STI/PUB/1153 Vol. 2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Intercomparison Procedures in the Dosmetry of And
INTERCOMPARISON PROCEDURES DOSMETRE TH N I F YO HIGH-ENERGY X-RAY AND ELECTRON BEAMS REPOR ADVISORN A F TO Y GROUP MEETING ORGANIZED BY THE INTERNATIONAL ATOMIC ENERGY AGENCY AND HELD IN VIENNA 2-6 APRIL 1979 A TECHNICAL DOCUMENT ISSUEE TH Y DB INTERNATIONAL ATOMIC ENERGY AGENCY, VIENNA, 1981 The IAEA does not maintain stocks of reports in this series. However, microfiche copies of these reports can be obtained from IN IS Microfiche Clearinghouse International Atomic Energy Agency Wagramerstrasse5 0 10 P.Ox Bo . A-1400 Vienna, Austria on prepayment of Austrian Schillings 25.50 or against one IAEA microfiche service coupon to the value of US S2.00. CONTENTS REPORT AND RECOMMENDATIONS OF THE ADVISORY GROUP Repor recommendationd an t Advisore th f so y Group..................7 . APPENDI . I XIAEA/WH O postal dose intercomparison (TLD) for high energy X-ray therapy. Instruction sheet................7 1 . APPENDI . XII IAEA/WH O postal dose intercomparison (TLD) for high energy X-ray therapy. Data sheet........................ 21 EXPERIENCE WITH AND THE NEED FOR DOSE INTERCOMPARISONS The IAEA/WHO thermoluminescent dosimetry intercomparison used for the improvemen clinicaf o t l dosimetry ............................7 2 . N.T. Racoveanu A surve f clinicallo y y applied dosimetry (Summary e reporth n o t IAEA/WHO postal dose intercomparison of cobalt-60 telecurie units with TLD) ........................................................3 3 . Seelenta. W g Dose intercomparison programm Regionae th f o e l Reference Centre of Argentina ...................................................... 45 R. Gonzalez, M.S. de Fernandez Gianotti Experience in intercomparison at an SSDL for orthovoltage and high energy beams ................................................. 51 G. -

Radiation Dose in Radiotherapy from Prescription to Delivery
IAEA-TECDOC-896 XA9642841 Radiation dose in radiotherapy from prescription to delivery INTERNATIONAL ATOMIC ENERGY AGENCY The originating Section of this publication in the IAEA was: Dosimetry Section International Atomic Energy Agency Wagramerstrasse 5 P.O. Box 100 A-1400 Vienna, Austria RADIATION DOSE IN RADIOTHERAPY FROM PRESCRIPTION TO DELIVERY IAEA, VIENNA, 1996 IAEA-TECDOC-896 ISSN 1011-4289 © IAEA, 1996 Printed by the IAEA in Austria August 1996 The IAEA does not normally maintain stocks of reports in this series. However, microfiche copies of these reports can be obtained from INIS Clearinghouse International Atomic Energy Agency Wagramerstrasse 5 P.O. Box 100 A-1400 Vienna, Austria Orders should be accompanied by prepayment of Austrian Schillings 100, in the form of a cheque or in the form of IAEA microfiche service coupons which may be ordered separately from the INIS Clearinghouse. FOREWORD Cancer incidence is increasing in developed as well as in developing countries. However, since in some advanced countries the cure rate is increasing faster than the cancer incidence rate, the cancer mortality rate is no longer increasing in such countries. The increased cure rate can be attributed to early diagnosis and improved therapy. On the other hand, until recently, in some parts of the world - particularly in developing countries - cancer control and therapy programmes have had relatively low priority. The reason is the great need to control communicable diseases. Today a rapidly increasing number of these diseases are under control. Thus, cancer may be expected to become a prominent problem and this will result in public pressure for higher priorities on cancer care. -

Chapter 5. Treatment Machines for External Beam Radiotherapy
