A Systematic Review of the Use of Opioid Medication for Those With
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Opioid-Induced Hyperalgesia in Humans Molecular Mechanisms and Clinical Considerations
SPECIAL TOPIC SERIES Opioid-induced Hyperalgesia in Humans Molecular Mechanisms and Clinical Considerations Larry F. Chu, MD, MS (BCHM), MS (Epidemiology),* Martin S. Angst, MD,* and David Clark, MD, PhD*w treatment of acute and cancer-related pain. However, Abstract: Opioid-induced hyperalgesia (OIH) is most broadly recent evidence suggests that opioid medications may also defined as a state of nociceptive sensitization caused by exposure be useful for the treatment of chronic noncancer pain, at to opioids. The state is characterized by a paradoxical response least in the short term.3–14 whereby a patient receiving opioids for the treatment of pain Perhaps because of this new evidence, opioid may actually become more sensitive to certain painful stimuli. medications have been increasingly prescribed by primary The type of pain experienced may or may not be different from care physicians and other patient care providers for the original underlying painful condition. Although the precise chronic painful conditions.15,16 Indeed, opioids are molecular mechanism is not yet understood, it is generally among the most common medications prescribed by thought to result from neuroplastic changes in the peripheral physicians in the United States17 and accounted for 235 and central nervous systems that lead to sensitization of million prescriptions in the year 2004.18 pronociceptive pathways. OIH seems to be a distinct, definable, One of the principal factors that differentiate the use and characteristic phenomenon that may explain loss of opioid of opioids for the treatment of pain concerns the duration efficacy in some cases. Clinicians should suspect expression of of intended use. -

Opioid Tolerance in Methadone Maintenance Treatment: Comparison
Gutwinski et al. Harm Reduction Journal (2016) 13:7 DOI 10.1186/s12954-016-0095-0 RESEARCH Open Access Opioid tolerance in methadone maintenance treatment: comparison of methadone and levomethadone in long-term treatment Stefan Gutwinski*, Nikola Schoofs, Heiner Stuke, Thomas G. Riemer, Corinde E. Wiers and Felix Bermpohl Abstract Background: This study aimed to investigate the development of opioid tolerance in patients receiving long-term methadone maintenance treatment (MMT). Methods: A region-wide cross-sectional study was performed focusing on dosage and duration of treatment. Differences between racemic methadone and levomethadone were examined. All 20 psychiatric hospitals and all 110 outpatient clinics in Berlin licensed to offer MMT were approached in order to reach patients under MMT fulfilling the DSM IV criteria of opiate dependence. In the study, 720 patients treated with racemic methadone or levomethadone gave information on the dosage of treatment. Out of these, 679 patients indicated the duration of MMT. Results: Treatment with racemic methadone was reported for 370 patients (54.5 %), with levomethadone for 309 patients (45.5 %). Mean duration of MMT was 7.5 years. We found a significant correlation between dosage and duration of treatment, both in a conjoint analysis for the two substances racemic methadone and levomethadone and for each substance separately. These effects remained significant when only patients receiving MMT for 1 year or longer were considered, indicating proceeding tolerance development in long-term treatment. When correlations were compared between racemic methadone and levomethadone, no significant difference was found. Conclusions: Our data show a tolerance development under long-term treatment with both racemic methadone and levomethadone. -
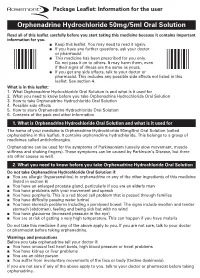
Orphenadrine Hydrochloride 50Mg/5Ml Oral Solution Rare (Affect More Than 1 in 10,000 People) N Forgetting Things More Than Usual
Uncommon (affect more than 1 in 1000 people) n Constipation Package Leaflet: Information for the user n Greater sensitivity to things around you or feeling nervous n Feeling light-headed and an unusual feeling of excitement (elation) n Difficulty sleeping or feeling tired. Orphenadrine Hydrochloride 50mg/5ml Oral Solution Rare (affect more than 1 in 10,000 people) n Forgetting things more than usual. Read all of this leaflet carefully before you start taking this medicine because it contains important information for you. Reporting of side effects n Keep this leaflet. You may need to read it again. If you get any side effects, talk to your doctor, n If you have any further questions, ask your doctor pharmacist or nurse. This includes any possible side or pharmacist. effects not listed in this leaflet. You can also report n This medicine has been prescribed for you only. side effects directly (see details below). By reporting Do not pass it on to others. It may harm them, even side effects you can help provide more information on if their signs of illness are the same as yours. the safety of this medicine. n If you get any side effects, talk to your doctor or United Kingdom pharmacist. This includes any possible side effects not listed in this Yellow Card Scheme leaflet. See section 4. Website: www.mhra.gov.uk/yellowcard or search for MHRA Yellow Card in the Google Play or What is in this leaflet: Apple App Store. 1. What Orphenadrine Hydrochloride Oral Solution is and what is it used for 2. -

