PE2092 Mastocytosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Living with Mast Cell Activation Syndrome
Anne Maitland, MD, PhD Living with Medical Director, Comprehensive Allergy Mast Cell & Asthma Care Activation Asst Professor, Dept of Medicine – Clinical Immunology Syndrome Icahn School of Medicine at Mt Sinai, New York Got MCAS? Mast Cell mediated disorders are common u 1 out of 2 of us are coping with some chronic immune mediated disorder. o ‘allergies’(rhinitis), sinus infections, hives (urticaria),food allergy/intolerance, skin swelling (angioedema), Anaphylaxis Signs and Symptoms eczema (atopic dermatitis and contact dermatitis), asthma issues, and the prototype of immediate hypersensitivity syndromes, anaphylaxis Why the rise in hypersensitivity disorders? Our genes in this environment! The human race has come to dominate its environment so completely that any analysis of the increase or appearance of a disease has to take changes in our lifestyle into account. In the case of allergic disease [hypersensitivity disorders] changes in our environment, diet, water quality, and personal behavior over the last 150 years have played a dominant role in the specificity of these diseases, as well as in prevalence and severity… it is clear that the consequences of hygiene, indoor entertainment, and changes in diet or physical activity have never been predicted. Thomas A. E. Platts-Mills, MD, PhD, FRS, The allergy epidemics: 1870-2010; J Allergy Clin Immunol 2015;136:3-13. Why? Trauma Stress Infection Connective Tissue Chemical Disorder exposure PIDD -manufactured Autoimmune Dz. -mold, Mastocytosis mycotoxins Hypertryptasemia (naturally Atopic Disorders occuring) Mast cell activation syndrome is easily treated, if it's But most patients with recognized MCAD suffer for Patients with mast cell activation syndrome (MCAS) frequently go for years without an accurate diagnosis… Harding, Reuters Health-New York, 2011 years… It is very common for one hypersensitivity condition to progress/morph into another, be provoked by more triggers. -

RD-Action Matchmaker – Summary of Disease Expertise Recorded Under
Summary of disease expertise recorded via RD-ACTION Matchmaker under each Thematic Grouping and EURORDIS Members’ Thematic Grouping Thematic Reported expertise of those completing the EURORDIS Member perspectives on Grouping matchmaker under each heading Grouping RD Thematically Rare Bone Achondroplasia/Hypochondroplasia Achondroplasia Amelia skeletal dysplasia’s including Achondroplasia/Growth hormone cleidocranial dysostosis, arthrogryposis deficiency/MPS/Turner Brachydactyly chondrodysplasia punctate Fibrous dysplasia of bone Collagenopathy and oncologic disease such as Fibrodysplasia ossificans progressive Li-Fraumeni syndrome Osteogenesis imperfecta Congenital hand and fore-foot conditions Sterno Costo Clavicular Hyperostosis Disorders of Sex Development Duchenne Muscular Dystrophy Ehlers –Danlos syndrome Fibrodysplasia Ossificans Progressiva Growth disorders Hypoparathyroidism Hypophosphatemic rickets & Nutritional Rickets Hypophosphatasia Jeune’s syndrome Limb reduction defects Madelung disease Metabolic Osteoporosis Multiple Hereditary Exostoses Osteogenesis imperfecta Osteoporosis Paediatric Osteoporosis Paget’s disease Phocomelia Pseudohypoparathyroidism Radial dysplasia Skeletal dysplasia Thanatophoric dwarfism Ulna dysplasia Rare Cancer and Adrenocortical tumours Acute monoblastic leukaemia Tumours Carcinoid tumours Brain tumour Craniopharyngioma Colon cancer, familial nonpolyposis Embryonal tumours of CNS Craniopharyngioma Ependymoma Desmoid disease Epithelial thymic tumours in -

