] (C.S.); [email protected] (A.B.); [email protected] (P.V.F.); [email protected] (S.P.); [email protected] (G.B.); [email protected] (R.C.) 2 UO Radiodiagnostica e Radioterapia Oncologica AOU Policlinico-S.Marco Catania, 95125 Catania, Italy; [email protected] (R.L.E.L.); [email protected] (R.M.); raff[email protected] (L.R.); [email protected] (V.S.) 3 Istituto Nazionale di Fisica Nucleare-LNS Catania, 95125 Catania, Italy; [email protected] (G.A.P.C.); [email protected] (G.C.) 4 Dipartimento di Chirurgia Generale e Specialità Medico-Chirurgiche, Università di Catania, 95125 Catania, Italy; [email protected] (A.R.); [email protected] (T.A.); [email protected] (A.L.) 5 Dipartimento di Oftalmologia, Università di Torino, 10124 Torino, Italy; [email protected] 6 Dipartimento -

An Overview of Auger-Electron Radionuclide Therapy
Current Drug Discovery Technologies, 2010, 7, 000-000 1 Targeting the Nucleus: An Overview of Auger-Electron Radionuclide Therapy Bart Cornelissen* and Katherine A Vallis MRC/CRUK Gray Institute for Radiation Oncology and Biology, University of Oxford, Oxford, United Kingdom Abstract: The review presented here lays out the present state of the art in the field of radionuclide therapies specifically targeted against the nucleus of cancer cells, focussing on the use of Auger-electron-emitters. Nuclear localisation of radi- onuclides increases DNA damage and cell kill, and, in the case of Auger-electron therapy, is deemed necessary for thera- peutic effect. Several strategies will be discussed to direct radionuclides to the nucleoplasm, even to specific protein tar- gets within the nucleus. An overview is given of the applications of Auger-electron-emitting radionuclide therapy target- ing the nucleus. Finally, a few suggestions are made as how radioimmunotherapy with nuclear targets can be improved, and the challenges that might be met, such as how to perform accurate dosimetry measurements, are examined. Keywords: Auger-electron, radionuclide, radioimmunotherapy, nucleus, targeted radiotherapy, molecular radiotherapy, PRRT. 1. INTRODUCTION tumour from within. Because of tumour-specific delivery, radionuclide therapy is also called targeted or molecular ra- The management of solid cancers relies on a combination diotherapy (tRT). Where antibodies or peptides are used to of surgery, systemic chemotherapy and locally delivered guide the radionuclide to epitopes or receptors on malignant radiotherapy. External beam X-ray radiotherapy (XRT) is cells, the terms radioimmunotherapy (RIT) or peptide recep- used in approximately 50% of all cancer patients as it is able tor radionuclide therapy (PRRT) are used, respectively. -

(12) Patent Application Publication (10) Pub. No.: US 2009/0156881 A1 Stokes (43) Pub
US 20090156881A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2009/0156881 A1 Stokes (43) Pub. Date: Jun. 18, 2009 (54) CONVERGENT WELL IRRADIATING Publication Classification PLAOUE FOR CHOROIDAL MELANOMA (51) Int. Cl. (76) Inventor: John P. Stokes, San Antonio, TX A6M 36/12 (2006.01) (US) A6DF 9/00 (2006.01) (52) U.S. Cl. ............................................................ 6OOf7 Correspondence Address: MEYERTONS, HOOD, KIVLIN, KOWERT & (57) ABSTRACT GOETZEL, P.C. Provided in some embodiments is a device suitable for treat P.O. BOX 398 ing an eye that includes a housing and a plurality offins. The AUSTIN, TX 78767-0398 (US) housing includes a base and a rim coupled to the perimeter of the base. The base and the rim at least partially define a cavity (21) Appl. No.: 12/252,136 in the housing, and the cavity is configured to accept one or more radiation seeds. The plurality of fins at least partially (22) Filed: Oct. 15, 2008 reside within or proximate the cavity of the housing. At least a portion of the fins are configured such that radiation emitted Related U.S. Application Data from one or more radiation seeds positioned in the cavity is (60) Provisional application No. 60/980,079, filed on Oct. substantially directed toward a center portion of the eye dur 15, 2007. ing use. SClera ChOroid Patent Application Publication Jun. 18, 2009 Sheet 1 of 8 US 2009/O156881 A1 C-H > O wis w CN Sa CNwas O C v N. l e CD VN sU O S & U wal w- F S S wis,N ws Patent Application Publication Jun. -

Comparison of Retinoblastoma Reduction for Chemotherapy Vs External Beam Radiotherapy
CLINICAL SCIENCES Comparison of Retinoblastoma Reduction for Chemotherapy vs External Beam Radiotherapy Daniel A. Sussman, MD; Erika Escalona-Benz, MD; Matthew S. Benz, MD; Brandy C. Hayden, BS; William Feuer, MS; Nicole Cicciarelli; Stuart Toledano, MD; Arnold Markoe, MD; Timothy G. Murray, MD Objective: To determine the time course and extent of Results: Twenty-six eyes of 26 patients were evaluated tumor reduction associated with systemic chemo- for tumor response; 18 patients were treated with sys- therapy or external beam radiotherapy (EBRT) in the treat- temic chemotherapy and 8 patients were treated with ment of advanced intraocular retinoblastoma. EBRT. Median follow-up was 36 months. A mean 68% reduction in tumor volume occurred after 1 cycle of che- Methods: Retrospective review of children with Reese- motherapy compared with a 12% reduction at a similar Ellsworth stages IV and V retinoblastoma undergoing pri- time point (1 month) after initiation of EBRT (PϽ.004). mary globe-conserving therapy with either systemic che- There was no statistically significant difference in tu- moreduction or EBRT. Study variables were recorded at mor volume reduction between treatment modalities at baseline, at monthly intervals for the first 6 months, and the 12-month follow-up visit. Both systemic chemore- at 12 months after the initiation of treatment. Tumor vol- duction and EBRT achieved 100% globe conservation and umes were calculated using basal area and height values 100% patient survival in this series. determined by ultrasonography, physical examination, and fundus photographic review. Conclusions: Retinoblastoma reduction exhibits a dif- ferential time course based on the applied primary treat- Main Outcome Measures: Outcome measures in- ment.