Nursing in the Digital Age Using Technology to Support Patients in the Home
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
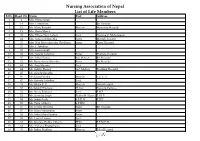
Nursing Association of Nepal List of Life Members S.No
Nursing Association of Nepal List of Life Members S.No. Regd. No. Name Post Address 1 2 Mrs. Prema Singh 2 14 Mrs. I. Mathema Bir Hospital 3 15 Ms. Manu Bangdel Matron Maternity Hospital 4 19 Mrs. Geeta Murch 5 20 Mrs. Dhana Nani Lohani Lect. Nursing C. Maharajgunj 6 24 Mrs. Saraswati Shrestha Sister Mental Hospital 7 25 Mrs. Nati Maya Shrestha (Pradhan) Sister Kanti Hospital 8 26 Mrs. I. Tuladhar 9 32 Mrs. Laxmi Singh 10 33 Mrs. Sarada Tuladhar Sister Pokhara Hospital 11 37 Mrs. Mita Thakur Ad. Matron Bir Hospital 12 42 Ms. Rameshwori Shrestha Sister Bir Hospital 13 43 Ms. Anju Sharma Lect. 14 44 Ms. Sabitry Basnet Ast. Matron Teaching Hospital 15 45 Ms. Sarada Shrestha 16 46 Ms. Geeta Pandey Matron T.U.T. H 17 47 Ms. Kamala Tuladhar Lect. 18 49 Ms. Bijaya K. C. Matron Teku Hospital 19 50 Ms.Sabitry Bhattarai D. Inst Nursing Campus 20 52 Ms. Neeta Pokharel Lect. F.H.P. 21 53 Ms. Sarmista Singh Publin H. Nurse F. H. P. 22 54 Ms. Sabitri Joshi S.P.H.N F.H.P. 23 55 Ms. Tuka Chhetry S.P.HN 24 56 Ms. Urmila Shrestha Sister Bir Hospital 25 57 Ms. Maya Manandhar Sister 26 58 Ms. Indra Maya Pandey Sister 27 62 Ms. Laxmi Thakur Lect. 28 63 Ms. Krishna Prabha Chhetri PHN F.P.M.C.H. 29 64 Ms. Archana Bhattacharya Lect. 30 65 Ms. Indira Pradhan Matron Teku Hospital S.No. Regd. No. Name Post Address 31 67 Ms. -

Lawrlwytho'r Atodiad Gwreiddiol
Operational services structure April 2021 14/04/2021 Operational Leadership Structures Director of Operations Director of Nursing & Quality Medical Director Lee McMenamy Joanne Hiley Dr Tessa Myatt Medical Operations Operations Clinical Director of Operations Deputy Director of Nursing & Deputy Medical Director Hazel Hendriksen Governance Dr Jose Mathew Assistant Clinical Director Assistant Director of Assistant Clinical DWiraerctringor ton & Halton Operations Corporate Corporate Lorna Pink Assistant Assistant Director Julie Chadwick Vacant Clinical Director of Nursing, AHP & Associate Clinical Director Governance & Professional Warrington & Halton Compliance Standards Assistant Director of Operations Assistant Clinical Director Dr Aravind Komuravelli Halton & Warrington Knowsley Lee Bloomfield Claire Hammill Clare Dooley Berni Fay-Dunkley Assistant Director of Operations Knowsley Associate Medical Director Nicky Over Assistant Clinical Director Allied Health Knowsley Assistant Director of Sefton Professional Dr Ashish Kumar AssiOstapenrta Dtiironesc tKnor oofw Oslpeeyr ations Sara Harrison Lead Nicola Over Sefton James Hester Anne Tattersall Assistant Clinical Director Associate Clinical Director Assistant Director of St Helens & Knowsley Inpatients St Helens Operations Sefton Debbie Tubey Dr Raj Madgula AssistanAt nDniree Tcatttore ofrs aOllp erations Head of St Helens & Knowsley Inpatients Safeguarding Tim McPhee Assistant Clinical Director Sarah Shaw Assistant Director of Associate Medical Director Operations St Helens Mental Health -