Guidelines for the Forensic Analysis of Drugs Facilitating Sexual Assault and Other Criminal Acts
Vienna International Centre, PO Box 500, 1400 Vienna, Austria Tel.: (+43-1) 26060-0, Fax: (+43-1) 26060-5866, www.unodc.org Guidelines for the Forensic analysis of drugs facilitating sexual assault and other criminal acts United Nations publication Printed in Austria ST/NAR/45 *1186331*V.11-86331—December 2011 —300 Photo credits: UNODC Photo Library, iStock.com/Abel Mitja Varela Laboratory and Scientific Section UNITED NATIONS OFFICE ON DRUGS AND CRIME Vienna Guidelines for the forensic analysis of drugs facilitating sexual assault and other criminal acts UNITED NATIONS New York, 2011 ST/NAR/45 © United Nations, December 2011. All rights reserved. The designations employed and the presentation of material in this publication do not imply the expression of any opinion whatsoever on the part of the Secretariat of the United Nations concerning the legal status of any country, territory, city or area, or of its authorities, or concerning the delimitation of its frontiers or boundaries. This publication has not been formally edited. Publishing production: English, Publishing and Library Section, United Nations Office at Vienna. List of abbreviations . v Acknowledgements .......................................... vii 1. Introduction............................................. 1 1.1. Background ........................................ 1 1.2. Purpose and scope of the manual ...................... 2 2. Investigative and analytical challenges ....................... 5 3 Evidence collection ...................................... 9 3.1. Evidence collection kits .............................. 9 3.2. Sample transfer and storage........................... 10 3.3. Biological samples and sampling ...................... 11 3.4. Other samples ...................................... 12 4. Analytical considerations .................................. 13 4.1. Substances encountered in DFSA and other DFC cases .... 13 4.2. Procedures and analytical strategy...................... 14 4.3. Analytical methodology .............................. 15 4.4. -

Clinical and Pharmacokinetic Evaluation of S
Casoni et al. Acta Veterinaria Scandinavica (2015) 57:21 DOI 10.1186/s13028-015-0112-4 RESEARCH Open Access Clinical and pharmacokinetic evaluation of S-ketamine for intravenous general anaesthesia in horses undergoing field castration Daniela Casoni1*, Claudia Spadavecchia1, Beat Wampfler2, Wolfgang Thormann3 and Olivier L Levionnois1 Abstract Background: Intravenous anaesthetic drugs are the primary means for producing general anaesthesia in equine practice. The ideal drug for intravenous anaesthesia has high reliability and pharmacokinetic properties indicating short elimination and lack of accumulation when administered for prolonged periods. Induction of general anaesthesia with racemic ketamine preceded by profound sedation has already an established place in the equine field anaesthesia. Due to potential advantages over racemic ketamine, S-ketamine has been employed in horses to induce general anaesthesia, but its optimal dose remains under investigation. The objective of this study was to evaluate whether 2.5 mg/kg S-ketamine could be used as a single intravenous bolus to provide short-term surgical anaesthesia in colts undergoing surgical castration, and to report its pharmacokinetic profile. Results: After premedication with romifidine and L-methadone, the combination of S-ketamine and diazepam allowed reaching surgical anaesthesia in the 28 colts. Induction of anaesthesia as well as recovery were good to excellent in the majority (n = 22 and 24, respectively) of the colts. Seven horses required additional administration of S-ketamine to prolong the duration of surgical anaesthesia. Redosing did not compromise recovery quality. Plasma concentration of S-ketamine decreased rapidly after administration, following a two-compartmental model, leading to the hypothesis of a consistent unchanged elimination of the parent compound into the urine beside its conversion to S-norketamine. -