Review of Radiation Oncology Physics: A Handbook for Teachers and Students CHAPTER 5. TREATMENT MACHINES FOR EXTERNAL BEAM RADIOTHERAPY ERVIN B. PODGORSAK Department of Medical Physics McGill University Health Centre Montréal, Québec, Canada 5.1. INTRODUCTION Since the inception of radiotherapy soon after the discovery of x-rays by Roentgen in 1895, the technology of x-ray production has first been aimed toward ever higher photon and electron beam energies and intensities, and more recently toward computerization and intensity-modulated beam delivery. During the first 50 years of radiotherapy, the techno- logical progress has been relatively slow and mainly based on x-ray tubes, Van de Graaff generators and betatrons. The invention of the cobalt-60 teletherapy unit by H.E. Johns in Canada in the early 1950s provided a tremendous boost in the quest for higher photon energies, and placed the cobalt unit into the forefront of radiotherapy for a number of years. The concurrently developed medical linear accelerators (linacs), however, soon eclipsed the cobalt unit, moved through five increasingly sophisticated generations, and became the most widely used radiation source in modern radiotherapy. With its compact and efficient design, the linac offers excellent versatility for use in radiotherapy through isocentric mounting and provides either electron or megavoltage x-ray therapy with a wide range of energies. In addition to linacs, electron and x-ray radiotherapy is also carried out with other types of accelerators, such as betatrons and microtrons. More exotic particles, such as protons, neutrons, heavy ions, and negative π mesons, all produced by special accelerators, are also sometimes used for radiotherapy; however, most of the contemporary radiotherapy is carried out with linacs or teletherapy cobalt units. -
Book of Extended Synopses
International Symposium on Standards, Applications and Quality Assurance in Medical Radiation Dosimetry (IDOS 2019) 18–21 June 2019 Vienna, Austria Book of Extended Synopses Organized by the CN-273 TABLE OF CONTENTS ORAL PRESENTATIONS Small Field Dosimetry Implementation of the International Code of Practice on Dosimetry of Small Static Fields used in External Beam Radiotherapy (TRS-483) ........................................................... 11 Detector Choice for Depth Dose Curves Including the Build-Up Region of Small MV Photon Fields .................................................................................................................. 15 Output Correction Factors for Eight Ionization Chambers in Small Static Photon Fields ........................................................................................................................................ 17 Reference Dosimetry of a New Biology-Guided Radiotherapy (BgRT) System Following the IAEA TRS-483 CoP ................................................................................................. 20 Uncertainty Contributors in the Dosimetry of Small Static Fields................................. 23 Small Field Photon Beams Audit Pilot Study: Preliminary Results .............................. 25 On the Implementation of the Plan Class-Specific Reference Field Concept Using Multidimensional Clustering of Plan Features ............................................................... 27 Computational Dosimetry Determination of Wair in High-Energy Clinical Electron -
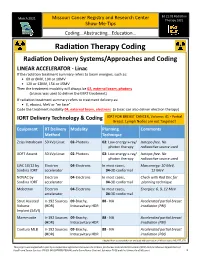
Radiation Therapy Coding
Ed 21:01 Radiation March 2021 Missouri Cancer Registry and Research Center Therapy 2021 Show-Me-Tips Coding...Abstracting...Education… Radiation Therapy Coding Radiation Delivery Systems/Approaches and Coding LINEAR ACCELERATOR - Linac If the radiation treatment summary refers to beam energies, such as: • 6X or 6MV, 10X or 10MV • 12X or 12MV, 15X or 15MV Then the treatment modality will always be 02, external beam, photons (a Linac was used to deliver the EBRT treatment) If radiation treatment summary refers to treatment delivery as: • E, eboost, MeV or “en face” Code the treatment modality 04, external beam, electrons (a Linac can also deliver electron therapy) IORT Delivery Technology & Coding IORT FOR BREAST CANCER, Volume: 41 - Partial Breast. Lymph Nodes are not Targeted! Equipment RT Delivery Modality Planning Comments Method Technique Zeiss Intrabeam 50 kVp Linac 02-Photons 02: Low energy x-ray/ Isotope-free. No photon therapy radioactive source used XOFT Axxent 50 kVp Linac 02-Photons 02: Low energy x-ray/ Isotope-free. No photon therapy radioactive source used LIAC 10/12 by Electron 04-Electrons In most cases, Max energy: 10 MeV, Sordina IORT accelerator 04-3D conformal 12 MeV NOVAC by Electron 04-Electrons In most cases, Check with Rad Onc for Sordina IORT accelerator 04-3D conformal planning technique Mobetron Electron 04-Electrons In most cases, Energies: 6, 9, 12 MeV accelerator 04-3D conformal Strut Assisted Ir-192 Sources 09-Brachy, 88 - NA Accelerated partial breast Volume (HDR) Intracavitary HDR irradiation (PBI) Implant -