The District Nursing and Community Matron Services Workforce: a Scoping Review in South London for the South London Nursing Network
The district nursing and community matron services workforce: A scoping review in South London for the South London Nursing Network Vari Drennan, Professor of Health Care & Policy Research March 2014 Acknowledgements The time and input from senior nurses in provider and commissioning organisations across London is acknowledged with gratitude. This scoping review was commissioned by the South London Nursing Network and funded by the South London Academic Health Science System. Disclaimer The views and opinions expressed within the document are those of the author and not of the funding or commissioning organisations. Author contact details Vari Drennan, Professor of Health Care & Policy Research. Faculty of Health, Social Care & Education, Kingston University & St. George’s University of London, Cranmer Terrace , London SW170RE [email protected] Page 2 of 30 Executive summary This report presents both an overview of the issues influencing district nursing and community matron workforces and also a scoping of key issues in respect of workforce development in district nursing and community matron services in South London to inform the work of the South London Nursing Network. Over view of the issues influencing the district nursing and community nursing workforces The strategic policy direction relevant to the district nursing and community matron services attend is that for patient populations with long term conditions and their family carers. The policy expectations are for increased activity in support of public health and compassionate care and treatment outcomes that include health promotion (for example increased physical activity and smoking cessation), adult vaccination programmes, support for self-management, reducing premature mortality, increasing quality of life, improving rehabilitation following inpatient stays, greater integration with other health and social are services and improvement to end of life care. -

The District Nurse in Our Society Nursing Times
The District Nurse in our Society Anthony J. Carr, SRN, NON Cert., QN, MRSH, AIHE Midland Area Organizer, Rcn Trained nurse, health educator, friend he suggests, is not readily recognized of the family-this is how the author by the public-or by her own colleagues sees the district nurse, but her position, in hospital It may seem unnecessary to many nurses to nurse patients in their the public, and in the nursing pro- district nurses to be reminded of the own homes. I do not, intend to fession .as to the training and ex- position they hold in their own com- survey the development of' district perience of the district nurse. munity. .On reflection, however, I nursing in this country-its beginnings While the Minister of Health is think they will agree that it is profitable in Liverpool with the Rathbone launching a national campaign for for all professional nurses to pause family, and the connections of Florence recruiting student and pupil .nurses every so often and make a reassess- Nightingale with the first projects of and projecting a true image of nursing, ment of their personal contribution, district nursing. What I would men- perhaps the local authorities may be away from' the 'pressure of daily work. tion is the fact that a district nurse is a persuaded to' correct the image of the The main purpose of this article, State-registered nurse, holding in most district nurse with their own local which is divided under six simple cases the National District Nursing publicity. headings, is that everyone should Certificate and/or on the roll of the' I personally have 'lost count of reassess her own position in the city, Queen's Institute of District Nursing. -

THE DEVELOPMENT of NURSING EDUCATION in the ENGLISH-SPEAKING CARIBBEAN ISLANDS by PEARL I
THE DEVELOPMENT OF NURSING EDUCATION IN THE ENGLISH-SPEAKING CARIBBEAN ISLANDS by PEARL I. GARDNER, B.S.N., M.S.N., M.Ed. A DISSERTATION IN HIGHER EDUCATION Submitted to the Graduate Faculty of Texas Tech University in Partial Fulfillment of the Requirements for the Degree of DOCTOR OF EDUCATION Approved Accepted Dean of the Graduate School August, 1993 ft 6 l^yrr^7^7 801 J ,... /;. -^o ACKNOWLEDGEMENTS C?^ /c-j/^/ C^ ;^o.^^ I would like to thank Dr. Clyde Kelsey, Jr., for his C'lp '^ ^unflagging support, his advice and his constant vigil and encouragement in the writing of this dissertation. I would also like to thank Dr. Patricia Yoder-Wise who acted as co-chairperson of my committee. Her advice was invaluable. Drs. Mezack, Willingham, and Ewalt deserve much praise for the many times they critically read the manuscript and gave their input. I would also like to thank Ms. Janey Parris, Senior Program Officer of Health, Guyana, the government officials of the Caribbean Embassies, representatives from the Caribbean Nursing Organizations, educators from the various nursing schools and librarians from the archival institutions and libraries in Trinidad and Tobago and Jamaica. These individuals agreed to face-to-face interviews, answered telephone questions and mailed or faxed information on a regular basis. Much thanks goes to Victor Williams for his computer assistance and to Hannelore Nave for her patience in typing the many versions of this manuscript. On a personal level I would like to thank my niece Eloise Walters for researching information in the nursing libraries in London, England and my husband Clifford for his belief that I could accomplish this task. -

Design and Implementation of Health Information Systems
Design and implementation of health information systems Edited by Theo Lippeveld Director of Health Information Systems, John Snow Inc., Boston, MA, USA Rainer Sauerborn Director of the Department of Tropical Hygiene and Public Health, University of Heidelberg, Germany Claude Bodart Project Director, German Development Cooperation, Manila, Philippines World Health Organization Geneva 2000 WHO Library Cataloguing in Publication Data Design and implementation of health information systems I edited by Theo Lippeveld, Rainer Sauerborn, Claude Bodart. 1.1nformation systems-organization and administration 2.Data collection-methods I.Lippeveld, Theo II.Sauerborn, Rainer III.Bodart, Claude ISBN 92 4 1561998 (NLM classification: WA 62.5) The World Health Organization welcomes requests for permission to reproduce or translate its pub lications, in part or in full. Applications and enquiries should be addressed to the Office of Publi cations, World Health Organization, Geneva, Switzerland, which will be glad to provide the latest information on any changes made to the text, plans for new editions, and reprints and translations already available. © World Health Organization 2000 Publications of the World Health Organization enjoy copyright protection in accordance with the provisions of Protocol 2 of the Universal Copyright Convention. All rights reserved. The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the Secretariat of the World Health Or ganization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. The mention of specific companies or of certain manufacturers' products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. -