Dermatofibrosarcoma Protuberans in a Male Infant
Pediatric Case Reports Dermatofibrosarcoma Protuberans in a Male Infant Leslie Peard, Nicholas G. Cost, and Amanda F. Saltzman Dermtofibrosarcoma protuberans is a rare cutaneous malignancy known to be locally aggressive. It is uncommonly seen in the pediatric population and can be difficult to distinguish from other benign skin lesions. We present a case of dermatofi- brosarcoma protuberans of the penis in a 6-month-old child managed with surgical resection. This case highlights the challenges of diagnosis of genital lesions in children and the complexities of genitourinary reconstruction following surgical resection. UROLOGY 129: 206−209, 2019. © 2018 Elsevier Inc. ermatofibrosarcoma protuberans (DFSP) is a and no frozen section was sent intraoperatively. The rare cutaneous malignancy with reported foreskin was not sent to pathology per institutional D annual incidence of 4.2 per million (0.3 to practice. 1.3 per million in pediatric patients) in the United Pathologic evaluation by a dermatopathologist revealed States. Patients are typically 20-50 years old. DFSP a CD34+ spindle cell neoplasm, favoring DFSP, with most commonly occurs on the trunk, and is very rarely involvement of deep and “lateral” margins (again, the found on the genitalia.1 To our knowledge, only four specimen was not orientated). FISH for the chromosomal cases of penile DFSP have been reported.2-4 The tumor translocation t(17,22) was negative. CT chest obtained is locally aggressive, with few reported cases of metas- for staging was negative for metastasis. After discussion at tasis.1 There is a paucity of data concerning character- multidisciplinary tumor board, options for management istics of disease and treatment strategies with only 2 proposed included Mohs surgery under local anesthesia by published guidelines available to guide management.5,6 dermatology versus wide local excision with frozen section We present a case of DFSP of the penis in an infant, under general anesthesia by urology. -
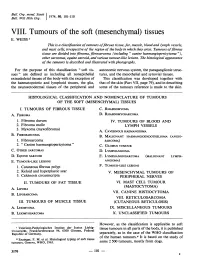
Mesenchymal) Tissues E
Bull. Org. mond. San 11974,) 50, 101-110 Bull. Wid Hith Org.j VIII. Tumours of the soft (mesenchymal) tissues E. WEISS 1 This is a classification oftumours offibrous tissue, fat, muscle, blood and lymph vessels, and mast cells, irrespective of the region of the body in which they arise. Tumours offibrous tissue are divided into fibroma, fibrosarcoma (including " canine haemangiopericytoma "), other sarcomas, equine sarcoid, and various tumour-like lesions. The histological appearance of the tamours is described and illustrated with photographs. For the purpose of this classification " soft tis- autonomic nervous system, the paraganglionic struc- sues" are defined as including all nonepithelial tures, and the mesothelial and synovial tissues. extraskeletal tissues of the body with the exception of This classification was developed together with the haematopoietic and lymphoid tissues, the glia, that of the skin (Part VII, page 79), and in describing the neuroectodermal tissues of the peripheral and some of the tumours reference is made to the skin. HISTOLOGICAL CLASSIFICATION AND NOMENCLATURE OF TUMOURS OF THE SOFT (MESENCHYMAL) TISSUES I. TUMOURS OF FIBROUS TISSUE C. RHABDOMYOMA A. FIBROMA D. RHABDOMYOSARCOMA 1. Fibroma durum IV. TUMOURS OF BLOOD AND 2. Fibroma molle LYMPH VESSELS 3. Myxoma (myxofibroma) A. CAVERNOUS HAEMANGIOMA B. FIBROSARCOMA B. MALIGNANT HAEMANGIOENDOTHELIOMA (ANGIO- 1. Fibrosarcoma SARCOMA) 2. " Canine haemangiopericytoma" C. GLOMUS TUMOUR C. OTHER SARCOMAS D. LYMPHANGIOMA D. EQUINE SARCOID E. LYMPHANGIOSARCOMA (MALIGNANT LYMPH- E. TUMOUR-LIKE LESIONS ANGIOMA) 1. Cutaneous fibrous polyp F. TUMOUR-LIKE LESIONS 2. Keloid and hyperplastic scar V. MESENCHYMAL TUMOURS OF 3. Calcinosis circumscripta PERIPHERAL NERVES II. TUMOURS OF FAT TISSUE VI. -

Mast-Cell Tumors
Glendale Animal Hospital 623-934-7243 familyvet.com Mast-Cell Tumors Basics OVERVIEW • Cancerous (known as “malignant”) round cell tumor; round cell tumors are made up of cells that appear round or oval on microscopic examination; mast-cell tumors are one type of round cell tumor • Tumor arising from mast cells • “Cutaneous” refers to the skin • Mast cells are connective tissue cells that contain very dark granules; the granules contain various chemicals, including histamine; they are involved in immune reactions and inflammation; mast cells can be found in various tissues throughout the body • Mast-cell tumors in dogs are graded as well differentiated or low grade (Grade 1), intermediately differentiated (Grade 2), and poorly differentiated, undifferentiated or high grade (Grade 3); in general, the more differentiated the mast-cell tumor, the better the prognosis • Differentiation is a determination of how much a particular tumor cell looks like a normal cell; the more differentiated, the more like the normal cell • Mast-cell tumors of the skin in cats are classified as “compact” (more benign behavior) or “diffuse” (more undifferentiated and aggressive) • Mast-cell tumors are the most common cancerous (malignant) skin tumor in the dog • Mast-cell tumors also may be found in the tissue immediately beneath the skin (that is, the subcutis), spleen, liver, and intestines • Mast-cell tumors are the most common tumor found in the spleen of cats • Mast-cell tumors can release histamine, leading to the development of hives, reddening of the -