An Overview of Auger-Electron Radionuclide Therapy
Current Drug Discovery Technologies, 2010, 7, 000-000 1 Targeting the Nucleus: An Overview of Auger-Electron Radionuclide Therapy Bart Cornelissen* and Katherine A Vallis MRC/CRUK Gray Institute for Radiation Oncology and Biology, University of Oxford, Oxford, United Kingdom Abstract: The review presented here lays out the present state of the art in the field of radionuclide therapies specifically targeted against the nucleus of cancer cells, focussing on the use of Auger-electron-emitters. Nuclear localisation of radi- onuclides increases DNA damage and cell kill, and, in the case of Auger-electron therapy, is deemed necessary for thera- peutic effect. Several strategies will be discussed to direct radionuclides to the nucleoplasm, even to specific protein tar- gets within the nucleus. An overview is given of the applications of Auger-electron-emitting radionuclide therapy target- ing the nucleus. Finally, a few suggestions are made as how radioimmunotherapy with nuclear targets can be improved, and the challenges that might be met, such as how to perform accurate dosimetry measurements, are examined. Keywords: Auger-electron, radionuclide, radioimmunotherapy, nucleus, targeted radiotherapy, molecular radiotherapy, PRRT. 1. INTRODUCTION tumour from within. Because of tumour-specific delivery, radionuclide therapy is also called targeted or molecular ra- The management of solid cancers relies on a combination diotherapy (tRT). Where antibodies or peptides are used to of surgery, systemic chemotherapy and locally delivered guide the radionuclide to epitopes or receptors on malignant radiotherapy. External beam X-ray radiotherapy (XRT) is cells, the terms radioimmunotherapy (RIT) or peptide recep- used in approximately 50% of all cancer patients as it is able tor radionuclide therapy (PRRT) are used, respectively. -

2020 VERSION 4 FINAL Practice Guideline Radiotherapy Skin Care Llv1
SCoTHE SOCIETY & COLLEGER OF RADIOGRAPHERS The Society and College of Radiographers Practice Guideline Document Radiation Dermatitis Guidelines for Radiotherapy Healthcare Professionals Second revised edition April 2020 Review date: 2025 ISBN: 978-1-909802-49-0 Endorsed by © The Society and College of Radiographers 2020. Material may only be reproduced from this publication with clear acknowledgement that it is the original source. If text is being translated into another language or languages, please include a reference/link to the original English-language text. Contents Page Executive summary 1 1. Introduction 4 2. Scope and purpose 8 3. Guideline question 8 4. Guideline development process 8 5. Guideline methodology 9 6. Radiotherapy skin care 26 7. Guideline recommendations 28 8. Implementation strategies 32 9. Recommendations for future research 33 10. Date of publication, review and updating 34 11. References 35 12. List of appendices (separate documents) Appendix 1 Group members Appendix 2 Stakeholder consultation combined and outcomes Appendix 3 External stakeholder comment form Appendix 4 2014 Systematic review 2014 Appendix 5 2014 On-going trails table (1) Appendix 6 2014 On-going trials table (2) Appendix 7 2019 Summary of evidence table Appendix 8 2019 Review summary of evidence table Appendix 9 Other interventions Appendix 10 Staff infosheet skin care Appendix 11 Staff infosheet skin care A5 leaflet Appendix 11 Staff infosheet skin care A5 leaflet – PRINT READY Appendix 12 Patient information sheet Appendix 13 Patient infosheet skin care A5 leaflet Appendix 13 Patient infosheet skin care A5 leaflet – PRINT READY Appendix 14 Skin care presentation Oncology Nursing Society (UKONS) colleagues have been involved in the writing of this document and UKONS recognises it as expert guidelines. -
Aapm Report No