Brush School District Re 2J District Wide School Nurse Job Description Reports To: Superintendent Terms of Employment: 169 Day W
Brush School District Re 2J District Wide School Nurse Job Description Reports to: Superintendent Terms of employment: 169 day work year, certified salary schedule Position Summary: The purpose of the district school nurse position is to ensure that the health needs during the school day of all students in the Brush school district are addressed. The district nurse will supervise and collaborate with the Thomson licensed practical nurse. The district school nurse will oversee school health services at the district level. Principle Responsibilities: The district school nurse will: 1. Provide nursing care for the health needs of students including emergencies 2. Develop and implement health care plans 3. Participate in the identification process of children with special needs 4. Maintain student health records 5. Direct the immunization program 6. Direct the vision and hearing screening program 7. Manage communicable disease outbreaks 8. Serve as a case manager for at-risk children 9. Serve as a liaison between and resource for teachers, administrators, parents, and community health care providers 10. Conduct health assessments 11. Delegate to, train, and supervise unlicensed assistive personnel 12. Serve as the Child Care Health Consultant for the preschool and Head Start 13. Oversee school health services at the district level 14. Supervise the licensed practical nurse at Thomson POSITION REQUIREMENTS Minimum Education: Bachelor’s degree in school nursing preferred Current license to practice as a registered nurse in Colorado, Current national certification in school nursing Current certification in CPR/AED and first aid Minimum Experience: Three years of experience in school nursing preferably in pediatrics in a hospital or clinical setting At least three years as an RN, preferably in pediatrics in a hospital or clinical setting Experience in outpatient settings with long term planning would beneficial. -

Principles and Elements of School Nurse Management of Students with Diabetes
Principles and Elements of School Nurse Management of Students with Diabetes Introduction It is the position of the Oregon School Nurses Association (OSNA) that all students are entitled to safe and effective management of their special health care needs by a Registered Nurse while at school.1 Increasing incidence of diabetes types 1 and 2 in youth,2 the associated advancing technological and medical management, and the requirements for schools to provide the necessary health care obligate the school nurse to be competent in providing evidence-based nursing care. To support the delivery of evidence-based, standardized nursing care the OSNA summarizes in this document the essential components of school nursing management for students with diabetes. By practice standards all nurses are accountable for maintaining current competency about the medical condition and evidence-based treatment measures. This document is intended to provide a best-practice frame work for Oregon’s school nurse services for students with diabetes. The document is not meant to provide a comprehensive medical and nursing curriculum on pediatric diabetes. The Association acknowledges the many excellent reference resources available on diabetes management and encourages readers to pursue review when desiring more in-depth information and practice tools. Roles of the School Nurse in Managing Students with Diabetes “It is the position of the National Association of School Nurses (NASN),” and therefore the OSNA, “that the school nurse is the only school staff member who has the skills, knowledge base, and statutory authority to fully meet the healthcare needs of students with diabetes in the school setting.”3 School nurse roles include, but are not limited to: • Development and implementation of individual health management plans (IHP), including the associated interventions such as delegation. -

Evaluation of Hospital Information System in the Northern Province in South Africa
EVALUATION OF HOSPITAL INFORMATION SYSTEM IN THE NORTHERN PROVINCE IN SOUTH AFRICA “ Using Outcome Measures” Report prepared for the HEALTH SYSTEMS TRUST By Nolwazi Mbananga Rhulani Madale Piet Becker THE MEDICAL RESEARCH COUNCIL OF SOUTH AFRICA PRETORIA May 2002 1 ACKNOWLEDGEMENTS The Department of Health and Welfare in the Northern Province is acknowledged for its mandate to conduct this study and its support of the project throughout. The project Team is recognised for its great efforts in developing the project proposal and obtaining the necessary funding to conduct the study, without which it would not have been possible. The project team members; Dr Jeremy Wyatt, Dr LittleJohns, Dr Herbst, Dr Zwarenstein, Dr Power, Dr Rawlinson, Dr De Swart, Dr P Becker, Ms Madale and others played a key role in maintaining the scientific rigour for the study and their dedication is appreciated. The MEDUNSA Community Health in the Northern Province is credited for the direction and support it provided during the early stages of project development, planning and implementation. It is important to explain that Ms Mbananga conducted the qualitative component of the study as a Principal investigator while she and Dr Becker were called upon to take over the quantitative component of the study and joined at the stage of post implementation data collection. The financial support that was provided by the Health Systems Trust and the Medical Research Council is highly valued this project could not have been started and successfully completed without it. We cannot forget our secretaries: Emily Gomes and Alta Hansen who assisted us in transcribing data. -