Dermatopathology
76A ANNUAL MEETING ABSTRACTS of the nodules aspirated was 1.8 (NNAN), 3.2 (HA), 3.0 (HCa) and 2.9 (PTC). The average numbers of nodules identified by US were 3.3 in NNAN, 2.0 in HA, 1.7 in HCa, Dermatopathology and 1.8 in PTC (p<0.05). Furthermore, 40% (4 of 10) and 20% (2 of 10) of HCa were vascularized and microcalcified on US, respectively; and 50% (7 of 14) of NNAN had 337 CD10 and Ep-CAM Expression in Basal Cell Carcinoma, Classical multiple (5) small nodules in the background thyroid. FNA Findings – the Hurthle cell Trichoepithelioma, and Desmoplastic Trichoepithelioma tumors had more cellular smears, discohesive Hurthle cells, few, if any, lymphocytes, TE Abbott, MD Cole, JW Patterson, MR Wick. University of Virginia Health System, and scarce or absent colloid in comparison to the smears from NNAN. Charlottesville, VA. Conclusions: Dominant thyroid nodules 2 cm or less on US without evidence of Background: The distinction between basal cell carcinoma (BCC) and increased vascularity or microcalcifications in combination with the background trichoepithelioma (TE) has historically been made on the basis of specific histologic thyroid containing multiple (3 or more) smaller nodules and the FNA smears containing criteria, but it may be difficult when the tumor sample is limited. Recent reports have some lymphoid aggregates with Hurthle cells in moderately sized sheets are likely to suggested a utility for CD10 and Ep-CAM immunostaining in recognizing BCC. be benign. Communication between clinician and pathologist correlating US and FNA Accordingly, this study was initiated in order to determine whether those markers findings in difficult cases may avoid unnecessary surgery. -

Serum Alpha-Fetoprotein Values in Dogs with Various Hepatic Diseases
Serum alpha-fetoprotein Values in Dogs with Various Hepatic Diseases Takatsugu YAMADA,1,2), Megumi FUJITA1), Satoshi KITAO3), Yoshinori ASHIDA1), Kazuya NISHIZONO1), Ryo TSUCHIYA1), Takuo SHIDA4), and Kousaku KOBAYASHI1) 1)Laboratory of Veterinary Internal Medicine and 4)Laboratory of Veterinary Radiology, School of Veterinary Medicine; 2)Research Institute of Bioscience, Azabu University, 1–17–71 Fuchinobe, Sagamihara, Kanagawa, 229–8501 and 3)Doubutsu Medical Center, 1–6–45 Nakahozumi, Ibaraki-shi, Osaka 567–0034, Japan (Received 2 December 1997/Accepted 10 February 1999) ABSTRACT. Serum alpha-fetoprotein (AFP) values were measured in hepatic diseased dogs with or without tumor and non-hepatic tumor bearing dogs by a sandwich ELISA using anti-dog AFP antiserum. Serum AFP values were less than 70 ng/ml in clinically healthy dogs. The values in dogs with hepatocellular carcinoma were higher than 1,400 ng/ml in 7 of 9 dogs, wherever those in two dogs with cholangiocarcinoma were in the normal range. Serum AFP values in hepatic diseased dogs without tumor were also high, however, the values were below 500 ng/ml in 90% of the dogs. In non-hepatic tumor dogs, serum AFP values were less than 500 ng/ml in 76% of the dogs. In the surgically removal cases with hepatocellular carcinoma, serum AFP values rapidly decreased. These results suggested that the sandwich ELISA using anti-dog AFP antiserum was an available method for diagnosis of hepatocellular carcinoma in dogs.—KEY WORDS: alpha-fetoprotein, canine, ELISA, tumor. J. Vet. Med. Sci. 61(6): 657–659, 1999 Serum alpha-fetoprotein (AFP) values have been used with hepatocellular carcinoma were also monitored AFP for the diagnosis of hepatocellular carcinoma [4, 5–6, 14] values after surgical removal of masses. -