AAPM REPORT NO. 249 (Revision of AAPM Report No. 90) Essentials and Guidelines for Clinical Medical Physics Residency Training Programs Report from the Work Group on Periodic Review of Medical Physics Residency Training October 2013 DISCLAIMER: This publication is based on sources and information believed to be reliable, but the AAPM and the editors disclaim any warranty or liability based on or relating to the contents of this publication. The AAPM does not endorse any products, manufacturers, or suppliers. Nothing in this publication should be interpreted as implying such endorsement. © 2013 by American Association of Physicists in Medicine DISCLAIMER: This publication is based on sources and information believed to be reliable, but the AAPM, the editors, and the publisher disclaim any warranty or liability based on or relating to the contents of this publication. The AAPM does not endorse any products, manufacturers, or suppliers. Nothing in this publication should be interpreted as implying such endorsement. ISBN-13: 978-1-936366-25-5 © 2013 by American Association of Physicists in Medicine All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means (electronic, mechanical, photocopying, recording, or otherwise) without the prior written permission of the publisher. Published by American Association of Physicists in Medicine One Physics Ellipse College Park, MD 20740-3846 ESSENTIALS AND GUIDELINES FOR CLINICAL MEDICAL PHYSICS RESIDENCY TRAINING PROGRAMS Report from the Work Group on Periodic Review of Medical Physics Residency Training Members: Joann I. Prisciandaro, Ph.D. (Work Group Chair) University of Michigan, Ann Arbor, Michigan Charles E. -

Design and Production of 3D Printed Bolus for Electron Radiation Therapy
DESIGN AND PRODUCTION OF 3D PRINTED BOLUS FOR ELECTRON RADIATION THERAPY by Shiqin Su Submitted in partial fulfillment of the requirements for the degree of Master of Science at Dalhousie University Halifax, Nova Scotia August 2014 © Copyright by Shiqin Su, 2014 Table of Contents LIST OF TABLES .......................................................................................................... vi LIST OF FIGURES ....................................................................................................... vii ABSTRACT................................................................................................................... xiv LIST OF ABBREVIATIONS AND SYMBOLS USED ............................................ xvi ACKNOWLEDGEMENTS ......................................................................................... xix Chapter 1 INTRODUCTION ..........................................................................................1 1.1 Cancer Treatment with Radiation..........................................................................1 1.1.1 Types of radiation therapies.......................................................................2 1.1.2 Beam generation in a linear accelerator.....................................................3 1.1.3 Treatment Planning....................................................................................8 1.2 Electron Beam Radiation Therapy ......................................................................10 1.2.1 Use of bolus in electron therapy ..............................................................12 -

A Perspective on the Radiopharmaceutical Requirements for Imaging and Therapy of Glioblastoma
A perspective on the radiopharmaceutical requirements for imaging and therapy of glioblastoma Julie Bolcaen1, Janke Kleynhans2,3, Shankari Nair1, Jeroen Verhoeven4, Ingeborg Goethals5, Mike Sathekge2,3, Charlot Vandevoorde1 and Thomas Ebenhan2,6 1Radiobiology, Radiation Biophysics Division, Nuclear Medicine Department, iThemba LABS, Cape Town, South Africa 2Nuclear Medicine Research Infrastructure NPC, Pretoria, South Africa 3Nuclear Medicine Department, University of Pretoria and Steve Biko Academic Hospital, Pretoria, South Africa 4Laboratory of Radiopharmacy, Ghent University, Ghent, Belgium. 5Ghent University Hospital, Department of Nuclear Medicine, Ghent, Belgium 6Nuclear Medicine Department, University of Pretoria, Pretoria, South Africa Corresponding author: [email protected] | [email protected] +27 12 354 4713 | +27 79 770 2531 1 Abstract Despite numerous clinical trials and pre-clinical developments, the treatment of glioblastoma (GB) remains a challenge. The current survival rate of GB averages one year, even with an optimal standard of care. However, the future promises efficient patient-tailored treatments, including targeted radionuclide therapy (TRT). Advances in radiopharmaceutical development have unlocked the possibility to assess disease at the molecular level allowing individual diagnosis. This leads to the possibility of choosing a tailored, targeted approach for therapeutic modalities. Therapeutic modalities based on radiopharmaceuticals are an exciting development with great potential to promote a personalised approach to medicine. However, an effective targeted radionuclide therapy (TRT) for the treatment of GB entails caveats and requisites. This review provides an overview of existing nuclear imaging and TRT strategies for GB. A critical discussion of the optimal characteristics for new GB targeting therapeutic radiopharmaceuticals and clinical indications are provided. Considerations for target selection are discussed, i.e. -