Risk Based Requirements for Medicines Handling
Risk based requirements for medicines handling Including requirements for Schedule 4 Restricted medicines Contents 1. Introduction 2 2. Summary of roles and responsibilities 3 3. Schedule 4 Restricted medicines 4 4. Medicines acquisition 4 5. Storage of medicines, including control of access to storage 4 5.1. Staff access to medicines storage areas 5 5.2. Storage of S4R medicines 5 5.3. Storage of S4R medicines for medical emergencies 6 5.4. Access to storage for S4R and S8 medicines 6 5.5. Pharmacy Department access, including after hours 7 5.6. After-hours access to S8 medicines in the Pharmacy Department 7 5.7. Storage of nitrous oxide 8 5.8. Management of patients’ own medicines 8 6. Distribution of medicines 9 6.1. Distribution outside Pharmacy Department operating hours 10 6.2. Distribution of S4R and S8 medicines 10 7. Administration of medicines to patients 11 7.1. Self-administration of scheduled medicines by patients 11 7.2. Administration of S8 medicines 11 8. Supply of medicines to patients 12 8.1. Supply of scheduled medicines to patients by health professionals other than pharmacists 12 9. Record keeping 13 9.1. General record keeping requirements for S4R medicines 13 9.2. Management of the distribution and archiving of S8 registers 14 9.3. Inventories of S4R medicines 14 9.4. Inventories of S8 medicines 15 10. Destruction and discards of S4R and S8 medicines 15 11. Management of oral liquid S4R and S8 medicines 16 12. Cannabis based products 17 13. Management of opioid pharmacotherapy 18 14. -

Development of Pain-Free Methods for Analyzing 231 Multiclass Drugs and Metabolites by LC-MS/MS
Clinical, Forensic & Toxicology Article “The Big Pain”: Development of Pain-Free Methods for Analyzing 231 Multiclass Drugs and Metabolites by LC-MS/MS By Sharon Lupo As the use of prescription and nonprescription drugs grows, the need for fast, accurate, and comprehensive methods is also rapidly increasing. Historically, drug testing has focused on forensic applications such as cause of death determinations or the detection of drug use in specific populations (military, workplace, probation/parole, sports doping). However, modern drug testing has expanded well into the clinical arena with a growing list of target analytes and testing purposes. Clinicians often request the analysis of large panels of drugs and metabolites that can be used to ensure compliance with prescribed pain medication regimens and to detect abuse or diversion of medications. With prescription drug abuse reaching epidemic levels [1], demand is growing for analytical methods that can ensure accurate results for comprehensive drug lists with reasonable analysis times. LC-MS/MS is an excellent technique for this work because it offers greater sensitivity and specificity than immunoassay and—with a highly selective and retentive Raptor™ Biphenyl column—can provide definitive results for a wide range of compounds. Typically, forensic and pain management drug testing consists of an initial screening analysis, which is qualitative, quick, and requires only minimal sample preparation. Samples that test positive during screening are then subjected to a quantitative confirmatory analysis. Whereas screening assays may cover a broad list of compounds and are generally less sensitive and specific, confirmation testing provides fast, targeted analysis using chromatographic conditions that are optimized for specific panels. -