Dermoscopic Features of Skin Lesions in Patients with Mastocytosis
STUDY Dermoscopic Features of Skin Lesions in Patients With Mastocytosis Sergio Vano-Galvan, MD, PhD; Iva´n A´ lvarez-Twose, MD; Elena De las Heras, MD, PhD; J. M. Morgado, Msc; Almudena Matito, MD; Laura Sa´nchez-Mun˜oz, MD, PhD; Maria N. Plana, MD, PhD; Pedro Jae´n, MD, PhD; Alberto Orfao, MD, PhD; Luis Escribano, MD, PhD Objectives: To evaluate dermoscopic features in a group factors for more symptomatic forms of the disease ac- of 127 patients with mastocytosis in the skin and to in- cording to the need for daily antimediator therapy. vestigate the relationship between different dermo- scopic patterns and other clinical and biological charac- Results: Four distinct dermoscopic patterns were ob- teristics of the disease. served: yellow-orange blot, pigment network, reticular vascular pattern, and (most frequently) light-brown blot. Design: Clinical and laboratory data were compared A reticular vascular pattern was identified in all telangi- among patients with mastocytosis grouped according to ectasia macular eruptiva and some maculopapular mas- the different dermoscopic patterns. tocytosis. In turn, all patients with mastocytoma dis- played the yellow-orange blot pattern. The reticular Setting: Patients were selected from the Instituto de Es- vascular dermoscopic pattern was associated with the need tudios de Mastocitosis de Castilla La Mancha and the De- for daily antimediator therapy; this pattern, together with partment of Dermatology of Hospital Universitario Ramo´n serum tryptase levels and plaque-type mastocytosis, rep- y Cajal from April 1 through September 30, 2009. resented the best combination of independent factors to predict the need for maintained antimediator therapy. -

PROMIS Itch Questionnaire – Children Symptom (PIQ-C-Symptom) Letter of Intent
Clinical Outcome Assessments (COA) Qualification Program DDT COA #000140: PROMIS Itch Questionnaire – Children Symptom (PIQ-C-Symptom) Letter of Intent Section 1. Administrative Structure This project has been led by Amy Paller, MD (PI of sub-study that developed the PIQ-C and co-PI of the PEPR project at Northwestern University) from the Dermatology and Pediatrics departments at Northwestern University (676 N. St. Clair, Suite 1600, Chicago, IL 60611) and Jin-Shei Lai, Ph.D. (contact co-PI of the PEPR project at Northwestern University) from the Medical Social Sciences and Pediatrics departments at Northwestern University (625 N. Michigan Avenue, 21st floor, Chicago, IL 60611). Dr. Paller has had 35 years of experience in caring for children with disorders causing itch. She is Chair of the Dept. of Dermatology, directs the Skin Disease Research Center at Northwestern (now Skin Biology and Diseases Resource-based Center) as well as the Pediatric Dermatology Clinical Research Unit, and has been the PI of more than 100 clinical trials in children with disorders associated with pruritus (atopic dermatitis, epidermolysis bullosa, ichthyosis, psoriasis), most of which involve measuring itch and quality of life. She has authored more than 250 peer-reviewed papers related to these disorders. She has been working on developing and validating PRO tools during the past 5 years, including through this project. Dr. Lai has significant experience in patient reported outcomes, including burden of disease and treatment impact studies across a range of pediatric and adult conditions. She has served as a principal investigator and co-investigator on several federal and foundation funded projects and is the lead developer of several pediatric and adult quality of life and symptom measurement instruments, including the PROMIS Fatigue and Cognition item banks for both adults and children, pediatric Neuro-QoL measurement system, and the pediatric Functional Assessment of Chronic Illness Therapy (pedsFACIT). -

Urticaria Pigmentosa: a Case Report and Review of Current Standards in the Diagnosis of Systemic Mastocytosis
Urticaria Pigmentosa: A Case Report and Review of Current Standards in the Diagnosis of Systemic Mastocytosis Riddhi J. Shah, DO,* Mark A. Kuriata, DO, FAOCD** *Dermatology Resident, 2nd year, MSUCOM/Lakeland Regional Medical Center, St. Joseph, MI **Dermatology Residency Program Director, MSUCOM/Lakeland Regional Medical Center, St. Joseph, MI Abstract Mastocytosis is a group of diseases that is characterized by mast-cell infiltration of the skin. The cutaneous forms of the disease are most identifiable, yet it is important to recognize the progression to systemic disease due to the eaffect on morbidity and mortality. We Our goal is to describe a case of cutaneous mastocytosis as well as review the current standards in diagnosis and management of systemic mastocytosis. Introduction patient had several bouts of loose stools. This and spleen did not reveal any organomegaly. Mast-cell disease is a rare disorder, primarily was accompanied by bloating and indigestion, Muscle strength and tone appeared to be within of childhood, that is usually self-resolving. which occurred 30 minutes after a meal. A normal limits. There were no palpable lymph Approximately two-thirds of cases are limited to colonoscopy was performed one year prior at an nodes in the neck, axillae or groin regions. outside facility, and it was within normal limits. the skin. The most common forms of cutaneous Our differential diagnosis included systemic However, no biopsies were performed to look mastocytosis include: mastocytoma, urticaria mastocytosis as well as carcinoid syndrome, for mast-cell infiltration of the digestive tract. pigmentosa, telangiectasia macularis eruptiva pheochromocytoma, inflammatory bowel disease, Our patient also had sharp, intermittent, left perstans, maculopapular cutaneous mastocytosis, urticaria, and myeloproliferative disorder. -