The Matron's Handbook
The matron’s handbook For aspiring and experienced matrons Updated July 2021 Contents Foreword........................................................................................ 2 Introduction .................................................................................... 4 The matron’s key roles................................................................... 6 1. Inclusive leadership, professional standards and accountability 8 2. Governance, patient safety and quality .................................... 12 3. Workforce planning and resource management ...................... 17 4. Patient experience and reducing health inequalities ................ 22 5. Performance and operational oversight ................................... 24 6. Digital and information technology ........................................... 27 7. Education, training and development ....................................... 33 8. Research and development ..................................................... 36 9. Collaborative working and clinical effectiveness ...................... 37 10. Service improvement and transformation .............................. 40 Appendix: The matron’s developmental framework and competencies............................................................................... 43 Acknowledgements ...................................................................... 51 1 | Contents Foreword Matrons are vital to delivering high quality care to patients and their relatives across the NHS and the wider health and care sector. They -

Divisional Structure - University Hospital Southampton NHS Foundation Trust – As at 1 July 2021
Divisional structure - University Hospital Southampton NHS Foundation Trust – as at 1 July 2021 Chief operating officer Joe Teape Division A Division B Division C Division D DCD – Andrew Webb DCD – Trevor Smith DCD – Freya Pearson DCD – David Higgs DDO – Greg Chapple DDO – Gavin Hawkins DDO – Martin De Sousa DHN/P – Rachel Davies DHN/P – Sarah Herbert DDO – Jacqui McAfee DHN/P – Louisa Green DHN/P – Natasha Watts Acuity Matron – Karen Hill DR&DL – Fraser Cummings DoM – Suzanne Cunningham DR&DL – Boyd Ghosh DR&DL – Bhaskar Somani DFM – John Light DR&DL – Luise Marino DFM – Alex Mawers (Interim) DS&BDM – Alison Gray DFM – Wayne Rogers DFM – Emma Hawkins DS&BDM – Adam Wells HRBP – Emma Watts DS&BDM – Dan Jeffery DS&BDM – Victoria Kearney HRBP – Rachel Dore HRBP – Rachel Dore (covering until replacement) Care groups HRBP – Katie Dunman (nee Molloy) Care groups Cancer care: Care groups Care groups Surgery: CGCL – Tim Iveson Women and newborn: Cardiovascular and thoracic: CGCL – John Knight CGM – Collette Byelong CGCL – Sarah Walker CGCL – Edwin Woo CGM – Justin Sanders (from 5/7/21) A/CGM – awaiting appointment CGM – Fiona Lawson CGM – Fiona Liddell A/CGM – Jon Watson Matron – Jenny Milner IP & Theatres Matron – Carol Gosling ACGM – Juliet Thomas A/CGM – Erin Flahavan Matron – Steph Churchill OP Matron – Karen Elkins Matron – Jenny Dove Neonatal Matron – Andrea Robson (interim) Matron – Kerry Rayner Matron – Julia Tonks Matron – Georgina Kirk Angie Ansell (from 12/7/21) Emergency medicine: Matron - Jean-Paul Evangelista Matron – Jo Rigby CGCL -

The Archive of the Queen's Nursing Institute in the Contemporary Medical Archives Centre
Medical History, 2000, 45: 251-266 Illustrations from the Wellcome Library The Archive of the Queen's Nursing Institute in the Contemporary Medical Archives Centre SHIRLEY DIXON* The Contemporary Medical Archives Centre (CMAC) at the Wellcome Library has always endeavoured to draw attention to the importance of archives and to publicize their existence and availability, often by surveying and listing the records of medical bodies in situ. One of the hoards of records to come to the attention of the CMAC in its early days was that held by the Queen's Nursing Institute- QNI (formerly Queen Victoria's Jubilee Institute for Nurses, and from 1928 the Queen's Institute of District Nursing), and in 1982 one of the archivists visited QNI headquarters at Lower Belgrave Street to record the types and covering dates of the material. She found such a rich accumulation of records that, on the.failure of a proposal that the QNI employ someone to sort and catalogue them fully, the CMAC undertook to survey and briefly list them. It was a typical survey of an old-established body, in that the archivist had to hunt high and low through the building, delving into cupboards, filing cabinets and drawers to locate material which had been kept for many years, but it was atypical from the point of view of the long history of the bodies which had generated the material, and the detail and richness of the records. The Institute had organized district nursing and district nurse training for the British Isles from its foundation in 1889, and even after the introduction of the National Health Service it had played a role as agent for many local authorities.