Effects of Prophylactic Ketamine and Pethidine to Control Postanesthetic Shivering: a Comparative Study
Biomedical Research and Therapy, 5(12):2898-2903 Original Research Effects of prophylactic ketamine and pethidine to control postanesthetic shivering: A comparative study Masoum Khoshfetrat1, Ali Rosom Jalali2, Gholamreza Komeili3, Aliakbar Keykha4;∗ ABSTRACT Background: Shivering is an undesirable complication following general anesthesia and spinal anesthesia, whose early control can reduce postoperative metabolic and respiratory complications. Therefore, this study aims to compare the effects of prophylactic injection of ketamine and pethi- dine on postoperative shivering.Methods: This double-blind clinical trial was performed on 105 patients with short-term orthopedic and ENT surgery. The patients were randomly divided into three groups; 20 minutes before the end of the surgery, 0.4 mg/kg of pethidine was injected to the first group, 0.5 mg/kg of ketamine was injected to the second group, and normal saline was injected to the third group. After the surgery, the tympanic membrane temperature was measured at 0, 10, 20, and 30 minutes. The shivering was also measured by a four-point grading from zero (no shiv- ering) to four (severe shivering). Data were analyzed by one-way ANOVA, Kruskal Wallis, Chi-square 1Doctor of Medicine (MD), Fellow of and Pearson correlation. Results: The mean age of patients was 35.811.45 years in the ketamine Critical Care Medicine (FCCM), group, 34.811.64 years in the normal saline group, and 33.1110.5 years in the pethidine group. Department of Anesthesiology and The one-way ANOVA showed no significant difference in the mean age between the three groups Critical Care, Khatam-Al-Anbiya (P=0.645). -

The In¯Uence of Medication on Erectile Function
International Journal of Impotence Research (1997) 9, 17±26 ß 1997 Stockton Press All rights reserved 0955-9930/97 $12.00 The in¯uence of medication on erectile function W Meinhardt1, RF Kropman2, P Vermeij3, AAB Lycklama aÁ Nijeholt4 and J Zwartendijk4 1Department of Urology, Netherlands Cancer Institute/Antoni van Leeuwenhoek Hospital, Plesmanlaan 121, 1066 CX Amsterdam, The Netherlands; 2Department of Urology, Leyenburg Hospital, Leyweg 275, 2545 CH The Hague, The Netherlands; 3Pharmacy; and 4Department of Urology, Leiden University Hospital, P.O. Box 9600, 2300 RC Leiden, The Netherlands Keywords: impotence; side-effect; antipsychotic; antihypertensive; physiology; erectile function Introduction stopped their antihypertensive treatment over a ®ve year period, because of side-effects on sexual function.5 In the drug registration procedures sexual Several physiological mechanisms are involved in function is not a major issue. This means that erectile function. A negative in¯uence of prescrip- knowledge of the problem is mainly dependent on tion-drugs on these mechanisms will not always case reports and the lists from side effect registries.6±8 come to the attention of the clinician, whereas a Another way of looking at the problem is drug causing priapism will rarely escape the atten- combining available data on mechanisms of action tion. of drugs with the knowledge of the physiological When erectile function is in¯uenced in a negative mechanisms involved in erectile function. The way compensation may occur. For example, age- advantage of this approach is that remedies may related penile sensory disorders may be compen- evolve from it. sated for by extra stimulation.1 Diminished in¯ux of In this paper we will discuss the subject in the blood will lead to a slower onset of the erection, but following order: may be accepted. -

Information to Users
The direct and modulatory antinociceptive actions of endogenous and exogenous opioid delta agonists Item Type text; Dissertation-Reproduction (electronic) Authors Vanderah, Todd William. Publisher The University of Arizona. Rights Copyright © is held by the author. Digital access to this material is made possible by the University Libraries, University of Arizona. Further transmission, reproduction or presentation (such as public display or performance) of protected items is prohibited except with permission of the author. Download date 04/10/2021 00:14:57 Link to Item http://hdl.handle.net/10150/187190 INFORMATION TO USERS This ~uscript }las been reproduced from the microfilm master. UMI films the text directly from the original or copy submitted. Thus, some thesis and dissertation copies are in typewriter face, while others may be from any type of computer printer. The quality of this reproduction is dependent upon the quality of the copy submitted. Broken or indistinct print, colored or poor quality illustrations and photographs, print bleedthrough, substandard margins, and improper alignment can adversely affect reproduction. In the unlikely. event that the author did not send UMI a complete mannscript and there are missing pages, these will be noted Also, if unauthorized copyright material had to be removed, a note will indicate the deletion. Oversize materials (e.g., maps, drawings, charts) are reproduced by sectioning the original, beginnjng at the upper left-hand comer and contimJing from left to right in equal sections with small overlaps. Each original is also photographed in one exposure and is included in reduced form at the back of the book. Photographs included in the original manuscript have been reproduced xerographically in this copy. -