The a Subunit of GTP-Binding Protein G0 in Neuroblastoma: Correlation with Advanced Disease Stage
[CANCER RESEARCH 54, 2334-2336, May 1, 19941 The a Subunit of GTP-binding Protein G0 in Neuroblastoma: Correlation with Advanced Disease Stage Yukio Ishiguro,' Kanefusa Kato, Tomiko Asano, Hiroshi Akatsuka, Hiroyuki Iwata, Fujio Ito, and Takahiro Ito Department ofSurgery, Branch Hospital ofNagoya University School ofMedicine, Daiko-minam4 Higashi-ku, Nagoya 461 [V. L, H. A., H. L, F. I., T. I.J, and Department of Biochemistry, Institute for Developmental Research, Aichi Prefectural Colony, Kamiya-cyo, Kasugai [K K, T. A.J, Japan ABSTRACT chemotherapy with cyclophosphamide and vincristine for 3 to 12 months. Stage III patients without recurrences (n = 5) had postoperative chemotherapy Tissue levels of the a subunit of G protein G0 (G0 a) were measured in for 2 years. Nine of 24 patients with distant metastases or recurrences had bone solid tumors from pediatric patients by immunoassay.G0 a concentra marrow transplants after complete clinical remissions. Survival time was tions were determined in the supernatant obtained by centrifugatlon of measured from the start of treatment. Diagnoses were confirmed histologically. tissue homogenates prepared in the presence (total G0 a) or absence of 2% Preparation of Tissue Extracts. Tissues were homogenized at 0°Cin 10 sodium cholate (soluble G0 a). Mean G0 a concentrations (total G0 a and volumes of 10 mM Tris-HCI (pH 7.5) containing 1 mM EDTA, using a soluble G0 a) in neuroblastomas (7 ganglioneuromas,13 ganglioneuro Polytron-type homogenizer. One-half of each homogenate was centrifuged at blastomas, and 50 neuroblastomas) were over 50-fold higher than those in 4°Cat 125,000 X g for 40 mm, and the supernatant was saved for G0 a other solidtumors from pediatric patients (n 13).Mean total G0a and analysis of the soluble fraction (soluble G0 a). -

Mast Cell Sarcoma: a Rare and Potentially Under
Modern Pathology (2013) 26, 533–543 & 2013 USCAP, Inc. All rights reserved 0893-3952/13 $32.00 533 Mast cell sarcoma: a rare and potentially under-recognized diagnostic entity with specific therapeutic implications Russell JH Ryan1, Cem Akin2,3, Mariana Castells2,3, Marcia Wills4, Martin K Selig1, G Petur Nielsen1, Judith A Ferry1 and Jason L Hornick2,5 1Pathology Service, Massachusetts General Hospital, and Harvard Medical School, Boston, MA, USA; 2Mastocytosis Center, Harvard Medical School, Boston, MA, USA; 3Department of Medicine, Harvard Medical School, Boston, MA, USA; 4Seacoast Pathology / Aurora Diagnostics, Exeter, NH and 5Department of Pathology, Brigham and Women’s Hospital, and Harvard Medical School, Boston, MA, USA Mast cell sarcoma is a rare, aggressive neoplasm composed of cytologically malignant mast cells presenting as a solitary mass. Previous descriptions of mast cell sarcoma have been limited to single case reports, and the pathologic features of this entity are not well known. Here, we report three new cases of mast cell sarcoma and review previously reported cases. Mast cell sarcoma has a characteristic morphology of medium-sized to large epithelioid cells, including bizarre multinucleated cells, and does not closely resemble either normal mast cells or the spindle cells of systemic mastocytosis. One of our three cases arose in a patient with a remote history of infantile cutaneous mastocytosis, an association also noted in one previous case report. None of our three cases were correctly diagnosed as mast cell neoplasms on initial pathological evaluation, suggesting that this entity may be under-recognized. Molecular testing of mast cell sarcoma has not thus far detected the imatinib- resistant KIT D816V mutation, suggesting that recognition of these cases may facilitate specific targeted therapy.