7 Clinical Applications of High-Energy Electrons
Clinical Applications of High-Energy Electrons 135 7 Clinical Applications of High-Energy Electrons Bruce J. Gerbi CONTENTS 7.8 Special Electron Techniques 159 7.8.1 Electron Arc Irradiation 159 7.1 Introduction 135 7.8.2 Craniospinal Irradiation 160 7.2 Historical Perspective 135 7.8.3 Total Skin Electron Therapy 162 7.3 Electron Interactions 136 References 164 7.4 Central Axis Percentage Depth-Dose Distributions 137 7.4.1 Central Axis Percentage Depth–Dose Dependence on Beam Energy 138 7.4.2 Central Axis Percentage Depth–Dose 7.1 Dependence on Field Size and SSD 138 7.4.3 Flatness and Symmetry – Introduction Off-Axis Characteristics 139 7.5 Isodose Curves 140 The basic physics of electron beams has been dis- 7.5.1 Change in Isodose Curves Versus SSD 141 cussed in several books and in several excellent 7.5.2 Change in Isodose Curves Versus Angle of chapters of standard radiation therapy textbooks Beam Incidence 142 Khan Hogstrom Strydom 7.5.3 Irregular Surfaces 142 ( 2003; 2004; et al. 2003). 7.6 Effect of Inhomogeneities on As with many of these previous works, the purpose Electron Distributions 143 of this chapter is to discuss the role of electron 7.6.1 Lungs 144 beams in radiation therapy, describe their physical 7.6.2 Bones 144 characteristics, and describe how this information is 7.6.3 Air Cavities 145 7.7 Clinical Applications of Electron Beams 146 relevant to clinical practice in radiation therapy. In 7.7.1 Target Definition 146 addition, several techniques using electron beams 7.7.2 Therapeutic Range – Selection of Beam Energy 147 that have been found to be useful in clinical settings 7.7.3 Dose Prescription – ICRU 71 147 will also be presented. -

Targeted Alpha Therapy: Progress in Radionuclide Production, Radiochemistry, and Applications
pharmaceutics Review Targeted Alpha Therapy: Progress in Radionuclide Production, Radiochemistry, and Applications Bryce J. B. Nelson 1, Jan D. Andersson 1,2 and Frank Wuest 1,* 1 Department of Oncology, University of Alberta, 11560 University Ave, Edmonton, AB T6G 1Z2, Canada; [email protected] (B.J.B.N.); [email protected] (J.D.A.) 2 Edmonton Radiopharmaceutical Center, Alberta Health Services, 11560 University Ave, Edmonton, AB T6G 1Z2, Canada * Correspondence: [email protected]; Tel.: +1-780-391-7666; Fax: +1-780-432-8483 Abstract: This review outlines the accomplishments and potential developments of targeted alpha (α) particle therapy (TAT). It discusses the therapeutic advantages of the short and highly ionizing path of α-particle emissions; the ability of TAT to complement and provide superior efficacy over existing forms of radiotherapy; the physical decay properties and radiochemistry of common α-emitters, including 225Ac, 213Bi, 224Ra, 212Pb, 227Th, 223Ra, 211At, and 149Tb; the production techniques and proper handling of α-emitters in a radiopharmacy; recent preclinical developments; ongoing and completed clinical trials; and an outlook on the future of TAT. Keywords: targeted alpha therapy; alpha particle therapy; targeted radionuclide therapy; theranos- tics; actinium-225; bismuth-213; astatine-211; radium-223; thorium-227; terbium-149 1. Introduction Radionuclide therapy has been employed frequently in the past several decades Citation: Nelson, B.J.B.; Andersson, for disease control, curative therapy, and pain management applications [1]. Targeted J.D.; Wuest, F. Targeted Alpha radionuclide therapy (TRT) is advantageous as it delivers a highly concentrated dose to a Therapy: Progress in Radionuclide tumor site—either directly to the tumor cells or to its microenvironment—while sparing Production, Radiochemistry, and the healthy surrounding tissues.