Prescription Regulations Summary Chart Who Hold an Approval to Prescribe Methadone from Their
Products included in the Triplicate Prescription Program* This is a reference list provided for convenience. While all generic medication names appear, only sample brand names are provided and it should not be viewed as an all-inclusive listing of all trade names of drugs included in the Triplicate Prescription Program. BUPRENORPHINE METHADONE BuTrans, Suboxone** Metadol, Methadose - May only be prescribed by physicians Prescription regulations summary chart who hold an approval to prescribe methadone from their BUTALBITAL PREPARATIONS provincial regulatory body*** Summary of federal and provincial laws governing prescription drug ordering, Fiorinal, Fiorinal C ¼ & C ½, Pronal, Ratio-Tecnal, records, prescription requirements, and refills Ratio-Tecnal C ¼ & C ½, Trianal, Trianal C ½ METHYLPHENIDATE Biphentin®, Foquest®, and Concerta® brands are excluded Revised 2019 BUTORPHANOL from TPP prescr ip t i o n p a d req u ir e m e n t s (generic versions Butorphanol NS, PMS-Butorphanol, Torbutrol (Vet), of these products require a triplicate presc ription) Torbugesic (Vet) Apo-Methyphenidate, PHL-Methylphenidate, PMS- Prescription regulations DEXTROPROPOXYPHENE Methylphenidate, PMS-Methylphenidate ER, Ratio- None identified Methylphenidate, Ritalin, Ritalin SR, Sandoz- According to the Standards of Practice for Pharmacists and Pharmacy Technicians: Methylphenidate SR, Teva-Methylphenidate ER-C FENTANYL/SUFENTANIL/ALFENTANIL 6.4 Neither a pharmacist nor a pharmacy technician may dispense a drug or blood product under a Alfentanil Injection, -

Kappa Opioid Receptor Regulation of Erk1/2 Map Kinase Signaling Cascade
1 KAPPA OPIOID RECEPTOR REGULATION OF ERK1/2 MAP KINASE SIGNALING CASCADE: MOLECULAR MECHANISMS MODULATING COCAINE REWARD A dissertation presented by Khampaseuth Rasakham to The Department of Psychology In partial fulfillment of the requirements for the degree of Doctor of Philosophy in the field of Psychology Northeastern University Boston, Massachusetts August, 2008 2 KAPPA OPIOID RECEPTOR REGULATION OF ERK1/2 MAP KINASE SIGNALING CASCADE: MOLECULAR MECHANISMS MODULATING COCAINE REWARD by Khampaseuth Rasakham ABSTRACT OF DISSERTATION Submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in Psychology in the Graduate School of Arts and Sciences of Northeastern University, August, 2008 3 ABSTRACT Activation of the Kappa Opioid Receptor (KOR) modulates dopamine (DA) signaling, and Extracellular Regulated Kinase (ERK) Mitogen-Activated Protein (MAP) kinase activity, thereby potentially regulating the rewarding effects of cocaine. The central hypothesis to be tested is that the time-and drug-dependent KOR-mediated regulation of ERK1/2 MAP kinase activity occurs via distinct molecular mechanisms, which in turn may determine the modulation (suppression or potentiation) by KOR effects on cocaine conditioned place preference (CPP). Three studies were performed to test this hypothesis. Study 1 examined the effects of U50,488 and salvinorin A on cocaine reward. In these studies, mice were treated with equianalgesic doses of agonist from 15 to 360 min prior to daily saline or cocaine place conditioning. At time points corresponding with peak biological activity, both agonists produced saline-conditioned place aversion and suppressed cocaine-CPP, effects blocked by the KOR antagonist nor-BNI. However, when mice were place conditioned with cocaine 90 min after agonist pretreatment, U50,488-pretreated mice demonstrated a 2.5-fold potentiation of cocaine-CPP, whereas salvinorin A-pretreated mice demonstrated normal cocaine-CPP responses.